Cardiac pathologies are represented by a large category of diagnoses. They are reflected in the international classifier and are used by practicing doctors to describe specific situations.
However, this condition is not considered an independent diagnosis, nor is it recognized as a full-fledged disease. What are we talking about in this case?
Short PQ syndrome is an acceleration of the transmission of bioelectric impulses from the sinus node to the ventricles. This abnormality is a finding on electrocardiography, but not a separate pathological condition.
The indicator can deviate in two directions, relatively speaking:
- Shortening or CLC Clerk-Levy-Christesco syndrome or SVC (Wolf-Parkinson-White) - a decrease in the period of impulse conduction to the ventricles.
Indicates the presence of additional beams that provide inadequately fast signal movement. Usually against the background of congenital pathologies.
- An increase in time indicates the opposite phenomenon, that is, a decrease in the quality of the signal.
Symptoms are not always present, and treatment is not required in all cases. You need to proceed from the specific situation.
Mechanism of development of deviation
The development of the syndrome is based on a congenital disorder of the structures of the cardiovascular system.
Ontogenesis of the fetus is accompanied by defects spontaneously, as a result of the influence of negative environmental factors on the body of the expectant mother or as a result of chromosomal abnormalities.
The syndrome can be detected both in the early period of a child’s life, even in infancy, and much later.
The problem does not always make itself known with symptoms at the beginning. Perhaps a sluggish, latent course over the course of many years.
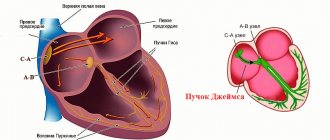
The essence of the deviation is always approximately the same in children and adults. Electrical impulses from the natural pacemaker (sinus node) are transmitted through special fibers to the atrioventricular node, where a slight delay occurs, then the signal along the His bundle is sent to the ventricles.
It is possible to develop additional pathways (Maheim or Kent in WPW syndrome, and James in CLC disorder).
In this case, there is a risk of an increase in the number of heartbeats per minute and the development of spontaneous paroxysmal tachycardia. It can provoke cardiac arrest and death of the patient; it is a dangerous form of arrhythmia.
The clinical picture is not always bright and pronounced. Yes, and not in all cases it is clearly present.
Up to a certain point, the body can compensate for the disorder. Then dysfunction comes. Then the symptoms will make themselves known.
Without treatment, the likelihood of organic changes in the structure of the myocardium, cardiac arrest and death of the patient in this regard gradually increases.
No doctor will undertake to assess the probability, the prognosis is vague, the course is unpredictable. This can happen in a month, a year or more.
If the PQ interval is shortened, the ECG reveals paroxysmal, dangerous tachycardia.
Pathogenesis
Histologically, additional conduction pathways appear as thin filaments located in the working atrial myocardium. The filaments connect the myocardium of the atria and ventricles through the atrioventricular groove, bypassing the structure of the normal conduction system of the heart.
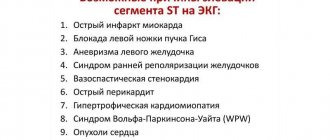
With WPW syndrome, excitation of part or all of the ventricular myocardium occurs earlier than when impulses pass through the standard route through the branches and bundles of His, through the atrioventricular node. On the electrocardiogram, ventricular preexcitation is reflected in the form of a delta wave - an additional wave of depolarization. At the same time, the width of the QRS complex increases, the PQ interval shortens.
The collision of the main depolarization wave and the additional delta wave leads to the formation of a confluent QRS complex, which becomes widened and distorted. After atypical excitation of the ventricles, the sequence of repolarization processes is disrupted, which leads to the formation of a discordant QRS complex on the ECG. This changes the polarity of the T wave and shifts the RS-T segment.
The formation of a circular wave of excitation (re-entry) leads to rhythm disturbances such as atrial fibrillation and flutter , paroxysmal supraventricular tachycardia . In this case, the impulse moves in the anterograde direction along the AV node from the atria to the ventricles, and along additional pathways in the retrograde direction - from the ventricles to the atria.
The difference between a syndrome and a phenomenon
The line between these two concepts is quite thin, at least for a patient who does not have deep medical knowledge. In both cases we are talking about findings obtained during electrocardiography.
The syndrome is a combination of two things:
- The first is the presence of a pronounced change in the ECG results. Shortening or lengthening does not matter in this context.
- The second mandatory point is the presence of a clinical picture. It indicates the onset of decompensation and the presence of the disease.
