Treatment of vein phlebitis should be timely.
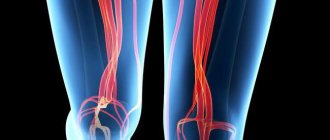
Phlebitis is an inflammatory process of the vein walls. During the development of the disease, the walls of blood vessels in the arm or leg, after a certain period of inflammation, are destroyed.
Find the answer Are you having a problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease.
The site provides reference information. Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious doctor. Any medications have contraindications. Consultation with a specialist is required, as well as detailed study of the instructions! Here you can make an appointment with a doctor.
The disease comes in acute and chronic forms.
Phlebitis often accompanies varicose veins. It appears after unsuccessful injections or the influence of pathogenic microorganisms.
Reasons for development
Post-injection thrombophlebitis can develop under the influence of the following factors:
- As a result of mechanical damage to blood vessels. A similar problem may occur after an intravenous injection or drip.
- As a result of a streptococcal infection.
- Failure to comply with basic sanitary requirements for a particular procedure.
The development of the disease can also be influenced by:
- The shape, diameter of the needle and the material from which it is made.
- Duration of stay of the needle in the vein area.
- The volume and concentration of the drug that is used for infusion into a vein.
The introduction of hypertonic solutions, which have an irritating effect on the walls of the vessel, can also cause the development of a similar problem. If a solution of doxycycline, glucose or calcium chloride is rapidly administered, the risk of developing the disease increases significantly.
It is known that the injection has a negative effect on the condition of the nerve endings, which provokes contraction of the vein. Post-injection thrombophlebitis is also accompanied by the formation of blood clots, which significantly inhibit blood flow.
Diet for phlebitis
With phlebitis, the venous wall is affected, on which harmful substances accumulate over time, so nutrition should be extremely rational. The following foods should be avoided:
- fatty, canned and smoked foods;
- carbonated and alcoholic drinks;
- fast foods;
- fresh baked goods and confectionery;
- chocolate;
- chips;
- margarine and butter.
The range of foods consumed should be increased by those that thin the blood and help avoid the formation of thrombotic masses in the lumens of blood vessels: lemon, beets, ginger root, cranberries, garlic
Manifestations
Acute and chronic course of the disease can be observed. In the chronic form of the disease, the affected vein is overly tense and provokes the development of pain. The skin at the site of inflammation may thicken and become hot to the touch. The chronic course of the disease is not accompanied by the development of any alarming processes and can be detected accidentally during the next routine examination by a doctor. As the disease becomes chronic, the risk of developing liver failure increases.
Post-injection phlebitis can begin with the development of intense pain in the area of the affected area of the vein. In this case, the patient may experience a significant increase in body temperature (up to 38.5 - 39 degrees). Treatment of the disease is selected depending on the degree of its development:
- During the first 24 hours, severe swelling develops in the area of the affected limb, which spreads to the surrounding tissues.
- Over the next few days, swelling spreads to the entire area of the limb.
- Post-injection phlebitis is accompanied by a significant deterioration in the patient’s general well-being, while his physical activity decreases.
At this stage, it is important to differentiate post-injection phlebitis from phlegmon in order to prevent premature surgical intervention. Carrying out surgery in this case significantly slows down the healing process and makes treatment expensive.
With further progression and lack of proper treatment, post-injection phlebitis provokes the following alarming symptoms:
- Severe, unbearable pain along the affected leg.
- Increased restlessness and excitability.
- There is a significant increase in the volume of the affected limb.
- The skin may become shiny and turn blue-burgundy.
- Excessive soft tissue tension is observed.
The body temperature rises above 39 degrees.
Symptoms and condition of the patient
Foci of phlebitis, after IV injections, usually appear on the surface of the veins of the upper extremities. From the very beginning of the disease, hyperemia of the skin, caused by the course of the inflammatory process, rapidly increases. It quickly spreads along the projection of the affected vein.
