Dressler syndrome (DS) is one of the complications of myocardial infarction, manifested by inflammation of the pericardium, pulmonary pleura, lungs, joints, increased body temperature, the content of markers of the inflammatory process, another name is post-infarction syndrome.
The prevalence of the disease, according to various sources, ranges from 4 to 30% (1,2). In recent years, this figure has decreased significantly. The trend towards a decrease in the prevalence of the syndrome is explained by more effective, comprehensive treatment.
Let's consider the mechanism of development of post-infarction syndrome, its causes, symptoms, methods of diagnosis, treatment, prevention, possible complications, prognosis.
Causes
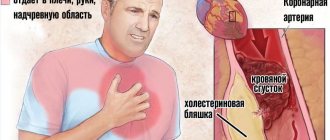
The initial cause of Dressler syndrome in cardiology is ischemic damage to the structural fibers of the heart muscle, which leads to the death of cardiomyocytes. In most cases, it develops with a complicated large-focal infarction. During the destruction of necrotic tissue, denatured proteins begin to enter the bloodstream. The immune system, in turn, reacts to them as if they were foreign. As a result, an autoimmune reaction occurs, which is the cause of the development of post-infarction syndrome.
Blood antigens, which penetrate into the pericardial membrane in the process of violating the integrity of the myocardium, have a certain significance in the formation of the symptom complex of this complication of a heart attack. Therefore, in addition to the acute stage, the trigger mechanism for the formation of the disease can be hemopericardium, characterized by hemorrhage into the pericardial cavity. In addition, this condition can be caused by chest injuries, heart injuries, or inadequate heart surgery. Also at risk are post-infarction patients with autoimmune pathologies. Some doctors believe that the development of the inflammatory process is caused by a viral infection. However, cardiologists do not yet have a clear answer on this issue.
Treatment
Dressler's syndrome in cardiology is a dangerous condition. His treatment is carried out in a hospital setting if this is the first case. Relapses are treated on an outpatient basis when the disease is mild.
In most cases, therapy is carried out with non-steroidal anti-inflammatory drugs. If they do not help, then hormonal drugs are prescribed.
Anticoagulants are not used for the syndrome, but when they are needed, small doses may be prescribed.
Glucocorticosteroid hormones are effective in combating the problem in the form of:
- Dexamethasone. It is used for injection. The main active ingredient is dexamethasone sodium phosphate. The drug has many contraindications, including pregnancy, pathologies of the digestive system, viral diseases and infections.
- Prednisone. The medicine provides antiallergic, anti-inflammatory and immunosuppressive effects. The dosage is determined separately for each case.
As for NSAIDs, therapy is usually carried out using:
- Diclofenac. the drug eliminates inflammation, relieves painful symptoms, and reduces body temperature. To achieve this effect, you need to take one or two tablets per day.
- Indomethacin. It has analgesic, antipyretic and anti-inflammatory properties.
Sometimes the use of acetylsalicylic acid is necessary.
To eliminate complications, invasive techniques can be used:
- If cardiac tamponade occurs, fluid is pumped out from the pericardium. This is done using a thin tube equipped with a needle, which is inserted into this part of the heart and the accumulated exudate is pumped out. To perform the procedure, local anesthesia is required.
- The pericardium is removed. This is necessary if severe inflammation has led to the development of compressive pericarditis. This procedure is called pericardiectomy.
Modern therapeutic techniques and high-quality treatment of myocardial infarction have reduced the number of cases of Dressler syndrome.
Pathogenesis
Dressler's syndrome in cardiology is an autoimmune process that develops as a result of intensified production of antibodies to cardiac antigens. In this case, an acute disruption of the processes of blood flow into the myocardium and the death of its cells leads to resorption of necrosis zones and the release of denatured components into the bloodstream. This promotes the development of an immune response with the formation of autoantibodies, the action of which is directed against proteins present in the serous integument of target organs.
Immune antibodies to cardiomyocytes, present in large quantities in the plasma of post-infarction patients, form immune complexes containing cells of their own tissues. They circulate freely in the bloodstream, accumulate in the visceral, pericardial pleura and in the internal structures of the joint capsules, provoking an inflammatory process of an aseptic nature. In addition to this, the level of cytotoxic lymphocytes begins to increase, which destroy damaged cells in the body. Thus, the state of both humoral and cellular immunity is significantly impaired, which confirms the autoimmune nature of the symptom complex.
