Some people have a competitive spirit that pushes them to various kinds of competitions. One of the fun things to do is hold your breath for a while. At this moment, you may feel an acute lack of air and a desire to take a breath faster. What happiness when the fear of suffocation is behind us. But it’s no laughing matter for those whose breathing intensifies or stops due to a person’s psychological or emotional state. There are signs of heart disease, asthma or diseases in the respiratory tract. But this is just shortness of breath with VSD, which frightens not only the person suffering from the disease, but also those around him.
Is there a danger from shortness of breath if this is a symptom of vegetative-vascular dystonia? How can a person cope with an attack of suffocation if breathing problems occur frequently?
Introduction
As a rule, people get used to putting up with most of the symptoms and attribute them to the characteristics of the body, poor health in general. But sometimes difficulties arise that cause serious anxiety and acute attacks. To a greater extent, they are associated with problems of the heart, blood vessels and respiratory tract.
Lack of air during VSD is a common and quite typical situation. The first thing you should focus on is fixability. The fear of asphyxia and heart attack is caused more by the psychological factor of losing control over the natural processes of one's own body than by a real physical threat.
Treatment of the disease
The appearance of lack of air during VSD requires the patient to contact a medical center. Restoring the breathing process is a complex and lengthy process. The doctor examines the patient and collects anamnesis, which allows him to make a preliminary diagnosis. If the need arises, consultation with an endocrinologist, ENT specialist and neurologist is recommended.
To confirm the preliminary diagnosis, instrumental examinations are recommended. The patient needs to undergo an x-ray of the lungs. Experts recommend performing an ultrasound examination of internal organs. This technique is used to determine the performance of the thyroid gland. Only the neurologist who prescribes the treatment can confirm the diagnosis.
To combat pathology, it is recommended to use an integrated approach. Psychotherapy is used to treat the patient, which allows him to change his attitude towards the pathological process.
If there is a lack of air during VSD, then it is recommended to perform special exercises to restore respiratory function. A complex of breathing exercises is developed by the doctor depending on the individual characteristics of the person and the severity of the pathology.
The patient must perform exercises daily and strictly adhere to the doctor’s recommendations, which will have a positive effect on the treatment process.
To prevent the pathological process, breathing exercises are performed using the abdomen. It is recommended to inhale twice as long as exhale. Classes should only be conducted in a calm environment. The duration of the exercises is at least 30 minutes a day .
Drug treatment
If the symptom occurs against the background of psychological disorders, the patient must take certain medications. Most often, patients are prescribed antidepressants and axiolytics. During the period of vegetative-vascular dystonia, patients are prescribed:
- Gidazepam;
- Corvalorla;
- Anaprilina.
Treatment of a pathological process with medications requires strict adherence to the dosage and doctor’s recommendations, which will eliminate the possibility of developing undesirable effects.
To achieve the highest possible therapeutic effect of medications, it is recommended to simultaneously conduct psychotherapy. With its help, the patient’s psychological state is restored and the breathing process is restored.
First aid
If attacks of shortness of breath occur, which are accompanied by a short-term loss of consciousness, the patient must be seated or laid down. If there is tight clothing, unbutton it or take it off. If the patient is indoors, then it is necessary to provide access to fresh air by opening windows and doors. The patient is revived by splashing the face and neck with cold water.
In order to restore the optimal ratio of oxygen to carbon dioxide in the lungs, you need to breathe into folded palms or a plastic bag. If an attack occurs, it is recommended to drink a glass of water in which a spoonful of sugar is first dissolved. If shortness of breath occurs, wash with cold water.
Therapy of the pathological process is labor-intensive. It should be carried out only under the supervision of a doctor and taking into account his recommendations, which will have a positive effect on the result.
General information
The feeling of lack of air during VSD can be due to various reasons. Shortness of breath may be caused by dystonia itself, but it may simply be a contributing factor. In both cases, an accurate medical diagnosis of the cause is extremely important.
In a situation where interruptions in breathing stem from real problems and illnesses (for example, coronary heart disease or bronchial asthma), using classic psychotherapy for VSD will simply be irrational - no more reasonable than applying plantain where plaster is required.