Thrombophlebitis develops due to alteration of vascular walls, physicochemical changes in blood composition
Upon examination, swelling of the subcutaneous tissue and soft tissues and their infiltration are determined. There is an increase in the patient's body temperature to 38-39 degrees, in addition, there is an increase and slight soreness of the regional (usually axillary and ulnar) lymph nodes. The vein has the appearance of a thickened tourniquet, reminiscent of connective tissue.
At this stage, diagnostic inaccuracies are possible, due to the similarity of the picture of phlebitis and phlegmon. If a thrombus clogs the central venous trunk, then a reflex spasm of the artery closest to it is possible, which can be taken as a manifestation of functional arterial obstruction.
Basic therapy methods
Post-injection phlebitis should be treated comprehensively: using both conservative and radical methods. If a patient has post-injection phlebitis, it is recommended to refrain from surgical intervention during the first 72 hours. Treatment at this stage comes down to antibacterial and detoxification therapy under the systematic supervision of a doctor.
Self-medication of the disease may be unsafe and may pose a threat to the patient’s life.
Drug therapy
If a patient is diagnosed with post-injection thrombophlebitis, treatment begins with the use of the following groups of medications:
- Drugs from the group of non-steroidal anti-inflammatory drugs: ibuprofen, acetylsalicylic acid, nimesulide.
- Venodynamic drugs: use of Aescusan or Troxevasin.
- In severe cases of the disease, the doctor may decide to treat post-injection phlebitis through lymphotropic administration of antibacterial drugs.
- Local therapy involves the application of ointment dressings, as well as the use of Heparin ointment and silver solution.
Post-injection phlebitis should be treated by applying semi-alcohol compresses to the affected area. If the tissue under the bandage begins to soften, this is an alarming sign indicating the development of an inflammatory process.
If post-injection phlebitis is detected at an early stage of development, then it is advisable to use hypothermic procedures. In case of severe inflammatory process, it is recommended to abstain from elements of physiotherapy.
In what cases is radical therapy required?
If thrombophlebitis festeres, treatment can be radical. Surgical intervention is required in cases where ointment compresses and the use of antibacterial agents do not provide quality treatment.
During the radical treatment procedure, the opening of the abscess is required, followed by excision of the purulent edges of the wound. The doctor makes an incision along the affected vein and ligates it. Sutures are not required in the future, as they may slow down the patient's healing process.
The recovery period after radical treatment can take several weeks.
Outcome and complications of phlebitis
The central terrible complication of phlebitis is thrombophlebitis. It occurs as a result of an increase in the thickness of the blood, which makes it difficult for it to move through the veins that are subject to destructive effects.
The accumulation of blood clots on the venous wall may be triggered, or a thrombus or embolus may form. The most terrible consequence of these modifications will be the detachment of a blood clot or embolus from the wall and circulation through the blood. As a result, it is introduced into some organs, which leads to a disastrous outcome.
Thrombophlebitis, which has passed into the stage of acute development, can be dangerous due to the manifestation of thromboembolism of the pulmonary artery, that is, clogging of the lung vessels with a detached blood clot, which disrupts the breathing process.
The companions of phlebitis will be abscesses and phlegmon. But various unfavorable outcomes and complications of phlebitis are observed when treatment is not started on time. If you consult a specialist in a timely manner, inflammatory processes in the veins are easily eliminated and do not cause undesirable consequences. The main thing is to identify the cause of the lesion, and then try to lead a healthy lifestyle and be guided by the principles of proper nutrition.
Types and causes of the disease
There are several types of diseases that occur in the veins after injection:
- periphlebitis, characterized by inflammation of the tissue that surrounds the vessel. This disease may be accompanied by thrombosis and phlebitis;
- pandeflit, which affects the membranes of the veins;
- endophlebitis, due to which the inner surface of the vein becomes inflamed when the vessel has been injured or has become infected.