Varieties
Dressler's syndrome after myocardial infarction - what is it? This disease is divided into 3 forms. Within each of them there are also several subtypes, the classification of which is based on the localization of inflammation. So, Dressler syndrome happens:
1. Typical. Clinical manifestations of this form are associated with inflammation of the visceral pleura, pericardium and pulmonary tissue. It includes combined and single variants of autoimmune damage to connective tissues:
- pericardial - the parietal and visceral layers of the pericardial sac become inflamed;
- pneumonic - infiltrative disorders form in the lungs, leading to pneumonitis;
- pleural - the pleura becomes the target of antibodies, signs of hydrothorax develop;
- pericardial-pleural – symptoms of sensitization of the pleura and serous membrane of the pericardium are observed;
- pericardial-pneumonic – the pericardial membrane and lung tissue are affected;
- pleural-pericardial-pneumonic - inflammation moves from the cardiac sac to the pulmonary and pleural structures.
2. Atypical. This form is characterized by variants caused by antibody damage to joints and vascular tissues. It is accompanied by an inflammatory process in large articular joints or skin reactions: pectalgia, “shoulder syndrome,” erythema nodosum, dermatitis.
3. Low-symptomatic (erased). In this form with mild symptoms, fever, persistent arthralgia and changes in the composition of white blood are noted.
When diagnosing atypical and erased forms of the syndrome, some difficulties often arise, which determine the relevance of a more in-depth study of this disease.
Dressler syndrome in cardiology: causes, symptoms, treatment, prognosis
Dressler's syndrome is one of the complications of myocardial infarction. It is also called post-infarction syndrome. This is an autoimmune disease that develops within a month after an acute attack.
Development mechanism
The syndrome is based on autoimmune processes. The problem occurs in 30% of cases, and in recent years it has become more common under the influence of non-steroidal anti-inflammatory drugs and reperfusion techniques.
The disease develops as a result of extensive, extensive or complicated myocardial infarction. The pathology is based on autoimmune aggression, which causes a hyperergic reaction in the sensitized organism.
The syndrome occurs over a long period of time, with periods of exacerbations followed by remissions. This causes disturbances in the health and quality of life of the patient.
What are the different forms?
Taking into account combinations of lesions, the following forms of the syndrome are distinguished:
- Typical. When it occurs, the outer lining of the heart, lung tissue, and the lining of the chest are damaged. Various combinations may occur, for example, the pericardium and lining of the chest are damaged, and other variations are possible.
- Atypical. When autoimmune disorders develop in the synovial membranes of the joints and skin damage, manifested by rashes and redness.
- Asymptomatic. In this case, the pathology is accompanied by low-grade fever for a long time, an increase in the erythrocyte sedimentation rate, an increase in the level of eosinophils, and pain in the joints.
Diagnostic features
To determine Dressler's syndrome after a heart attack, you must:
- Collect the patient's medical history. The doctor asks for complaints, determines when the first signs appeared, and finds out whether there have been cases of similar pathologies in the family.
- Perform a physical examination. It consists of determining the color and appearance of the skin, analyzing breathing movements, measuring pressure in the arteries, listening to heart sounds and checking body temperature.
- Donate blood and urine for a general analysis. At the same time, the blood composition, cell level, erythrocyte sedimentation rate and other indicators are determined.
- Undergo a biochemical blood test. It will provide information about cholesterol and glucose levels.
- Undergo electrocardiography and echocardiography.
- Take an x-ray of the chest cavity.
- Undergo magnetic resonance imaging and CT scan
You may also need to consult a therapist.
Possible complications and prognosis
The occurrence of complications in the post-infarction period is very rare. In isolated cases, patients suffered from kidney pathologies in the form of glomerulonephritis and vascular diseases, such as hemorrhagic vasculitis.
In rare cases, if hormonal therapy has not been carried out, effusion pericarditis turns into an adhesive form. It complicates the process of relaxation of the heart muscle and causes congestion in the systemic circulation. This leads to the development of diastolic heart failure.
In post-infarction syndrome, relapses alternate with remissions. A weakening of the manifestations of the pathological process is observed during treatment, as soon as it is stopped, the condition worsens. Each relapse can last from a week to several months.
Dressler's syndrome is a complication that has a favorable prognosis. With this diagnosis, the patient is issued a sick leave certificate. It indicates that the person has lost capacity for work for a period of 3–3.5 months. If the condition does not improve, this period will be extended.
Persistent loss of ability to work and the assignment of a disability group to a patient are indicated when frequent relapses are observed and serious disturbances in the functioning of the cardiovascular system have occurred, which are associated not only with pathology, but also with myocardial infarction.