The opposite situation is also unsafe - when the symptoms are confused by the initial self-diagnosis, difficulty breathing is a consequence of autonomic disorders due to developing neurosis, and the patient is diligently treating fictitious asthmatic complications... Advanced VSD also leads to more serious complications than compression in the chest and difficulty breathing under stress.
Symptoms of hyperventilation
Not everyone experiences the syndrome in the same way. Its symptoms may be similar to those of a heart attack, and the syndrome may “masquerade” as a disease of the thyroid gland or lungs. It differs from asthma in that a person experiences difficulty not when exhaling, but when inhaling. Main manifestations of the syndrome:
- inability to take a deep breath;
- feeling of insufficient inhalation (lack of air);
- constant yawning;
- sore throat, dry cough;
- the appearance of fear of death (panic attack);
- fear of cramped conditions and stuffiness;
- when inhaling there is a feeling of a “coma” in the throat;
- pain in the heart area;
- tightness in the chest;
- a feeling that takes your breath away.
In addition, the removal of carbon dioxide from the body leads to muscle spasms, numbness in the areas around the mouth, feet and hands. Mineral imbalance manifests itself in the form of dizziness, trembling of the arms and legs. Such symptoms cause even greater anxiety in the patient, which aggravates the course of vegetative-vascular dystonia. Sometimes hyperventilation during VSD can be accompanied by other characteristic syndromes - cardiovascular or hyperexcretion syndrome (increased sweating).
Why suffocation causes fear
Even in the initial stages of VSD development, when crises are not so acute and other symptoms of the disease are not pronounced, breathing difficulties can frighten the patient. Accompanied by sudden sharp pain in the sternum, they resemble signs of heart failure. Occurring unexpectedly, in the middle of the night, in a state of anxiety or emotional fluctuations, the slightest changes in breathing can lead to panic attacks. Fear of suffocation blocks adequate perception of reality and leads to the development of real phobias.
Most often, in the presence of dystonia (one of its types), the patient is diagnosed with hyperventilation syndrome. But this is not the only form that a violation of oxygen metabolism in the body takes on with autonomic disorders of the nervous system.
Breathing disorders due to VSD: mechanism of development
The mechanism of hyperventilation syndrome itself is complex and until now a complete concept of the mechanism of its development has not been fully formulated. Most researchers agree that when in a stressful situation, in a state of fear, overwork or anxiety, a person can unconsciously change the depth of breathing and its rhythm. Trying to provide the muscles with an additional flow of oxygen, a person, as if before a sports competition, tries to breathe faster. Breathing becomes frequent and shallow, but additional oxygen remains unclaimed. This leads to subsequent unpleasant and frightening sensations of lack of air in the lungs.
Moreover, the occurrence of such disorders leads to a state of constant anxiety and fear, which ultimately contributes to the appearance of panic attacks, which aggravate the course of the already “difficult” hyperventilation syndrome.
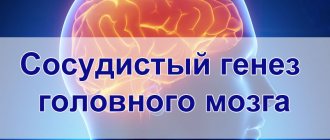
Improper breathing leads to changes in blood acidity: frequent shallow breaths lead to a decrease in carbon dioxide levels in the body. A normal concentration of CO2 in the body is necessary to maintain the walls of blood vessels in a relaxed state. Lack of carbon dioxide leads to muscle tension, vasoconstriction - the brain and body begin to experience oxygen deficiency.
It is believed that for the occurrence and development of hyperventilation syndrome, the presence of two factors is sufficient: 1. Individual predisposition (for example, physical fatigue; experience of “improper breathing”, when interruption of breathing was accompanied by discomfort; etc.); 2. The impact of various external, so to speak, circumstances (stress, pain, infection, etc.). At the same time, even if the triggering causes are eliminated (what triggered the increased activity of the respiratory organs), hyperventilation continues to function. Thus, a “vicious circle” is formed, which begins to circulate autonomously. And the symptoms can last a long time [].
I forgot how to breathe
An absurd but frequent recognition of people suffering from apnea (short-term involuntary cessation of breathing). This happens to many people in their sleep: a person wakes up with the feeling that the lungs have stopped working, and oxygen has not entered the body for a long time.