Solutions quite often cause post-injection thrombophlebitis, because irritation of the vessel walls occurs. For example, if an infusion of doxycycline, hydrochloride, potassium chloride, or glucose occurs quickly enough, this is fraught with the development of complications.
The post-injection complication is due to the fact that during the injection of the solution there is a very high chance of a spasm occurring, which is the result of a violation of the nerve endings.
Spasms also provoke a narrowing of the distance between the veins and inflammation in the tissues. Sometimes the blood slows down, which can cause blood clots to form.
Sometimes post-injection thrombophlebitis develops at home, which is caused by the following factors:
- Stopping binge drinking.
- Urgent detoxification.
- Self-injections.
Such reasons first cause endophlebitis, so if you try - whether successful or not - to install IVs at home, you must go to the hospital.
This will help avoid progress in the development of the disease and the occurrence of complications.
Why does post-injection phlebitis develop?
The disease appears against the background of a violation of the integrity of the venous wall during the installation of a catheter. But this does not mean that every such manipulation ends in inflammation of the vessel. Post-injection phlebitis occurs in the presence of the following risk factors:
- installation of a catheter for a long period;
- incorrect calculation of the dose of medication administered through the catheter;
- non-compliance with the principles of asepsis and antisepsis;
- use of cheap, low-quality medical instruments;
- rapid administration of medication.
Often, phlebitis of the veins in the arm after a catheter is provoked by self-installation of a medical device at home. Patients who do not have experience in carrying out such manipulations rely on their own strength and ignore the sequence of actions, principles of disinfection and other nuances.
Diagnostics
Only a doctor can determine whether a patient has developed a disease in the veins after an injection. To do this, a comprehensive study of the patient is carried out. First, the emphasis is on examining the clinical signs. Secondly, conducting a histological examination. It helps to detect whether cells in smooth muscle have been replaced by so-called fibrous tissue. Thirdly, taking tests to understand what type of post-injection thrombophlebitis doctors need to deal with.
Doctors pay special attention to those patients whose disease began to develop after surgery. The most dangerous is pulmonary thrombophlebitis, which results in pulmonary embolism. It is very difficult to diagnose and treat.
The easiest way to treat a disease that occurs as a result of mechanical damage to the veins, their walls, and inflammation that can be observed there. But this must be done before the disease spreads to the veins of the arms and legs, which is a fairly common occurrence with venous thrombophlebitis.
Causes and diagnosis
Post-injection and post-infusion phlebitis can develop after injury to the vessel walls by catheters installed for infusions, injections and droppers. The extent and nature of the damage depend on many factors:
- the material from which the catheter is made;
- needle length and diameter;
- duration of stay in the vein;
- volume and concentration of the infused solution;
- compliance with sanitary rules.
The cause may be hypertonic concentrations of substances administered through a dropper that irritate the walls of the vessel. When a solution of doxycycline hydrochloride, calcium and potassium chloride, 40% glucose solution and other substances is administered at high speed, there is an increased risk of developing such complications.
After administration, a spasm often occurs caused by a violation of the nerve endings, a narrowing of the lumen of the vein, and the development of an inflammatory process. At this stage, due to slowing blood flow, a blood clot may form.
Post-injection phlebitis often develops during out-of-hospital interventions - when using a drip to stop binge drinking at home, during urgent detoxification measures, including IV injections during suicide attempts, in drug addicts after injections of aggressive drugs.
In such cases, endophlebitis occurs initially, in which the internal lining of the vessel is affected; in the future, the process may progress and severe complications may develop.
Diagnosis is made based on clinical signs. An important link in making a diagnosis is a histological examination, which reveals the replacement of smooth muscle cells with fibrous tissue. This picture is typical for chronic phlebitis, originating from post-injection.