The syndrome itself cannot make a person disabled. But this does not mean that its manifestations should be ignored. You can't do without treatment.
Lifestyle adjustments
After myocardial infarction, a person’s usual activity and lifestyle are significantly limited. Therefore, it is necessary to make changes to your diet and daily routine to prevent relapse. The patient must:
- Avoid excessive physical activity. They increase the work of the heart, and due to post-infarction changes, this causes an attack of oxygen starvation and severe complications. But you can’t give up sports completely. Moderate exercise will help restore the heart muscle faster. It is useful to walk in the fresh air and do aerobics.
- Avoid harmful foods that increase cholesterol levels and cause atherosclerosis. Patients need to avoid fatty and fried foods, eat more vegetables and fruits.
- Watch your weight. If you have extra pounds, this problem must be solved, but exhausting diets are prohibited.
- Avoid alcoholic drinks and smoking.
- Avoid emotional shocks, stress, sudden changes in climatic conditions.
Compliance with these recommendations will avoid a recurrent attack and reduce the risk of complications.
Source: https://KardioPuls.ru/bolezni/sindrom-dresslera/
Symptoms
Classic Dressler syndrome develops approximately 2-4 weeks after a heart attack. The most common symptoms include heaviness and pain in the chest, fever, cough, and shortness of breath. The pathological process in most cases begins acutely, with an increase in temperature to febrile or subfebrile levels. Dizziness, weakness, nausea appear, breathing and pulse increase.
Pericarditis is an obligatory element of the symptom complex. It is typically characterized by painful sensations of varying intensity in the heart area, radiating to the abdominal area, neck, shoulders, shoulder blades and both arms. The pain can be sharp, paroxysmal, or dull, squeezing. When swallowing and coughing, there is tightness in the chest, and the pain intensifies. It weakens when lying on your stomach or standing. Palpitations, shortness of breath, and frequent shallow breathing are often observed. In 85% of patients, a friction rub of the pericardial layers appears. After a few days the pain subsides. A characteristic manifestation of pleurisy is unilateral stabbing pain in the upper torso, which intensifies with a deep breath and bending to the healthy side.
Pneumonitis is typically characterized by hard, weakened breathing, wheezing, shortness of breath, and cough. Lower lobe pneumonia develops less frequently. The disease is accompanied by weakness, excessive sweating and fever. Blood may appear in the sputum. In atypical forms of the disease, the functions of the joints are impaired.
Pericarditis and Dressler's syndrome
Pericarditis is inflammation of the pericardial sac of a rheumatic, infectious or post-infarction nature. The pathology is manifested by weakness, pain in the chest, which intensifies with inhalation and coughing. Treatment of pericarditis requires bed rest. In the case of a chronic form of the disease, the regimen is determined by the patient’s condition. For acute fibrinous pericarditis, symptomatic treatment is prescribed: anti-inflammatory non-steroidal drugs, analgesics to eliminate pain, medications that normalize metabolic processes in the heart muscle, and more. In Dressler syndrome, pericarditis is treated with drugs that eliminate the underlying disease.
Symptoms
Dressler's syndrome is manifested by intoxication, cardialgia, and polyserositis. Patients develop chest pain, weakness, weakness, malaise, fever, then symptoms of hydropericardium and hydrothorax are added.
The pain behind the sternum is squeezing or pressing in nature and radiates to the left arm, shoulder blade, and shoulder. Taking drugs from the nitrate group usually does not bring relief. When examining patients, pale skin, hyperhidrosis, hypotension, and tachycardia are noted. Auscultation reveals dull tones and a “gallop rhythm.” In this condition, patients should be hospitalized immediately.
Pericarditis
The main manifestation of the pathology is pain, the intensity of which varies from moderate to painful and paroxysmal. It is weakened by standing and worsened when the patient lies on his back, breathes deeply or coughs. The pain can be constant or occur periodically.
In addition to pain, pericarditis is characterized by the following symptoms:
- Pericardial friction noise, heard at the left edge of the sternum, especially when bending the torso forward. It decreases after fluid is released into the pericardium and consists of atrial and ventricular components, occurring in systole and diastole, respectively.
- Fever is a rise in body temperature to subfebrile levels. Intoxication syndrome is manifested by weakness, malaise, aching muscles and joints. The cause of fever is the activation of pyrogens released into the blood during inflammation.
- Leukocytosis, eosinophilia and high ESR.
- Shortness of breath, swelling of the jugular veins, hepatomegaly are signs of severe pathology.
- Palpitations, dry cough, chills, shallow and rapid breathing.