Shortness of breath during VSD is associated with fear and exaggeration of the catastrophic nature of the situation: the person sits up abruptly in bed, begins to breathe shallowly and rapidly. The pressure rises, the heart beats faster, trying to quickly fill the lack of oxygen in cells and tissues. Interruptions in pressure do not relieve difficulty breathing. On the contrary, dizziness, darkening of the eyes, and a feeling of hopelessness are added to them.
All of the above fits perfectly into the classification of both panic attacks and classic apnea. But why does the patient lose his breath at a time when the body should be as relaxed as possible?
Major breathing problems
Patients experiencing shortness of breath during VSD do not always clearly indicate what kind of discomfort in the respiratory tract arose.
- It is difficult for those with shortness of breath to take a deep breath. No matter how much a person inhales, there is a lump in the throat, oxygen remains at the upper limit. I want to breathe deeper, but something is stopping me;
- Other patients with shortness of breath during VSD complain of the inability to exhale. There is no carbon dioxide in the lungs, which must be expelled as a waste product;
- A heavy deep breath, a suffocating cough, snoring, yawning - these are also symptoms of breathing problems during vvd, which are provoked by an incorrect reaction of the autonomic center.
Lack of air in the form of shortness of breath during VSD is deceptive, because there is an excess of oxygen in the blood, but it does not reach the brain. There is no physical activity, no carbon dioxide is produced. Panic appears, which can provoke hyperventilation and fainting if the patient does not pull himself together.
In addition to shortness of breath with VSD, a person experiences additional symptoms:
- Sweating with chills;
- The heartbeat increases and there is a feeling that it will jump out of the chest;
- The pupils may dilate and there is a state of panic in the eyes;
- Problems with the gastrointestinal tract (diarrhea, flatulence, bloating, pain, nausea).
Shortness of breath during VSD in some cases causes headache, dizziness, temporary blurred vision (a feeling of a veil or spots in the eyes). The cause of VSD symptoms is oxygen starvation of the brain.
Is it possible to “forget” how to breathe?
The fact is that both the somatic and autonomic nervous systems are responsible for the regulation of respiratory processes. In other words, it happens both consciously and uncontrollably. We can, of our own free will, hold our breath, make inhalations and exhalations deeper or shallower, and regulate the muscular movement of the chest, thus influencing the process of gas exchange. But when we are distracted, focused on extraneous tasks, in deep sleep or in a stressful situation, unable to pay attention to the breathing process, it is the autonomic nervous system that controls the depth and frequency of breaths, heart rate and other related factors.
When the autonomic system begins to malfunction and not function as it should (vegetative dysfunction), everything that was previously controlled by it also goes into discord. The body's reactions cease to correspond to external stimuli, tachycardia and panic occur without actual danger, shortness of breath - without physical exertion, eating disorders and allergies - without real poisoning and allergens, and so on.
Symptoms
Shortness of breath caused by VSD manifests itself in different ways. Patients complain about:
- Heaviness in the sternum, a feeling of constriction in the chest.
- Sharp stabbing pain when inhaling.
- Heavy breathing and shortness of breath that occurs during light exertion, when singing or talking, or during emotional experiences.
- Feeling of lack of oxygen when breathing.
- It is difficult to inhale and exhale; the process of breathing itself seems like an effort that causes shortness of breath.
- Waking up from deep sleep with the feeling that breathing has stopped.
The last point causes particular concern for those suffering from dystonia, and after it - possible insomnia.
Dream
Why do night attacks frighten patients so much? The formulation “I forget to breathe in my sleep” is illogical, as we have already discussed, primarily because memory is not involved in the breathing process while the brain is immersed in the sleepy phase.
What really happens to those who say, “I feel suffocated at night”? In medical terms, their body experiences apnea - cessation of pulmonary ventilation due to weakening of the muscle tone and soft tissues of the throat. When falling asleep, the muscles seem to “sag,” blocking the airways. Classic apnea lasts up to 10 seconds, hypopnea takes 10 seconds or longer. This time is enough to awaken the brain and send an SOS signal about the problem.
“I wake up because I can’t breathe” is a reason for an examination, but in no case for momentary panic. By getting out of a lying position and consciously doing a series of breathing exercises, you can bring the nighttime incident under control and prevent a panic attack.