Features of treatment
Therapy depends on the type of disease and the severity of the disease. Most often, a conservative treatment method is used for thrombophlebitis. Firstly, the patient is prescribed non-steroidal drugs, which include Ibuprofen or Nimesulide. Secondly, drugs to fight bacteria. Thirdly, anticoagulants are used. Fourthly, bandages impregnated with drugs containing a high level of silver are applied.
If the veins are not severely affected, but only their surface, then the pain syndrome is first relieved, and then the main type of treatment is carried out. But with an extensive course of the disease, which is accompanied by bacterial infections, treatment may include the following methods:
- Elimination of puffiness.
- Increasing lymph circulation in the blood and veins.
- Elimination of spasms and hypertonicity of the walls of blood vessels.
- Fighting blood clots and their formation.
- Increased blood flow through the veins.
- Relief of inflammation.
Ointments that contain the substances heparin and troxevasin can be applied to areas of inflammation; they can significantly reduce the course of the disease and increase the flow of blood through the veins. Trental is also prescribed simultaneously with these drugs to prevent the formation of blood clots.
Patients who have been diagnosed with thrombophlebitis are hospitalized for several weeks for inpatient treatment. This reduces the risk of developing various forms of embolism and liver failure. Doctors strictly prohibit self-medication so as not to cause serious harm to health and life. After treatment, patients are prescribed preventive measures, as well as undergoing a mandatory medical examination 2 times a year. At the same time, people should normalize their lifestyle by removing factors that can cause spasms or blood clots.
Intravenous injections are a procedure performed dozens of times daily in most medical settings. Even such a simple intervention can cause a number of complications. It is worth considering why post-injection phlebitis occurs, what the symptoms of this condition are, and what treatment should be given.
What and how to treat
Treatment of phlebitis is complex. The treatment regimen depends on the causes of inflammation. If superficial veins are affected, care is provided on an outpatient basis. In more severe cases, hospitalization is required. The main methods of treating this vascular pathology are:
- Elimination of the root cause (treatment of the underlying disease).
- Providing peace.
- Giving the limb an elevated position (effective for damage to the blood vessels of the legs).
- Physiotherapy (UHF therapy, acupuncture, reflexology, mud baths, magnetic therapy, infrared irradiation).
- Normalization of venous blood viscosity.
- Use of medications.
- Wearing compression stockings. Required after acute symptoms disappear. This knitwear allows you to create pressure on the inflamed vessel and normalize the outflow of blood. Compression tights, stockings and socks are used. An alternative is elastic bandaging of the limb.
- Wearing special orthopedic shoes. It is required if a vein in the leg in the foot area is inflamed.
- The use of traditional medicine.
- Local procedures (dressings with heparin ointment). Indicated for thrombophlebitis.
- Therapeutic physical education (physical therapy). Effective for concomitant varicose veins of the legs.
- Detoxification. Indicated for severe forms of the disease (pylephlebitis). Therapy after the drip is continued.
- Complete nutrition.
- Surgery and minimally invasive procedures.
Surgery
If phlebitis develops, treatment may include surgery. If the portal vein is inflamed due to appendicitis or inflammation of the gallbladder, cholecystectomy and appendectomy are required. For phlebitis of the superficial veins, surgery is most often not required. In other cases, the following interventions can be performed:
- Troyanov-Trendelenburg operation (indicated for ascending thrombophlebitis);
- sclerotherapy;
- laser intervention;
- phlebectomy and miniphlebectomy (performed for varicose veins).
Drug therapy
The following medications are used in the treatment of phlebitis of the lower extremities:
- Antibacterial agents. Indicated for tissue suppuration.
- NSAIDs (Ketonal, Ketoprofen, Flamax Forte). Effective for inflammation of the veins in the arm or leg with severe pain.
- Local drugs (Voltaren, Dolgit, Indovazin).
- Venotonics (Phlebofa, Vazoket, Phlebodia 600, Phlebaven, Troxevasin, Troxerutin, Detralex, Venarus).
- Antihistamines (Suprastin, Tavegil). Indicated for allergic nature of phlebitis.