The phenomenon of shortened PQ is represented only by changes in electrocardiography. There are no symptoms or clinical picture. Therefore, the condition in question is not a pathological process. At least until a certain point.
As has been said, there is a fine line. The phenomenon can become a syndrome. On the contrary, such a connection does not work.
The use of such terminology often confuses patients. To clarify what exactly is happening, it is recommended to contact a cardiologist to clarify the disorder and interpret the electrocardiogram.
WPW syndrome during pregnancy
The clinically silent syndrome does not require specific treatment. However, during pregnancy , WPW syndrome can manifest itself as paroxysmal rhythm disturbances, which requires timely consultation with a cardiologist to select effective therapy.
With frequent attacks of tachycardia against the background of diagnosed WPW syndrome, pregnancy is contraindicated. This precaution is associated with the risk of developing life-threatening arrhythmias. With tachycardia, blood circulation in organs and tissues is disrupted, which negatively affects not only the condition of the mother, but also the development of the fetus.
Symptoms
The clinical picture depends on the specific disease, its severity, age, gender, lifestyle and many other factors.
As noted earlier, a short PQ interval is not a diagnosis. This is just an objective indicator on the cardiogram.
The changes are represented by two disorders, which are reflected in the international classifier.
This is Wolff-Parkinson-White (or WPV, for short) or Clerk-Levy-Christesco (CLC) syndrome. Both are of an innate nature, but may not appear immediately, but over a period of time.
There are three age peaks: the first occurs during infancy, the second during puberty, from 13 to 18 years. The latter is determined by 40-50 years.
With the development of Wolff-Parkinson-White syndrome, we are talking about a typical clinic:
- Increased heart rate. Tachycardia persists throughout the entire period of the pathological process, manifested by paroxysms, rare or frequent attacks. Heart rate can reach 200-300 beats. These are not full-fledged contractions, but individual movements of the myocardium; they are recorded only with the help of electrocardiography. Subjectively, they are felt as an uneven beat with an increased heart rate.
- Sweating. Hyperhidrosis. Regardless of physical activity. Develops due to activation of the autonomic nervous system. May be part of the collaptoid reaction or precede it.
- Dyspnea. Against the background of rest at the moment of paroxysm (attack). Then everything fades away until the next abnormal episode, and so on in a circle, until specific treatment is started.
- Pale, bluish skin.
- Panic attacks. Accompanied by a feeling of strong inexplicable fear in the patient. May be associated with motor agitation.
- Pain in the chest area. Cardiac discomfort has a pressing, burning character. This is a direct indication of a malnutrition of tissues, their probable destruction, which can end in failure (coronary insufficiency, ischemic heart disease and other “delights”).
- Fainting. Syncope. They do not occur in all cases, but this is possible. More common in children. Indicates insufficient nutrition of the brain. They may be accompanied by pain in the back of the head, temples (cephalalgia), diffuse discomfort, and disorientation in space.
Clerk-Levy-Christesco syndrome is accompanied by slightly different symptoms. Although the origin of the pathological process is similar.
There are no fundamental differences observed in the clinic. Chest pain, tachycardia, shortness of breath, nausea, loss of consciousness and other phenomena are also detected.
The key point is the length of the episode. Against the background of CLC syndrome, the duration is minimal, no more than 10-15 minutes. ERV can last for several hours.
In general, the disease (Clerk-Levi-Christesco) has a latent but dangerous course. Because it more often provokes supraventricular paroxysmal tachycardia and death of the patient in the early years.
It is possible to differentiate the two diagnoses only by ECG results.
How does short PQ syndrome manifest?
The clinical picture of shortened PQ syndrome is caused by the occurrence of paroxysmal tachycardia, since during the interictal period the patient usually does not present any complaints from the cardiovascular system. Symptoms of tachycardia are the following:
- The sudden, sharp onset of an attack, caused by provoking factors or occurring without them, in itself,
- Feeling of a strong heartbeat, sometimes with a feeling of interruptions in the heart,
- Autonomic manifestations - severe weakness, hyperemia or paleness of the face, sweating, coldness of the extremities, fear of death,
- Feeling of suffocation or lack of oxygen, feeling of insufficient inspiration,
- Unpleasant discomfort in the heart area of a pressing or burning nature.
If the symptoms described above appear, you should definitely seek medical help by calling an ambulance or going to a clinic.
Flow options
In all cases, several variants of the clinical course of the disease are described.
- Hidden or asymptomatic type. Occurs in 40% of patients. It is not necessary that pathology always moves in this way. Transformation into other forms is possible. Usually, as the disorder progresses and the condition decompensates.