Hangover
A healthy lifestyle as the main cure for VSD automatically includes giving up alcohol. After drinking alcohol, it is doubly difficult for the body to cope with autonomic dysfunction - the need to remove toxins from the blood, an imbalance in sugar and hemoglobin levels also affects the amount of oxygen supplied with blood flow to the lungs.
Why is it hard to breathe when you have a hangover? Yes, at least from the fact that the illusory feeling that during VSD there is not enough air, actually means an insufficient number of oxygen molecules entering the cells of the tissues of the internal organs.
Shortness of breath is provoked by any strong stress on the body, and the state of alcohol intoxication is quite one of them.
Diagnostics
It is necessary to exclude the presence of other diseases that also cause shortness of breath
The reasons why a person has difficulty breathing are very diverse, so you need to see a doctor to confirm the diagnosis of VSD. It is necessary to consult with several specialists at once. First you need to see a therapist. He will conduct a general examination, prescribe an ECG and a number of other examinations to exclude cardiovascular pathologies. If no abnormalities are detected, the patient will be referred to a neurologist. The doctor conducts a general examination, excludes pulmonary neuralgia, since this disorder is often accompanied by sudden shortness of breath, prescribes a series of laboratory tests and only then makes a diagnosis. It is imperative to check the functioning of the heart, to exclude infectious diseases and nerve damage, including against the background of osteochondrosis.
Note! Shortness of breath is often observed with cervical osteochondrosis due to compression of the spinal nerve roots.
After all the examinations, the doctor will draw up a treatment regimen, taking into account other symptoms observed in the patient.
Yawn
The feeling of lack of oxygen (not air in general, but an element in the body) is not always caused by physical exertion or physical breathing disorders.
Sometimes patients complain that they constantly yawn without an objective reason (lack of sleep, etc.). Yawning is also an indicator of oxygen deficiency in the body and manifests itself as a reflex.
The common belief that yawning is “contagious” is associated with the phenomenon of psychogenic shortness of breath and neurotic consequences, when the breathing disorder of others (for example, a family member) is unconsciously copied by a person. This situation is especially dangerous in infancy. There are cases where an absolutely healthy child reflexively repeated the intermittent, rapid breathing of the parent, which over time progressed into its own pathology.
What is shortness of breath?
Scientifically, respiratory failure is called pulmonary hyperventilation syndrome. The main feature of this condition is difficulty inhaling and exhaling . Such a disorder has nothing to do with the improper functioning of the respiratory system, but is caused by a violation of cardiovascular function.
During hyperventilation, rapid breathing occurs with the capture of large volumes of air. This is the symptom that characterizes VSD.
Causes of difficulty breathing
Situations when a person has difficulty breathing with a hangover, after a cycle of exercise, or when waking up at night seem not as critical as the ragged breathing of a person at rest. When breathing is difficult in a lying old person or baby, in a healthy adult in the fresh air, in a teenager leading an active lifestyle - why is there not enough oxygen in such cases?
The causes of respiratory failure may lie in a number of congenital pathologies. Choking during VSD can be a reaction to neurotic attacks; hypoxia is sometimes a side effect of heart failure, a tendency to hypotension and coronary heart disease, problems with the lungs and even with the muscular frame of the chest.
Osteochondrosis and spinal problems can also affect breathing difficulties. The reasons, whatever they may be, should be carefully investigated by the attending physician.
How to recognize psychogenic shortness of breath
In a state of severe stress, a person sometimes does not even notice shortness of breath. Awareness comes only when others ask him why he breathes so often, because he is quite calm in appearance and does not make any intense movements. In this case, we can talk about such a condition as shortness of breath at rest with VSD.
For example, dystonics experiencing irrational fears may begin to breathe rapidly just at the thought of a “threatening” object. In many cases, they do not even draw a parallel between the symptom and the existing disorder and mistake various uncomfortable sensations in the chest for pain in the heart.
We recommend reading: Hair loss due to stress - how to preserve your hair?
Psychogenic shortness of breath can be recognized by the following accompanying signs:
- tachycardia, blood pressure surges;
- frequent urination;
- headaches, numbness or coldness of the extremities;
- body tremors, diarrhea;
- heat in the face and neck.