- Drugs that normalize microcirculation (Pentoxifylline, Trental).
- Neuroprotectors. Indicated for cerebral form of the disease.
- Anticoagulants and antiplatelet agents (Curantil, Cardiomagnyl, Thrombo Ass, Heparin, Clopidogrel). Reduce blood viscosity, increasing its fluidity.
- Local drugs effective for thrombosis (Heparin ointment).
It is necessary to treat phlebitis with medications taking into account their tolerability and contraindications.
Traditional medicine
For phlebitis of the veins in the arm, treatment may include the use of traditional medicine in the form of compresses, lotions, decoctions and infusions. The most commonly used:
- a mixture based on arnica oil and vinegar (applied to intact skin);
- oak bark (you can make a decoction from it for oral administration);
- ginkgo biloba infusion;
- infusion of horsetail (taken orally);
- pineapple pulp;
- decoction of hop cones;
- infusion based on clover and sweet clover leaves.
For inflammation of the veins, treatment with folk remedies is an addition to drug therapy. It is carried out with the permission of the attending physician.
Diet
If there is inflammation in the vein area, then you need to stick to a diet. It is necessary to enrich the menu with products that thin the blood and strengthen blood vessels (seaweed, citrus fruits, tomatoes, currants and other berries, seafood, onions, garlic, fermented milk products and nuts). It is necessary to limit the consumption of watercress, spinach, kale and liver, as they are rich in vitamin K (it helps to increase blood clotting).
Why does it occur
Post-injection thrombophlebitis is inflammation of the venous wall as a result of improper placement of a drip, catheter or other intravenous intervention. Phlebitis after an injection can be triggered by a drug that was administered too quickly or to which the body reacted too aggressively.
This disease has been assigned a code according to ICD-10 – “I80”. This data is necessary for the doctor to enter information into the outpatient card.
Post-injection phlebitis on the arm can be caused by the following reasons:
- Mechanical damage to the vein;
- Infection;
- Failure to comply with sterile standards for manipulation;
- Needle too wide;
- Excessively large volume of drug injected into a vein;
- Prolonged stay of the catheter in the vein;
- High concentration of active ingredients in the injection solution.
Thrombophlebitis is a post-injection complication that occurs against the background of the formation of blood clots due to slowing of blood flow as a result of venous inflammation. When the skin and veins are punctured, the nerve endings react. They cause contraction of the vascular muscles, which also increases the risk of blood clots.
The risk of infection through a catheter is higher when placing IVs at home, both when calling an ambulance, and when the patient independently withdraws from a drinking binge.
Clinical picture of vessel wall rupture
When a blood vessel is injured, blood enters the surrounding tissue, which leads to the appearance of characteristic symptoms of hemorrhage. Bruises after an injection in the buttock may be accompanied by the appearance of lumps in the soft tissues. The main signs of hematomas and bruises on the body are:
- redness at the injection site, which over time changes its shade from yellowish to bluish;
- the appearance of a thickening on the skin at the site of the bruise;
- soreness at the injury site.
Post-injection, or post-infusion, phlebitis is an inflammation of the venous walls, which is a complication of intravenous injection or infusion.
Among all types of vascular pathology, post-injection phlebitis is recognized as the most common form.
Administration of the drug through a vein causes vasospasm, provoking a narrowing of the venous lumen, as well as the penetration of infection, and leads to inflammation of the vein walls. This process is accompanied by a significant slowdown in blood circulation, deterioration of chemical indicators of blood composition, thinning of the tissues of the vascular walls, the formation of stagnation, and the detection of infectious agents in the plasma. All this increases the risk of blood clots, leading to a serious complication of phlebitis - thrombophlebitis.
Phlebitis caused by infusion is characterized by the following types:
- periphlebitis - inflammation of the subcutaneous tissue at the site of vessel damage;
- panphlebitis - damage to all venous layers;
- endophlebitis is a pathological change in the inner choroid.