- Light type. Paroxysms develop once every month or two, or less often. Lasts from 5 to 15 minutes, goes away completely without any traces, on its own.
- Moderate in severity. Episodes of varying frequency, not necessarily regular. Accompanied by a persistent increase in the number of heart contractions and poor health. Duration is 2-4 hours, sometimes longer. Independent complete regression is almost never observed; the use of drugs or the use of electrocardioversion is required to interrupt the paroxysm.
- A severe form of shortening of the PQ interval is accompanied by a pronounced disturbance: the attack continues indefinitely. Additionally, ventricular fibrillation, or atrial flutter, is detected. The probability of death is maximum; urgent hospitalization is required.
The clinical picture is almost always the same. But it is nonspecific, which does not allow doctors to say unambiguously about the origin.
Forecast
The prognosis for this disease is usually favorable, especially if it is asymptomatic. However, in people with a family history, deaths are possible. The exception is athletes and test pilots. They fall into the category of professional risk.
If patients have cardiac complaints, their prognosis is somewhat worse. But modern treatments can reduce the risk of fatal complications. In any case, there is no need to panic. It is better to contact a competent specialist who can make the correct diagnosis and prescribe effective treatment.
Source: FB.ru
https://www.baby.ru/blogs/post/322258155-269443768/ here is my story about childbirth, if you are interested, read it) there are a lot of letters.
I only paid for signing the exchange, then another 700 UAH. I gave birth with the team on duty as a matter of principle. I don't think it's necessary to overpay. I wanted to thank the doctor of my own free will. And so it happened.
I gave the doctor 500 UAH after giving birth (or it was the midwife, I don’t know). I also wanted to give it to the second doctor who helped me give birth, but he left by the time I came out of anesthesia. 100 UAH to the nurse, and upon discharge, 100 UAH to the children's nurse. Well, some people bought medicine there themselves; I needed IVs.
The doctor to whom I gave 500 UAH said that if we can afford to thank him, it would be nice, but if we are in a difficult financial situation, just a sincere thank you will be enough. And he will not be offended by us if he does not receive material gratitude from us. Just like that. I am incredibly glad that I ended up with them, and gave birth in the 7th maternity hospital. And they said that they were waiting for me next time) So that I would come to them for the second one. And that's exactly what I'll do)
Partner births are generally the default there. When I signed the exchange, they immediately wrote to me that there would be partnerships, without even asking me anything.
The room is super comfortable. For 2 blocks. Toilet and shower for me and the neighbor. Everything is clean, odorless, neat. Comfortable. The children's nurse comes running on the first call. They feed you a lot) But not homemade food, of course. And they feed it like 2 times a day... I don’t remember. In any case, you need to have your own food with you) Visits are free... from 8 a.m. to 7 p.m., apparently. My mother was constantly sitting with me, my friends, husband, future godmothers came) I was not bored, I could sleep, eat in peace, and wash. I sent you the photos)
I was registered in the residential complex at the 5th maternity hospital. And for certain reasons, I had to be inside there. In the pathology department.
In the reception department I came across an outright boor. He spoke very rudely to pregnant girls... VERY rudely! and was rude to me personally. When I was afraid that he would examine me in the chair, he answered me, saying, why did I even think that he would climb into me there? Like for 300 years he needs to go to someone there and look at something there. And in general, all of us who are pregnant are incredibly stupid. At that time I was still slightly thinking about the choice between the 5th and 7th maternity hospital, but after the rudeness in the reception area, I finally decided that only the 7th.
The maternity hospital itself is beautiful, clean, and neatly renovated. The staff in the maternity hospital itself is good, I liked it... However, the nurses are somehow not very good. But the head of pathology (if I’m not mistaken) is a very pleasant man. So kind and soft. Talked very nicely to pregnant women)
I would recommend you the 7th maternity hospital, to be honest)
Source: www.baby.ru
Causes
Factors in the development of a shortened interval are always intrauterine. That is, the disorder or predisposition to it occurs during the mother’s pregnancy.
There are already two options here:
- The first is a spontaneous violation in the 1st trimester. When the cardiovascular system is formed. This is the main reason.
- The second is chromosomal disorders, genetic mutations (extremely rare).
Then everything depends on the case. An anatomical defect does not always manifest itself immediately after birth.
A child can live for years and seem healthy until a certain point. As long as the body copes, everything is fine. And then a trigger factor is required that will lead to dysfunction and tip the scale in the other direction.