If rapid breathing is accompanied by a cough and copious expectoration, patients often resort to using various antitussives, which does not bring any results. This circumstance may also indicate the psychogenic nature of the respiratory rhythm disorder.
I choke when I'm nervous
It is important to remember that any symptoms of vegetative-vascular dystonia are closely related to the psycho-emotional sphere. Breathing under stress becomes shallow and constricted, muscles contract spasmodically and are in constant tension. Complaints of “suffocating in the morning” may be a consequence of a nervous habit developed to return to a nervous state as soon as the brain leaves the deep sleep phase.
It happens that it is impossible to take a deep breath when one (no matter whether positive or negative) bright emotion dominates, it is difficult to inhale after eating or sleeping, there is pressure in the sternum due to changes in internal pressure and external temperature. This can be associated with any change in the external situation or internal state - only the fact that the body malfunctions instead of harmoniously adapting to the situation is important.
Causes
Hyperventilation
The first cause of shortness of breath with VSD. Since vegetative-vascular dystonia is simply a bodily reflection of constant stress and anxiety, people suffering from this scourge often force their breathing. Without even noticing it. After all, they are constantly preparing to either flee or attack. Although it may seem to them that this is completely wrong.
Nevertheless, it is so. Therefore, their body introduces more oxygen than necessary. And it emits more carbon dioxide than it should. After all, he is preparing for active muscular work. Which in the end it doesn’t exist. Therefore, a state of hyperventilation develops, which is often felt by a person as a lack of air, shortness of breath.
Holding your breath
Quite often, it becomes difficult to breathe with VSD simply because the person is not breathing. Some neurotics, who are sure that they have heart and/or lung diseases, develop a “gentle” type of breathing for themselves: they begin to breathe very shallowly. They think that this way they minimize the load on diseased body systems.
Of course, the effect of such “gentle” behavior turns out to be the opposite of what was expected. Shortness of breath, a feeling of lack of air appears. How can they not appear if a person is constantly actually holding his breath?
Respiratory muscle strain
It may be difficult to breathe during VSD because the respiratory muscles are too tense. Like all other skeletal muscles.
Some even specifically tense their abdominal muscles. So it seems to them that the heart is not beating so fast, and breathing is not so deep. And it's supposedly safe.
Of course, such muscle strain in the chest, abdomen and back does not pose any threat to life or health. But it can be subjectively perceived as difficulties in performing breathing movements.
Drying of the mucous membranes of the upper respiratory tract
It may be difficult to breathe due to nerves because the nasal mucosa is drying out. This drying out is associated with spasm of the capillaries of the mucous membrane, which develops against the background of stress.
Again, such a spasm is not life-threatening in any way, but it can cause a neurotic person to open his mouth and begin to puff as if he were running or suffering from a severe runny nose.
Not only the nasal mucosa can dry out, but also the throat. And this often becomes the cause of a nervous cough.
Heartbeat
Shortness of breath during neurosis often occurs against the background of increased heartbeat, which, in turn, is directly related to the anxious state in which the person is.
The stronger the pulse, the faster the breathing. This is the norm.
Fear, suspiciousness and hypersensitivity
All of the above physical symptoms of psychogenic shortness of breath are only theoretically physical. In fact, they are a bodily reflection of the nervous tension and fear in which a patient with VSD resides.
Therefore, the main cause of nervous breathing problems is suspiciousness (constant monitoring of one’s well-being) and fear when something becomes “wrong” with the state of the body.
Very often, an attack of fear of suffocation, which develops into a panic attack, develops as follows:
- the person is nervous;
- he experiences natural changes in breathing, which provoke the development of the “symptom of shortness of breath”;
- next comes fear;
- and after the fright there is a further increase in symptoms;
- increased fear, panic, etc.
This results in an acute attack of psychogenic shortness of breath, often developing into a panic attack.
At the same time, breathing problems with VSD can also be chronic. In this case, acute panic does not develop. But a person constantly thinks that it is “hard for him to breathe, there is not enough air, now he will suffocate, etc.”