Typically, inflammation of the veins after injection is localized on the arms or lower legs, but phlebitis can develop on any part of the body.
Post-injection phlebitis is formed due to damage to the vein during an intravenous injection or a catheter installed for infusions.
The risk of developing phlebitis depends on many factors. The main ones among them are the following:
- the size (length and diameter) of the needle through which the medicine was administered;
- use of low-quality raw materials for the manufacture of catheters and syringes;
- installation of a device (catheter) for a long time;
- failure to comply with sanitary standards during the procedure;
- ignoring aseptic rules;
- incorrectly calculated dose and high concentration of the administered drug;
- infection (candida, streptococci, staphylococci) due to failure to maintain sterility.
After a catheter has been in the vein for a long time, there are frequent cases of infection, which further complicates the inflammation and course of phlebitis.
According to statistics, the development of phlebitis on the arm is most often provoked by self-installation of IVs at home (when removing patients from a drinking binge, ignoring hospital treatment, during urgent emergency care, etc.). Also at risk are people with drug addiction, who very often inject in places that are far from sterile. In such cases, the process of inflammation usually begins with damage to the inner layer of the vessel (endophlebitis) with further progression of the pathology.
Symptoms
Post-injection phlebitis of the vein manifests itself within several hours or even days after intervention in the venous bed. The disease is manifested by the following symptoms:
- Thickening of the vein at the injection site;
- Pain when trying to perform an action;
- Hardening of soft tissues at the injection site;
- When you try to touch, a sharp throbbing pain occurs;
- The injection site swells;
- Hyperemia develops within a day.
The surrounding tissues are also subject to a pathological process. The swelling decreases only after a few days. Gradually, the area where the injection was performed becomes burgundy, then turns blue.
If the patient does not receive proper care at this stage, serious complications will develop.
After a few days, post-infusion phlebitis manifests itself with even more aggressive symptoms:
- The limb ceases to freely extend and bend at the joint;
- The surface of the skin turns red;
- Body temperature rises to critical levels;
- The lymph nodes become enlarged and painful.
If help is not provided, infiltration of the vascular walls begins. Suppuration occurs. Closely located arteries are involved in the process.
Treatment of post-injection phlebitis in an advanced stage is carried out only by surgery. But timely therapy makes it possible to avoid surgery.
Visually, it is impossible not to notice the manifestations of phlebitis after a catheter or an unsuccessful intravenous injection. In the photo you can see what this pathology looks like.
Phlebitis of the veins on the arm after a catheter and injections
In drug therapy, doctors prefer to use intravenous administration of various drugs. This is due to the fact that thanks to this method you can get a quick and necessary result. However, quite often after a catheter, which is placed for ease of drug administration, there is a risk of phlebitis.
Phlebitis on the arm after a catheter is an inflammatory process; it is localized on the walls of the veins as a result of their traumatic effects during the treatment of a certain disease. If this condition is not treated, then after some time the damaged vessels will begin to collapse.
So, what is phlebitis, why the veins become inflamed and what therapeutic measures are used in this case.
What is vein phlebitis?
Phlebitis of the vein in the arm occurs not only due to the catheter, but also after any perforation of the vein: intravenous injection, infusion, that is, the placement of a drip. Among the many inflammatory processes occurring in blood vessels and diseases associated with them, post-injection phlebitis is considered the most common form.
Principles of post-injection phlebitis
When a medicine is injected into a vein, vasospasm occurs, which provokes favorable penetration of the infection. These actions can lead to inflammation in the vascular walls.
Then blood circulation slows down a little, blood chemical parameters deteriorate, the walls of blood vessels become thinner, congestion forms, and infectious agents are found in the plasma.
The likelihood of blood clots increases significantly, which is a serious complication of the disease - thrombophlebitis.