Among them:
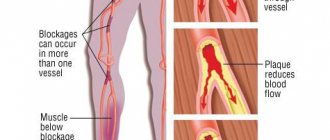
- Drinking alcohol, smoking, drug addiction. Cocaine, heroin, and, to a lesser extent, amphetamine are particularly dangerous in this regard.
- Constant use of caffeine.
- Insufficient sleep.
- Frequent stress, physical overload. That is, moments that provoke an increase in the synthesis of cortisol, adrenaline, and adrenal hormones.
- Using medications without a doctor's prescription. Especially anti-inflammatory drugs.
- A history of hypertension, diabetes mellitus, and endocrine disorders.
The list is incomplete. There is also an increased risk in the early years (up to 3 years), during puberty and in later life. It is necessary to carefully monitor patients from risk groups.
Classification
There are 4 clinical forms of WPW syndrome:
- Manifesting form. Characterized by the presence of a constant delta wave, which is recorded in 0.15-0.20% of the general population. Retrograde and antegrade conduction along additional pathways is recorded.
- Intermittent form. Characterized by transient signs of pre-excitation, most often detected by clinical data.
- Latent form . Signs of pre-excitation are recorded only when the atria (mainly the left atrium) are stimulated through the coronary sinus during an invasive EPI (electrophysiological study). There may be a slowdown in the conduction of impulses through the AV node during massage of the carotid sinus or administration of Propranolol , Verapamil .
- Hidden form. Only retrograde atrial preexcitation is characteristic. Paroxysms of atrial fibrillation and antidromic tachycardia conducted through additional conduction pathways are not observed. An ECG in sinus rhythm shows no signs of WPW syndrome.
There are 3 stages of the disease:
- I – short-term attacks (lasting less than half an hour) of orthodromic tachycardia. The attacks are stopped reflexively.
- II – the frequency and duration of attacks increases (from half an hour to 3 hours). The attacks are stopped by taking one antiarrhythmic drug together with the use of vagal tests. To prevent the onset of paroxysmal tachycardia, drug therapy is used.
- III – frequent attacks of orthodromic tachycardia, lasting more than 3 hours.
Attacks of atrial or ventricular fibrillation and attacks of ventricular tachycardia are recorded. Disorders of the conduction system of the heart appear in the form of bundle branch blocks, sick sinus syndrome , and anti-ventricular blockades. Resistance to antiarrhythmic drugs is noted.
There are several anatomical variants of the syndrome, taking into account the morphological substrate:
Syndrome with accessory muscle atrioventricular fibers:
- passing through the fibrous junction from the aortic to the mitral valve;
- passing through the accessory parietal atrioventricular junction (left or right);
- associated with an aneurysm of the middle vein of the heart or sinus of Valsalva;
- coming from the atrial appendage (right or left);
- running along paraseptal, septal, inferior or superior fibers.
Syndrome with Kent's bundles (specialized muscle atrioventricular fibers). The bundles are formed from rudimentary tissue similar to the structure of the AV node:
- entering the myocardium of the right ventricle;
- entering the right bundle branch (atrio-fascicular).
Diagnostics
The basis of the examination is electrocardiography. This is the gold standard for assessing the conditions in question.
A typical picture that is revealed during the instrumental technique:
- Negative T wave.
- Widening of the QRS complex, which corresponds to a decrease in the efficiency of myocardial contraction with formal excessive excitation of cardiac structures.
- ST region depression. Again, it speaks of dysfunctional disorders, ineffectiveness of the muscle organ.
- A delta wave is necessarily detected. Normally it shouldn't be there. It is noted with early excitation of the ventricles. Before full systole (contraction). The intensity of this indicator can be used to judge the severity of the pathological process. The larger the delta wave, the worse the situation is at the moment.
- PQ interval is shorter than 0.12 sec.
The characteristics under consideration are not always present in full. Then we can talk about a truncated disorder.
The clinical picture also does not develop in 100% of situations, even against the background of the presence of a “set” of deviations on the graph. In this case, they talk about the phenomenon of shortened PQ.
But the diagnosis cannot be dismissed out of hand. To say that the disorder is relatively safe, you need to monitor the patient for at least a couple of weeks.
Other studies are used less frequently; they do not provide the necessary information, because there are no organic pathologies that provoke the condition in question.
Basically, a consultation with a cardiologist, interviewing the patient or his parents about complaints, and collecting an anamnesis are required. In order to establish a probable trigger factor, develop treatment tactics, and secondary prevention aimed at preventing relapses.
