Pericarditis is a large group of inflammatory diseases of the pericardium of primary and secondary origin.
Among all types of pericarditis, the dry form is the most common. The uniqueness of the clinical manifestations makes it possible to suspect inflammation of the pericardial sac in time and seek medical help.
The article discusses the causes, signs and distinctive features of dry pericarditis, as well as methods of diagnosis and treatment.
Dry pericarditis - what is it?
Fibrinous pericarditis (ICD-10 code: I30) is an inflammatory disease of the outer and inner layers of the heart sac, accompanied by the deposition of the inflammatory protein fibrin between them.
The incidence is 0.1% of all cardiac pathologies.
Has the following characteristics:
- Local swelling;
- Local increase in temperature and dilation of blood vessels;
- Pain syndrome;
- Dysfunction of the cardiac membrane.
Fibrinous inflammation may be an early stage of other types of pericarditis. In response to the action of the etiological factor, a specific protein, fibrin, falls out on the pericardial layers. Fibrin deposits are white sticky thread-like masses. Their massive deposits lead to adhesion and destruction of the cardiac membrane.
Ischemic disease Macropreparations Myocardial infarction 1
Objectives 1) Histologically, an area devoid of nuclei and surrounded by young connective tissue was found in the myocardium. Name the process and its outcome. In what diseases does the described picture most often occur? 2) At the autopsy, liquid blood and blood clots were found in the cardiac membrane. Heart weighing 650 g. , the thickness of the wall of the left ventricle is 2.5 cm. In the apex region, a large area of the myocardium throughout the entire thickness of the wall has a gray-yellow color and a soft consistency. In the epicardium above this area, a narrow gap is visible, the edges of which are saturated with blood. What disease are we talking about according to the modern classification of diseases? What is its morphological manifestation in the heart? What is the immediate cause of death? What is the underlying disease? 3) Two hours later, after the onset of the attack of chest pain, the patient died. Myocardial infarction was diagnosed electrocardiographically. What stage of a heart attack are we talking about? With the help of what reagents is macroscopic diagnosis of a heart attack at this stage possible? What histochemical features are characteristic of this stage of infarction? What structural changes in myocardiocytes are typical for this stage? Possible causes of death of a patient at this stage of myocardial infarction? 4) An obese man, who smoked two packs of cigarettes a day for 10 years and suffered from hypertension, suddenly developed a prolonged attack of chest pain. Three days later, death occurred due to symptoms of acute heart failure. What disease was accompanied by an attack of angina and led to the patient’s death? What changes in the heart could be detected at autopsy? What changes could be detected in the coronary arteries of the heart? What risk factors did this patient have? What disease can be considered background? 5) A patient who had suffered from atherosclerosis for many years and had previously suffered a myocardial infarction developed a prolonged attack of chest pain. The patient is hospitalized. Three days after hospitalization, a sudden expansion of the borders of the heart to the left occurs, and heart pulsation appears in the area of the apex. Against the background of progressive heart failure - right-sided hemiplegia. What disease can be assumed in this case? What disease should be considered background? What heart complication can you think about? What can be associated with the development of hemiplegia? 6) A patient who suffered a massive transmural myocardial infarction two years ago has a significant expansion of the borders of the heart, pulsation of the heart at the apex, shortness of breath, cough with rusty sputum, an enlarged liver, and edema. When these symptoms increase, the patient dies. What disease does the patient have? The form of this disease, the cause of death?
Causes and mechanism of development
Dry pericarditis can be primary or secondary. Primary develops without a previous disease, secondary - after it. Among the main etiological factors are:
- Microbial agents;
- Hypothermia;
- Systemic autoimmune diseases;
- Metabolic pathology.
The most common causes of dry pericarditis are viral infections of the respiratory tract and intestines, pneumonia, and influenza.
At the first stage, blood cells are attracted to the site of inflammation. Edema, local fever, and infiltration of platelets and leukocytes develop. During the second stage, the level of fibrinogen, the precursor protein of fibrin, increases in the blood. In the third stage, the accumulation of fibrin leads to the adhesion of the pericardial layers to each other.