Phlebitis that occurs after an IV drip has several varieties:
- periphlebitis (when the subcutaneous tissues become inflamed along with the damaged vein);
- panphlebitis (all venous layers are damaged);
- endophlebitis (characterized by changes occurring inside the vein).
Symptoms of the disease and the patient’s feelings
Phlebitis usually manifests itself within 24 hours after intravenous administration of the drug. The patient experiences redness at the site of the catheter or injection. It is removed with a catheter. However, the inflammatory process may continue to worsen and be accompanied by the following symptoms:
- due to the accumulation of blood at the injection site, the veins thicken and protrude outward;
- soft tissues thicken, which becomes noticeable upon palpation;
- severe pain occurs that radiates to the fingers;
- the hand swells (and several hours after the injection), severe swelling appears;
- blue discoloration of the affected area;
- The elbow and axillary lymph nodes are noticeably enlarged.
The patient's condition continues to deteriorate, the body temperature rises, and on the 3-4th day the limb stops bending and straightening at the elbow joint. If treatment is not started, the pathology will begin to spread to the adjacent vessel. Suppuration of the venous walls is also possible.
Therapy methods
Treatment of phlebitis after injections into a vein, as well as infusions, is carried out using conservative methods. In complex or advanced situations, they resort to a radical method of therapy - surgery.
The type of treatment depends primarily on how much time has passed since the onset of the inflammatory process. If the patient consults a doctor at 1-3 knocks, then drug therapy is still applicable. But in any case, immediate treatment of post-injection phlebitis is necessary, otherwise sad consequences cannot be avoided.
Drug treatment of phlebitis
To reduce the risk of possible complications, post-injection phlebitis must be treated at the first signs of pathology. Conservative treatment methods consist of the following:
- use of non-steroidal anti-inflammatory drugs;
- antibacterial agents are used to prevent blood poisoning;
- To reduce blood viscosity and prevent the formation of blood clots, the patient is prescribed anticoagulants.
In the first stages of phlebitis on the arm, you only need to relieve pain and relieve inflammation. If the process lasts a long time and a bacterial infection occurs, then complex treatment is used.
In addition to internal administration of drugs, external treatment is used: ointments and gels containing heparin and troxerutin. These agents reduce inflammation and improve venous patency.
Traditional methods of treatment
Alternative medicine, namely ointments and compresses, actively helps to speed up the healing process for phlebitis.
There are several of the most effective folk remedies for the treatment of inflammation of the veins:
- Honey compress. Take honey, apply a thin layer of it to the inflamed area and fix with a cloth.
- Cabbage leaf. As you know, cabbage leaves can relieve inflammation. Wash the cabbage leaf, scald it with hot water, spread with honey and apply to the problem area.
- Iodine network. Today, it is difficult for doctors to explain the fact that a banal iodine network can relieve inflammation and pain.
- Alcohol compress. You need to soak a piece of cotton wool in alcohol and apply Vaseline on top. Place the prepared compress on the affected area of skin and secure it with a bandage.
Traditional therapy can only be used as an additional treatment; it does not replace medication, in particular when it comes to the acute form of the disease.
In what cases is radical therapy required?
If drug therapy does not give positive results in the fight against phlebitis and the disease lasts for a long time, then surgical intervention would be a reasonable solution. This occurs when the affected area is inflamed, suppuration begins, blood clots form, and post-injection thrombophlebitis occurs.
The operation is performed in a hospital setting. Under local anesthesia, the patient has the resulting suppuration removed. The next day after surgery, it is recommended to wrap your arm with an elastic bandage and try not to disturb the limb.
If phlebitis, especially its acute form, is not treated, a complication of the inflammation process (for example, blood poisoning) may occur and lead to death.
Diet for phlebitis
With phlebitis, the venous wall is affected, on which harmful substances accumulate over time, so nutrition should be extremely rational. The following foods should be avoided:
- fatty, canned and smoked foods;
- carbonated and alcoholic drinks;
- fast foods;
- fresh baked goods and confectionery;
- chocolate;
- chips;
- margarine and butter.