- Ascites.
- Swelling of the legs.
Pericarditis is an obligatory element of Dressler's syndrome, which has a mild course. After a few days, the intensity of the pain decreases, the body temperature returns to normal, and the general condition of the patients improves.
Pleurisy
Pleurisy is an inflammatory disease of the pleura, the main symptoms of which are: chest pain, difficulty breathing, cough, pleural friction noise, fever. Patients often complain of a scratching sensation inside.
Abdominal localization of the syndrome
The pathology is determined by peritonitis, an inflammatory process in the internal lining of the cavity. It has a clear clinical picture:
- intense, excruciating pain in the abdomen. The strength of the painful sensations decreases when you find a comfortable body position - most often lying on your side with your legs bent;
- stool disorders;
- pronounced increase in temperature.
With the development of this form of the syndrome, it is urgent to differentiate the autoimmune form from the infectious form, which is often a consequence of pathologies of the digestive tract. Treatment tactics, which most often involve the use of various groups of medications, depend on the results of timely diagnosis.
Diagnosis of pathology
We continue to describe Dressler's syndrome after myocardial infarction. What this is is now clear. However, the situation is described only in a general case; it is better for each individual person to consult with their doctor. When diagnosing this complication of a heart attack, the patient’s complaints, characteristic clinical symptoms and the results of a comprehensive instrumental and laboratory examination are taken into account. Valuable diagnostic parameters that give a complete picture of the patient’s condition include:
- Clinical criteria. Signs that confirm a high likelihood of developing Dressler's polyserositis are febrile fever and pericarditis.
- Laboratory research. In the CBC, the following are possible: eosinophilia, leukocytosis, increased ESR. In addition, a blood test is performed to check for markers of damage to the heart muscle. An increase in the level of globular proteins - troponin T and troponin I - confirms the fact of cell death.
- In the diagnosis of Dressler syndrome, an ECG is often used, which shows negative dynamics. The most typical sign is unidirectional movement of the ST segment in several leads.
- Ultrasound of the pericardium and pleural cavities.
- Chest X-ray. With the development of pleurisy, the interlobar pleura thickens, with pericarditis the cardiac shadow expands, and with pneumonitis, darkening is detected in the lungs. In some cases, cardiomegaly is clearly visible in Dressler's syndrome after a heart attack.
- In unclear diagnostic situations, MRI of the lungs and heart is prescribed.
Diagnostics
The diagnosis of Dressler syndrome is established by a combination of symptoms and the results of clinical, instrumental, and laboratory examinations. After listening to the patient’s complaints, the doctor will definitely conduct an auscultation of the chest. Typical noises indicate the presence of inflammatory processes. Their absence does not provide grounds to exclude the disease, since exudative forms most often occur secretly. In this case, inflammation can only be detected using visual diagnostic methods.
Features of auscultation in post-infarction syndrome.
| Diseases | Noise Characteristics |
| Pericarditis | At the beginning of the disease, a pericardial friction noise is heard, reminiscent of crunching snow. It intensifies if you press hard on the stethoscope, hold your breath, or take a knee-elbow position. |
| Pleurisy | Breathing is shallow and rapid. With dry pleurisy, a pleural friction noise is heard. It is very delicate, reminiscent of the rustling of leaves or rough, similar to the crunch of snow. The accumulation of exudate is accompanied by the disappearance of extraneous sounds. |
| Pneumonia | Fine wheezing, harsh breathing. |
Diabetes is an indication for the following tests:
- Blood analysis. An increase in ESR, C-reactive protein level, an increase in the number of leukocytes, and eosinophils is often detected.
- Electrocardiography. ECG changes are recorded only in the presence of pericarditis.
- Ultrasound of the heart. It may reveal thickening of the pericardial layers and an increase in the space between them. The cavity of the heart sac sometimes contains a small amount of fluid.
- Chest X-ray, MRI or CT. Visual diagnostic methods allow you to see the accumulation of fluid, the presence of characteristic changes in the structure of the lungs and pleura.
- Pleural, pericardial puncture. Using a special needle, the doctor sucks out the contents of the pleural and pericardial cavity. Characteristic signs of inflammation are the presence of a large number of eosinophils, leukocytes, and high levels of C-reactive protein.
Treatment of this disease
Treatment takes place in an inpatient setting. Emergency care for Dressler syndrome is usually not required, since there is no obvious threat to life. However, if you start treatment sooner, your chances of recovery increase significantly.