Against the background of such thoughts, which lead to chronic nervous excitement, chronic psychogenic shortness of breath occurs. Since a neurotic person worries all the time, listens to himself, and therefore constantly “suffocates.”
Irrational should thinking
So, people who have shortness of breath due to neurosis constantly think that they are suffocating. These thoughts are intrusive. Suspiciousness is high.
However, in addition to these thoughts, they also have irrational thinking of must, which in this case convinces them that they:
- should always breathe absolutely evenly;
- they may not suddenly want to take a deep breath;
- their breathing should not accelerate;
- the nose should not dry out, etc.
That is, their respiratory system must work like the mechanism of a Swiss watch. And nothing else. And if it works a little differently, then they die.
But man is not a robot. The functioning of his internal organs is constantly changing slightly. And this is the norm.
All people on Earth “suffocate” from time to time. They just aren't afraid of it. They don't pay any attention to it at all.
Look at the first grader. He sits and writes the first letters in his life. The mouth is open. Panting from tension.
A Vsdeshnik in such a situation would immediately decide that it is difficult for him to breathe, there is not enough air, etc. But the first-grader does not notice that he is “suffocating.” He doesn’t notice because there are no irrational thoughts in his head that he shouldn’t puff. And if it puffs, it means it’s the end.
A neurotic person has such thoughts in his head. Therefore, he regards normal changes in breathing caused by nervous tension as a symptom of a serious illness. Scared. And off we go...
Bronchial asthma
Sometimes vegetative crises (acute attacks of worsening symptoms of dystonia) are associated with similar exacerbations of another disease. Thus, night suffocation, dry frequent cough with VSD and the inability to breathe fully can be manifestations of bronchial asthma.
Sometimes a short-term, lasting several seconds feeling of “forgot how to breathe” is replaced by an annoying asthmatic cough and happens in moments of emotional fluctuations. Respiratory processes are closely related to the coordination of the nervous system, both conscious and unconscious; this means that asthma in the case of experiencing VSD can be just psychosomatic.
Correct breathing for vegetative-vascular dystonia
Treatment with a psychotherapist will help you deal with your inner feelings and fears. In addition, a person will learn to correctly assess the situation, without perceiving everything in the worst terms. The main aspect of therapeutic therapy is breathing exercises for VSD. Classes are conducted gradually, without pursuing instant results.
In a relaxed state, you need to sit on the floor, you can do it in the lotus position (cross your legs together in a sitting position). At these moments, it is necessary to protect yourself from extraneous thoughts and ideas. It is important to fully concentrate on the training. Moderate temperatures in the room, without other noise, will have a positive effect. It would be a good idea to place a small container of water nearby. Water can be sweetened, because glucose has a beneficial effect on brain cells, thereby promoting vasodilation.
In the process of completing tasks, you need to learn the following techniques for self-control during stress:
- Replace chest breathing with diaphragmatic breathing movements.
- Control the gap between the perfect inhalation and exhalation.
- Ensure calm and peaceful breathing.
Why there is a lump in the throat with VSD and how to eliminate it
What are the breathing exercises for VSD? In the first point, there is a correct change in breathing, which helps create a positive emotional background. The second paragraph talks about regulating respiratory movements, which is the main measure to prevent a lack of air flow in case of vegetative-vascular disorder. The third point involves self-control of the respiratory center, which helps restore gas exchange within the pulmonary organs.
The first sessions of breathing exercises may be difficult, but there is no need to be sad. Regular training will teach you to control emotions and breathing. The key to exercise is to maintain a daily routine without overeating, excessive physical activity, as well as hypothermia and overheating. Before starting class, you need to eat no earlier than one and a half to two hours, otherwise it will be difficult to concentrate. During the therapy period, you need to protect yourself from noisy entertainment events, drinking alcohol, smoking, and taking psychotropic medications.
Treatment
Whatever the symptoms, they all complicate the normal course of life, and the person needs the help of a specialist. For clarification, they turn to a therapist, neurologist, cardiologist, psychotherapist - each of these specialists can conduct an examination at their own level in order to find out as accurately as possible what caused the breathing disorder.