Reasons for development
The main causes of fibrinous pericarditis are the following conditions or diseases:
- viral infections - enteroviruses, cytomegaloviruses, Coxsackievirus, HIV, mumps (mumps);
- bacterial infection;
- autoimmune diseases – systemic lupus erythematosus, rheumatoid arthritis;
- rheumatism;
- tuberculosis processes;
- pneumonia;
- myocardial infarction;
- terminal phase of chronic renal failure;
- malignant neoplasms;
- blood poisoning;
- damage to the chest organs, as well as surgical interventions performed in this area.
The consequences of all these diseases or conditions can be an inflammatory process in the pericardium, which can lead to the proliferation of fibrin fibers.
Symptoms and signs by stage
Along the way, three forms of the disease are distinguished:
- Acute (up to 2 weeks);
- Subacute (2 weeks – 6 months);
- Chronic (more than 6 months).
Acute dry pericarditis is characterized by vivid symptoms and severe pain . The pain develops gradually, over the course of a day, and is stabbing, cutting or squeezing in nature. There is an increase in pain when bending the body, coughing, eating and at the height of inspiration. Pain syndrome is accompanied by:
- Fever;
- Muscle weakness;
- Drowsiness;
- Redness of the skin of the face and chest.
The patient notes a feeling of uneven, loud heartbeat, interruptions in heart function. Characterized by self-limitation in food and physical activity, shortness of breath. The disease is accompanied by insomnia due to deterioration in the lying position.
The subacute form is transitional between acute and chronic and does not always develop . It is most typical for elderly patients with late or irrational treatment. A distinctive characteristic of this form is the reduction of pain and normalization of body temperature. Patients complain of palpitations, shortness of breath, and dizziness.
The chronic form is characterized by a successive change of remission and exacerbation . During the period of exacerbation, the clinical picture corresponds to the symptoms of acute fibrinous pericarditis; during remission, patients feel satisfactory. Exacerbations occur during the cold season or after the action of a provoking factor (infection). Fever rarely develops.
What happens to the cardiovascular system?
With a small lesion, fibrin resorption occurs quickly. In view of this, cardiac damage is minimal in the form of tachycardia and a decrease in stroke force. With massive protein deposits, an irreversible adhesive process develops.
Organic changes in the pericardium complicate ventricular contractions and lead to the development of extrasystoles, arrhythmias and blockades. Cardiac tamponade does not develop.
Clinical manifestations
At the first stage, the disease is quite difficult to diagnose.
Since the symptoms of dry pericarditis include increased body temperature, general weakness, increased sweating, decreased appetite and are characteristic of the onset of most diseases. A characteristic sign of the presence of pericarditis is pericardial pain. It is localized behind the sternum. The strength ranges from insignificant to similar to angina pectoris. Manifested by tingling, burning, scratching. The pain becomes stronger when lying on the left side, when inhaling, swallowing, or coughing. It weakens when the body is tilted forward. It can radiate to the left shoulder, shoulder blade, neck, and is not controlled by nitrates.
Patients are also bothered by paroxysmal coughing and difficulty swallowing. Breathing becomes shallow, accompanied by shortness of breath. In children, hiccups are a common symptom;
A change in the nature of pain is a poor prognostic sign and indicates a transition to the exudative form of the disease. The pain resembles angina pectoris, radiating to the back and shoulder blades.
Also, depending on the cause of pericarditis, each patient may exhibit individual symptoms.
Establishing diagnosis
Diagnostic triad of fibrous pericarditis:
- ECG changes;
- Pain in the precordial region;
- Pericardial murmur.
The diagnostic algorithm includes examination, objective examination, laboratory and instrumental methods.
- Inspection. The forced position of the patient with a forward bend is revealed.
- Palpation. Local pain and swelling behind the sternum and to the left of it are determined. No displacement of the apical impulse is observed.
- Percussion. If dry pericarditis turns into exudative, a shift in the boundaries of relative cardiac dullness of the heart to the left, right and down is noted. In other cases, the boundaries are not changed.
- Auscultation. With dry pericarditis, a continuous pericardial murmur is detected by auscultation, which does not disappear after coughing and is not carried to the vessels of the neck. The noise intensifies when the stethoscope is pressed against the skin and is squeaky or “crunchy” in nature.
- Laboratory data. An increase in ESR, CRP and fibrinogen levels in the blood serum is detected. Viral etiology is characterized by an increase in lymphocytes of more than 40%. PCR is performed to determine virus antigens.