The main role in the range of therapeutic measures for post-infarction Dressler syndrome is played by drug therapy, which has several goals and involves the use of drugs with multidirectional effects:
- Cardiotropic, which help eliminate cardiac disorders. These are medications used in the treatment of coronary artery disease: beta blockers, antianginal agents, nitrates, calcium channel blockers, cardiac glycosides.
- Anti-inflammatory. In case of resistance to NSAIDs, short courses of glucocorticoids are administered. For severe forms of the disease, medications of other groups (Methotrexate, Colchicine) are used.
Anticoagulants are not used in treatment after a heart attack due to the increased likelihood of developing hemopericardium. If necessary, their use is prescribed subtherapeutic dosages. In each individual case, the treatment of this pathology is selected individually. In case of severe pain, intramuscular administration of analgesics is indicated. If there is a significant accumulation of effusion, a puncture of the pericardial cavity or thoracentesis is performed. For cardiac tamponade, surgical intervention is performed - pericardiectomy.
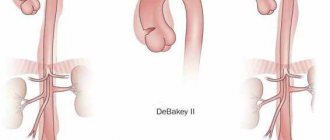
Etiology and pathogenesis
The main cause of diabetes is myocardial infarction. It is believed that diabetes often develops after large-focal and complicated infarctions, as well as after bleeding into the pericardial cavity. Diabetes, or more precisely post-cardiac injury syndrome, can develop after cardiac surgery (postpericardiotomy syndrome, postcommissurotomy syndrome). In addition, typical signs of diabetes may appear after other cardiac injuries (wound, contusion, non-penetrating blow to the chest, catheter ablation).
Currently, diabetes is considered as an autoimmune process caused by autosensitization to myocardial and pericardial antigens. Certain importance is also attached to the antigenic properties of blood entering the pericardial cavity. In post-infarction syndrome, antibodies to heart tissue are constantly detected, although they are often found in patients with MI without any signs of this syndrome, although in smaller quantities
The etiological factor of diabetes may be an infection, in particular a viral one, since in patients who developed this syndrome after cardiac surgery, an increase in the titer of antiviral antibodies is often recorded
Pathological anatomy
Even in severe cases, post-infarction syndrome does not lead to death. If such patients die from other complications of acute myocardial infarction, pathologists usually detect fibrinous, serous, or serous-hemorrhagic pericarditis. Unlike epistenocardial pericarditis, inflammation of the pericardium in diabetes is diffuse.
How to prevent the development of Dressler syndrome?
This syndrome is not considered a life-threatening condition; even in the most severe cases, the prognosis for the patient is relatively favorable. Methods of primary prevention, which is aimed at eliminating the causes of the development of Dressler's syndrome, have not yet been developed to date. However, to reduce the likelihood of articular manifestations, early activation is recommended for patients who have suffered an acute infarction. For pathologies with a recurrent course, anti-relapse therapy is prescribed to prevent re-exacerbation of the pathological process.
Forms
In cardiology, the following forms of pathology are distinguished:
- A typical or advanced form of post-infarction syndrome is manifested by symptoms of inflammation of the pericardium, pleura, lungs, and joints. There are mixed options.
- The atypical form is realized by inflammation of large joints, allergic skin lesions, development of peritonitis or bronchial asthma. More rare forms are pulmonitis, periostitis, perichondritis, synovitis, vasculitis, glomerulonephritis.
- The low-symptomatic form includes persistent low-grade fever, arthralgia, and characteristic changes in the composition of the blood.
According to the course and time of development, Dressler syndrome is divided into:
- “Early diabetes” – occurring immediately after a heart attack,
- “Late diabetes” – developing several months after a heart attack.
Clinical guidelines for Dressler syndrome
In order to reduce the risk of developing this disease, it is necessary to pay close attention to all emerging symptoms associated with heart disease. Since the initial cause of the development of Dressler's syndrome is myocardial infarction, preventive measures should primarily be aimed at preventing the development of this acute condition. The main clinical recommendation for this is timely observation by a cardiologist, taking anti-ischemic, antithrombotic drugs, as well as drugs to reduce high cholesterol levels.
Complications of this pathology
In the absence of high-quality and timely diagnosis and medical care, Dressler's syndrome can lead to the development of constructive or hemorrhagic pericarditis (the appearance of bloody exudate or compression of cardiac tissue), and in more advanced cases it causes serious cardiac tamponade. This pathology is characterized by a relapsing course with remissions and exacerbations occurring at intervals from 1-2 weeks to 2 months. Under the influence of therapy, a weakening of symptoms is observed, and in the absence of correction, the disease, as a rule, attacks with renewed vigor.