Often, in the absence of hereditary pathologies, diseases of the cardiovascular system and without an urgent need for drug treatment of developed neurosis, the problem is solved quite simply. Methods of relaxing physiotherapy, psychological self-diagnosis during attacks and herbal preparations are selected individually for each patient.
Treatment of shortness of breath with tablets
In special cases, when respiratory problems are caused by the development of clinical neurosis, drug therapy is used to treat it. However, any antidepressants, sleeping pills and sedatives must be prescribed by the attending physician and agreed with the diagnosis confirmed by other specialists. Otherwise, drug intervention can only worsen the problem.
For example, if a person at the self-medication level decides to take a course of sleeping pills in order to stop waking up at night, this will not save him from hyperventilation. It will only be more difficult for the body to “ask for help” to the brain when, due to weakening muscle tone, the lungs stop working for 10-15 seconds.
It is important for a person suffering from psychosomatic apnea, first of all, to explain how to breathe correctly and calm the growing fear of suffocation during an exacerbation of the VSD crisis.
Breathing exercises
In order to restore breathing not only in the current moment, but also to ensure a restful night's sleep without unscheduled awakenings, therapeutic exercises are used. It includes both physical exercises to calm the nervous system (such as yoga, stretching and relaxation massages) and statistical breathing exercises.
Their types vary depending on the goal pursued, but one way or another they include training:
- deep breath;
- control the depth and duration of inhalation and exhalation;
- number of inhalations and exhalations per minute;
- control of the intensity of diaphragm work;
- conscious participation in the respiratory process of other muscle groups.
The benefits of deep breathing are mainly due to increased oxygen saturation. In addition, the depth of inspiration slows down its speed, which means it reduces the risk of involuntary tachycardia, when the heart begins to beat faster than expected due to a series of short shallow breaths.
Breathing yoga
Various yoga practices offer a combination of a set of exercises aimed not only at flexibility and muscle tone, but also at the health of internal organs. Aligning the heart rate and eliminating internal smooth muscle tension caused by psychosomatics is a useful skill for diagnosed VSD.
Conscious breathing is first practiced according to the indicated patterns (alternate breaths from each nostril, alternating their depth and duration), then introduced to the level of habit. So, thanks to weeks of training, you can train your body in a stressful situation to slow it down instead of increasing your breathing, urging the body to first calm down and relax.
Therapeutic breathing exercises
Since the middle of the last century, breathing exercises using the Strelnikova method have been actively used in the USSR and are still considered an ingenious method. Including the work of many muscle groups, it helps not only to establish uniform deep breathing, but also to recover after surgery, develop a voice, relieve fatigue, perform a “massage of internal organs,” etc.
It is used not only as a treatment method, but also as a preventive measure, recommended also for adolescents and children. A specially designed set of exercises can replace 15-30 minutes of morning and evening exercises, as well as a relaxing massage session.
Correctly performed breathing exercises are recommended in the presence of both VSD and other concomitant diseases - neurosis, asthma, hypertension, etc.
Treatment of respiratory neurosis
When deciding how to get rid of respiratory tract neurosis, you need to understand the importance of an integrated approach in this matter. Drug treatment should be accompanied by a course of psychotherapy.
Treatment with drugs
Drug therapy is determined after a series of tests, since the signs of neurosis are similar to the manifestations of other diseases. Based on the complexity of the pathology, the degree of its development and the characteristics of the patient’s body, the doctor prescribes the necessary medications. A patient with a severe form of respiratory neurosis may be prescribed the following types of medications:
- herbal based sedatives;
- tranquilizers and antidepressants that relieve anxiety and stabilize the patient’s psycho-emotional state;
- antipsychotic drugs that block areas of the brain that affect the occurrence of neurological shortness of breath;
- vitamins B and D, some types of microelements (magnesium, calcium);
- beta blockers.
A complex of sedatives is often prescribed to be taken during all stages of the disease, including during the recovery period.
You cannot prescribe therapy yourself, since a number of medications have contraindications. Improper use can lead to worsening of the condition and even death.
Treatment with folk remedies
You can relieve the symptoms of respiratory neurosis in children and adults using traditional medicine. The effect of most decoctions is sedative.