There is no fundamental difference in who has deviations from the norm. A shortened PQ interval in adults and children suggests the same thing.
An adjustment is made only for the person’s age in order to determine the normal heart rate (in young patients the rate is initially higher, in infancy it is significantly higher).
Why does CLC syndrome form?
In order for a patient to have shortened PQ syndrome, it is necessary to have additional bundles that conduct electrical impulses. The formation of such bundles occurs even at the stage of fetal development in the womb.
In childhood, shortened PQ syndrome is recorded in both infants and adolescents, as the body develops rapidly, but not always. Symptoms may not appear throughout life, being determined only by the results of the cardiogram.
| Diseases that provoke paroxysmal tachycardia | Factors provoking paroxysmal tachycardia |
| · Myocardial infarction; | · Experienced stressful situations and emotional stress ; |
| · Congenital heart defects ; | · Physical activity that is unusual for the patient is higher than normal; |
| · Hypertrophic cardiomyopathy (a disease characterized by thickening of the wall of the left and/or right ventricles); | · Visited the sauna or steam bath the day before; |
| · Myocarditis (inflammation of the heart muscle, provoked by infectious diseases, toxins and allergic reactions). | · Sudden change in temperature, as an example when leaving a warm room into the cold; |
| · Hypertensive crisis (an emergency condition provoked by a strong increase in blood pressure, which can pose a threat to life in human organs); | |
| · Increased pressure inside the abdomen (with severe coughing, defecation, labor, sudden lifting of heavy objects); | |
| · Eating too much food at one time; | |
| · Drinking excessively hot or cold liquids; | |
| · Sometimes with the use of sedatives and beta blockers, which may affect short PQ syndrome. |
All of the above reasons are not guaranteed, but can probably affect the appearance of short PQ syndrome. These factors should be avoided, if possible, so as not to put yourself at risk.
Treatment
Treatment methods are conservative and surgical. Before resorting to radical measures, drug correction is carried out.
Two pharmaceutical groups are used:
- Beta blockers. Mainly Anaprilin, less often others. Allows you to stop pathological excitation in the tissues of the heart.
- Antiarrhythmic. Procainamide, Propafenone. With great care so as not to make things worse.
Attention:
Calcium antagonists and ATP agents should not be used. So as not to provoke cardiac arrest.
As part of urgent symptomatic care, doctors resort to electrocardioversion. Passing current for a fraction of a second to restore normal heart rate.
This is an emergency measure aimed at saving the patient’s life and improving well-being.
Surgery is required in extreme cases. That is, almost always, oddly enough. It is impossible to correct an organic disorder with tablets.
The method is identical - radiofrequency ablation. This is a minimally invasive intervention, it consists of introducing a special miniature emitter into the cardiac structures and destroying the abnormal conduction pathway using a bloodless method.
The procedure is painless and causes virtually no discomfort.
In the future, everything should return to normal without any additional measures. Unless the disease provokes other anatomical changes in the heart and brain.
Prevention
Patients with CLC syndrome generally do not require specific preventive measures. Especially if he had not shown himself in any way before. But in case of discomfort, such as pain, shortness of breath, dizziness or fainting, you should contact your local physician. There are general methods for preventing all diseases of the cardiovascular system:
- changing your lifestyle to a more active one;
- weight loss;
- rational diet;
- giving up bad habits: smoking and drinking alcohol;
- reducing the consumption of table salt;
- sleep at least eight hours a day.
There is probably no need to remind you that it is necessary to reduce the number of stressful situations and increase the time of walking in the fresh air.
Prognosis and complications
The outcome in 95% of cases, subject to treatment, is favorable.
Without therapy it is always negative. The result is severe disability or death of the patient over the course of several years. And it happens even faster.
It is impossible to accurately predict when the fateful hour will come. Fairly said for an asymptomatic and bright course.
Among the consequences of CLC or SVC syndromes are heart attack (acute malnutrition of cardiac structures), cardiac arrest, also called asystole, stroke (death of nerve fibers as a result of poor nutrition).
The logical end is the death of a person.
How is it diagnosed?
The main method by which shortened PQ is diagnosed is an electrocardiogram (ECG).
The results of the heart examination indicate the main signs of the syndrome:
- The frequency of contraction of the heart muscle is higher than normal, with a range of 120 to 200 beats in 60 seconds;
- Direct shortening of the PQ interval (less than 0.11 seconds);
- The ventricular complexes are normal in case of supraventricular tachycardia, and expand in the case of ventricular tachycardia, which directly threatens human life;
- With supraventricular tachycardia, sinus rhythm is correct.