- ECG. Changes in dry pericarditis are more striking and specific than in exudative pericarditis. The following signs are revealed: Decrease in the ST segment by 5-10 mm below the isoline;
- The amplitude of the T wave is twice normal;
- In lead aVL the PR interval is shortened;
- The length of the ST segment exceeds the length of the T wave by 25% or more.
Differential diagnosis
Dry pericarditis is differentiated from:
- Exudative (by increasing the cardiac boundaries);
- Pneumonia (fluid level on x-ray, cough with purulent sputum);
- Myocardial infarction (a Q wave appears on the ECG, the pain is not relieved by analgesics);
- Tumors and injuries of the chest (detected using x-rays).
Symptoms of dry pericarditis allow one to suspect a number of diseases of other organs and systems:
- To exclude tuberculosis, a Mantoux test is performed;
- To exclude uremia, the level of creatinine and uric acid in the blood is determined;
- Autoimmune diseases are identified by the presence of rheumatoid factor, LE cells, ASL-O, and autoantibodies in the serum;
- To exclude thyroid diseases, T3 and T4 levels are examined.
All patients are tested for HIV infection and syphilis.
Diagnostics
Based on the description of the patient's symptoms, the doctor may suspect fibrinous pericarditis. To confirm the suspected diagnosis, auscultation is performed. The doctor may hear the following:
- Pericardial friction rub. It is concentrated in the region of the heart, in its lower part. The sounds coincide with the heartbeats and persist during breathing. It may become more pronounced when pressed with a phonendoscope. As a rule, when liquid appears, the noise disappears.
- Pleuropericardial murmur. It is a consequence of friction of the pleura, relatively dull and poorly audible. It is the pleuropericardial murmur that is considered the most obvious manifestation of the disease.
ECG is a method for diagnosing fibrinous pericarditis.
For the differential diagnosis of fibrinous pericarditis, other methods are also prescribed: ECHO-CG, ECG, x-ray of the sternum and others.
Pathanatomy: description of macroscopic and microscopic specimens
Fibrin accumulations are deposited between the epicardium and the inner layer of the pericardium, which form thread-like deposits. When the leaves come apart, the pathological areas are easily wounded and have a striped appearance. In this regard, the macropreparation is called “hairy heart”.
The pericardial cells are stretched and partially destroyed. Between them, accumulations of fibrin and cells are found - neutrophils, lymphocytes, platelets and fibroblasts. This phenomenon is called “cellular lymphocytic infiltration” and is characteristic of the acute stage of inflammation. In the chronic stage, connective tissue fibers, calcium deposits, and microthrombosis are found in the microslide.
Click here to see photo
Possible complications and consequences
Outcomes of dry pericarditis without therapy:
- Formation of adhesions, transition from chronic to constrictive;
- Involvement of mediastinal and pleural organs in the process (pleuropericardial fibrosis);
- Rhythm disturbances;
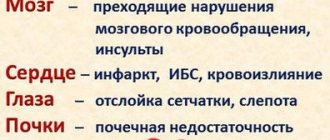
- Chronic heart failure.
Adverse effects after therapy are extremely rare. In cases where treatment was started at the wrong time, accidental injury to the heart is possible when trying to remove adhesions surgically.
Pericarditis, like most heart diseases, can lead to chronic heart failure if left untreated. This is a condition when the heart cannot pump enough blood. On the pages of our website you will find a lot of important information about the classification, main causes, prevention and relief of attacks of CHF.
Complications
If you consult a doctor in a timely manner, dry pericarditis does not cause complications. Otherwise, the disease may become more complicated:
- “Shell-hearted” (15%). A phenomenon where calcium begins to be deposited in the affected area of the pericardium, which impedes the functioning of the heart.
- Heart failure (15%). It is dangerous because the heart cannot perform its job normally, which disrupts the blood supply to all organs.
If left untreated, dry pericarditis can become constrictive (10%), then the pericardium becomes inflamed, and scar bridges form in its cavity, which will compress the heart, as well as into an exudative form with cardiac tamponade (15%).
Fibrinous pericarditis in children
Occupies 5% of all pediatric cardiac pathology. In 60% of cases, the disease has a viral etiology and develops in the cold season. Children experience long-term general symptoms (fever, intoxication), as well as dyspepsia (vomiting, diarrhea). In some cases, this lengthens the duration of therapy, but the prognosis remains relatively favorable. Mortality rate is less than 0.1%.