For example, mix crushed chamomile flowers, caraway fruits and valerian root in a ratio of 3:5:2. Take 1 tbsp. l. mixture and pour a glass of boiling water. Then let it brew for 20-25 minutes. Drink to reduce irritability, anxiety and excitability.
Herbs such as hawthorn, motherwort, mint, chamomile, etc. have a good effect.
Psychotherapy
Sessions with a psychotherapist involve identifying a problem that disturbs a person’s calm and leads to psycho-emotional disorder, as a result of which respiratory tract neurosis manifests itself. The work is carried out in several stages:
- Awareness that a problem exists and needs to be solved.
- Understanding that some circumstances cause a strong negative impact on the patient’s life and because of this, its quality greatly deteriorates.
- Recognizing the cause that leads to stress. This is a long process, since it does not always lie on the surface and can be realized.
- Gaining the skill to look at what is happening around you differently. A person tries to change his habitual thinking to a positive one.
- Developing the ability to manage and overcome an anxious state independently.
It is important for a person to understand to what extent his fear is justified and what steps he can take to avoid it.
Prevention
In order to prevent the situation from worsening in the presence of VSD, it is necessary to observe a number of simple conditions for a healthy life. The number one tip is balanced physical activity.
A sedentary lifestyle, cardiac problems and a poorly developed respiratory system are fertile ground for dystonia. To train the body we recommend:
- physiotherapy;
- fitness (but not active cardio exercises);
- yoga;
- swimming and various water procedures;
- breathing exercises;
- walking in the fresh air;
- control over emotional state.
A few more tips
In order to prevent the occurrence of neurological shortness of breath due to psychological problems, the body should be given a break from mental stress. If a person devotes most of his time to office work, it is recommended to spend leisure hours paying attention to the body, and not to the screen of the phone, TV and computer.
Sometimes taking sedatives helps in the fight against neurosis, also having a beneficial effect on the functioning of the cardiovascular system and respiratory organs.
Every night 7-8 hours of healthy sleep in a clearly established mode, relaxation sessions and selected therapy, a positive psychological attitude towards conscious healthy life - all this helps to establish harmonious functioning of the body.
- Symptoms and treatment of VSD against the background of cervical osteochondrosis
- Symptoms of cardiovascular dystonia and methods of its treatment
- What to do when your heart hurts from worries?
- Algorithm for the treatment of VSD, panic attacks and phobias
Diagnosis of shortness of breath with VSD
Shortness of breath, as a symptom of VSD, can be confused with a serious pathology that must be treated under the supervision of a therapist or specialist. Choking may indicate heart failure, vascular dystonia, head or spinal injuries, colds or viral complications.
To confirm the symptoms of VSD in the form of shortness of breath, you need to go to the clinic and undergo a full examination to confirm that shortness of breath is a sign of VSD:
- A conversation with a therapist who, through a visual examination, will try to understand the cause of shortness of breath;
- Referral for laboratory study of biological material (blood, urine).
- Hardware diagnostics of the heart, lungs, and other organs if the doctor suspects another pathology (X-ray, ultrasound, MRI, ECG);
- Consultation with a neurologist, cardiologist, endocrinologist to exclude problems in the heart, spinal regions, and thyroid gland;
- A conversation with a psychiatrist to identify the root cause of shortness of breath during VSD, which occurs during panic attacks.
Having received a doctor’s conclusion that the patient has no organic pathology, you can choose treatment that will help cope with shortness of breath during VSD.
In some cases, shortness of breath with VSD is a secondary problem for the patient, because it arose against the background of organic pathology, for example:
- Chronic colds;
- Problems in the spine, especially in the cervical region, when the symptom of suffocation is provoked by compression of the vertebrae in the chest area. The patient may confuse the occurrence of shortness of breath with VSD with a problem in the heart, or a heart attack may be hidden under an asthmatic spasm;
- Vascular dystonia, provoked by the formation of plaques, thinning of the walls of blood vessels;
- An allergy expressed in the form of an asthmatic attack.
If shortness of breath during VSD causes fear and is repeated with a certain frequency, the patient may be in a nervous state. A single attack of shortness of breath during VSD, when there is a feeling of approaching death, creates a platform for a person to have panic attacks and difficulty breathing, although there is no real threat.