These include:
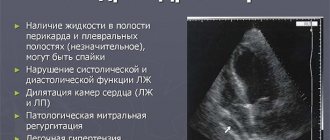
- Ultrasound examination of the heart;
- Ultrasound of the heart during the day;
- Bicycle ergometry. Carrying out an electrocardiogram after physical activity using a special device;
- Transesophageal electrophysiological study (TEPE) is carried out by electrically influencing the myocardium by inserting a probe into the esophagus;
- Intravascular electrophysiological study. Used in especially rare cases;
- Magnetocardiography. This research method allows you to fully evaluate the activity of the heart muscle.
The use of certain hardware tests is prescribed by the attending physician, depending on the patient’s complaints and symptoms.
Medical therapy
If the syndrome is asymptomatic, treatment is usually only applied to individuals with a family history of sudden death. Also, patients who require treatment include athletes and people in dangerous professions associated with excessive stress. If paroxysms of supraventricular tachycardia are present, therapeutic therapy is used, the effect of which is to eliminate attacks and prevent them with the help of a variety of medications. Physiotherapy may be used.
An important indicator is the nature of the arrhythmia: orthodromic, antidromic, AF. You should also pay attention to its subjective and objective tolerability, ventricular contraction frequency and the presence of concomitant heart diseases.
Adenosine is considered the main drug used in treatment
The main drug used for treatment is Adenosine. A side effect is a transient increase in atrial excitability. The next drug of choice is Verapamil, and the group of β-blockers acts as a second-line drug.
If we talk about non-drug methods, then we are talking about transthoracic depolarization and atrial pacing. In exceptional cases, a decision is made to surgically destroy the accessory tracts. Surgical treatment is resorted to if it is impossible to carry out any other treatment methods, or if they are unsuccessful. This decision is also made if it is necessary to perform open heart surgery to eliminate a concomitant disease.
How to provide first aid during an attack?
In case of constantly recurring relapses of accelerated heartbeat, you should know the following algorithm of actions:
- Massage the area where the carotid artery branches. This will lead to normalization of heart contractions;
- Gently massage the eyeballs;
- To alleviate the patient's condition, you can lower your face into cool water while holding your breath. Use no more than 10 minutes;
- Take a deep breath, strain, hold your breath, exhale slowly;
- Do several squats, tensing your whole body.
Symptoms of paroxysmal tachycardia
Example of shortening PQ to 0.03 s
The manifestation of symptoms of shortened PQ syndrome is possible in any age category. Over a long period of time, the disease may not show signs. With the CLC phenomenon, the electrocardiogram shows a shortening of PQ. But the patient does not show any obvious symptoms, and he does not feel any burden.
Manifestations of shortened PQ are considered based on the symptoms of such tachycardia.
It is expressed in the following signs:
- Heavy breathing, lack of oxygen, inability to breathe fully;
- Painful sensations in the heart area, characterized by a squeezing and burning nature of the manifestation;
- The attack begins suddenly, after experiencing provoking factors;
- The presence of an increased heart rate, rarely with sensations of an unstable pulse;
- Sudden feeling of weakness;
- Pale complexion;
- Increased sweating;
- Cold upper and lower extremities;
- Anxiety, fear of dying.
Symptoms develop periodically and are in the nature of attacks. In the intervals between them, the patient feels as usual and does not experience any abnormal sensations.
In the presence of provoking factors, the following symptoms may appear:
- attacks develop suddenly, for no apparent reason;
- a person feels a strong heartbeat that causes him discomfort;
- severe weakness and fatigue appear;
- sweat appears on the skin;
- limbs cool;
- the skin on the face either turns red or turns pale;
- the patient experiences a feeling of lack of oxygen, which may be accompanied by a fear of death;
- There is a burning sensation in the heart area, a feeling of constriction in the sternum.
If short PQ syndrome is considered pathological, then the patient experiences attacks of rapid heartbeat that last from ten to twenty seconds. They go away on their own and do not require drug intervention. Most often, such paroxysms are associated with stress, overwork, and excessive physical activity. But, as a rule, the reason remains unknown.
A sudden increase in heart rate can cause patients to have panic attacks, a feeling of discomfort in the chest area, pallor and perspiration. But sometimes patients do not even suspect that they have a heart pathology. The PQ interval on the cardiogram is counted from the beginning of the P wave to the beginning of the Q wave. Normally, this indicator ranges from one hundred twenty to two hundred milliseconds.