Find out in more detail about pericarditis in childhood from a separate material.
Treatment tactics are the same as for adults. Doses of drugs are calculated based on the age and weight of the child. For young children, it is preferable to use drugs in the form of suppositories.
Choice of treatment tactics
The goal of therapy is to reduce pain and eliminate the causative factor. Indication for treatment is diagnosis of “Dry pericarditis”.
Indications for hospitalization:
- Pregnancy;
- Childhood;
- Fever;
- Severe pain syndrome;
- Persistent tachycardia;
- Rhythm disturbances.
The following groups of drugs are used in therapy:
- Anti-inflammatory drugs (NSAIDs) - diclofenac, ibuprofen, aspirin, ketorol, indomethacin. If they are ineffective, they are replaced with colchicine or used in combination with NSAIDs;
- If colchicine is ineffective, hormones (prednisolone) are added to therapy;
- Auxiliary agents – interferon, cycloferon, anaferon, viferon.
Invasive treatment is rarely performed. The indication for this is long-term resorption of fibrin deposits. To remove them, a puncture of the pericardium is performed, during which its cavity is cleared of fibrin and washed with antiseptic solutions.
Treatment table No. 10 is assigned. The diet is aimed at reducing the consumption of salt and animal fats, as well as replenishing protein deficiency. The daily calorie content of food is 2500 kcal.
Bed rest. Children and pregnant women are treated in a hospital until complete recovery. The remaining patients, with clinical improvement, switch to outpatient treatment.
Lifestyle does not change after suffering from the disease. Working capacity is rarely reduced, only in the case of secondary complications.
Treatment and observation of the patient
Fibrinous pericarditis requires complex treatment – etiotropic and symptomatic. It should be carried out in a hospital, since regular monitoring of the level of arterial and venous pressure and heart rate is necessary. Also, such patients need repeated ECHO-CG for timely diagnosis of the possible transition of the disease to an exudative form.
Such patients need diet, vitamins, moderate exercise and immunomodulators to correct the body’s immune state.
Drug therapy consists of taking non-steroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids. The following may also be prescribed:
- narcotic analgesics - in the presence of severe pain,
- antibiotics - if the disease is bacterial in nature,
- acetylsalicylic acid - if pericarditis formed against the background of myocardial infarction.
The use of anticoagulants is contraindicated due to possible bleeding in the pericardial cavity.
In most cases, NSAIDs are prescribed. Glucocorticoids are needed in the following cases:
- with allergic pericarditis caused by taking medications;
- with pericarditis of autoimmune origin.
The dose of GCS is selected depending on the cause and complexity of the disease. You should avoid taking them if you have a viral etiology of pericarditis.
For tuberculous pericarditis, GCS is prescribed in combination with anti-tuberculosis drugs. In this case, the patient is managed by a phthisiatrician.
If a patient develops heart failure due to pericarditis, it is necessary to prescribe treatment with diuretics in combination with a cardiac glycoside.
There are situations when drug therapy is ineffective. Then surgery is necessary to avoid the formation of adhesions between the pericardial sheets. The most effective surgical option in this case is pericardiectomy. Its essence lies in opening the chest and draining the pericardium.
Clinical guidelines
If you have characteristic symptoms, you should not resort to self-medication. It is necessary to seek help as early as possible and conduct a comprehensive examination. In the treatment of dry pericarditis, the following rules should be followed:
- The drugs of choice are NSAIDs and antivirals;
- Antibiotics are prescribed only when effusion occurs;
- The patient is provided with physical and emotional peace;
- Until the patient's condition improves, he remains on bed rest.
The ESC clinical guidelines for the diagnosis and management of patients with pericardial disease, approved in 2020, provide clear answers on how to treat pericarditis. It can be downloaded here.
Forecast
The prognosis is favorable. With dry pericarditis, cardiac tamponade never develops, and the incidence of complications does not exceed 5%. Life expectancy is unchanged. Mortality ranges from 0.1 to 2%.
Dry pericarditis is the most common form of inflammation of the heart sac. The clinical picture of the disease is largely determined by the causative factors, form and duration of inflammation. In diagnosis, the most significant methods are cardiac auscultation and ECG. Timely detection of dry pericarditis is the key to early and successful therapy to avoid common cardiac complications.