The range of foods consumed should be increased by those that thin the blood and help avoid the formation of thrombotic masses in the lumens of blood vessels: lemon, beets, ginger root, cranberries, garlic
Preventive measures
Every person should take their health seriously: eat rationally, lead a healthy lifestyle, and take timely preventive measures for existing chronic diseases. As preventive measures for vascular pathologies, doctors recommend:
- walk in the fresh air in any weather;
- give up all bad habits;
- play sports and live according to the regime;
- eat rationally;
- do not forget to lubricate the place where the needle is inserted with venotonics if you are undergoing treatment using intravenous injections or infusions.
A frivolous attitude towards phlebitis is fraught with serious consequences. Any suspicion of venous inflammation is a reason to consult a doctor. If measures are taken in time, the patient’s complete recovery will be guaranteed.
Source: //venaz.ru/bolezni/vospalenie-ven/flebit-ven-ruk
Diagnostic measures
If thrombosis occurs after the injection, it is important to see a doctor immediately. A phlebologist treats vascular diseases. He will be able to make a preliminary diagnosis after examination, but to confirm the pathology and differentiate it from other disorders, the following procedures are required:
- General blood analysis;
- Coagulability test;
- X-ray of a limb with post-injection phlebitis;
- Ultrasound of the vein at the site of inflammation.
A thorough examination of the affected tissue area will allow the doctor to verify the correctness of the diagnosis and select adequate treatment. Only competent therapeutic methods can prevent the development of severe complications.
How does pathology manifest itself?
Phlebitis after intravenous drip or catheterization of veins manifests itself within 24 hours after the procedure and is accompanied by the following symptoms of venous inflammation:
- thickening due to the accumulation of blood at the injection site and protrusion of the vein outward (appears 2-3 hours after the injection;
- pain when moving a limb;
- stiffening (hardening) of soft tissues, detected upon palpation;
- the appearance of a sharp throbbing pain radiating to the fingers, shoulder, thigh (depending on where the injections were given);
- swelling and swelling of the injection area (appears after a few hours);
- redness of the affected area after 24 hours, followed by the appearance of a burgundy tint and blue discoloration;
- increasing swelling on day 2, swelling of the affected area, including surrounding tissues.
Ignoring the above symptoms of phlebitis leads to the fact that on the 3-4th day the limb stops bending/unbending at the knee/elbow joint, hyperemia and infiltration of the vascular walls develops, and body temperature increases (after some time it can reach 39-40°C).
In the future, the signs of venous inflammation only intensify:
- lymph nodes in the armpits and elbows become inflamed;
- suppuration of the walls of blood vessels forms, affecting nearby arteries.
With such an advanced stage of phlebitis, an operation to excise the pus is prescribed.
Read also: Hemorrhoidal thrombophlebitis
In addition, post-infusion phlebitis occurs against a background of general malaise, a noticeable decrease in physical activity, and pronounced pain.
Principles of treatment
In most cases, patients seek help in the initial stages of inflammation due to the formation of a blood clot. Thanks to this, conservative treatment can be used.
To avoid having to undergo surgery, treatment should begin within the first three days after the onset of post-injection phlebitis.
Conservative treatment tactics
The initial stages of post-injection thrombophlebitis can be treated with medication. Veins are restored if the drugs are correctly selected and used regularly.
The goals of drug treatment are as follows:
- Stop the inflammatory process;
- In case of infection, neutralize its effect;
- Restore normal blood circulation in the limb;
- Return the venous walls to their previous integrity.
Drugs prescribed for the treatment of post-injection phlebitis help reduce blood viscosity, reduce inflammation and pain. Treatment at the initial stages of pathology consists of the use of the following medication groups:
- Nonsteroidal anti-inflammatory drugs (NSAIDs);
- Medicines to strengthen the venous wall and speed up blood circulation;
- Anticoagulants;
- Fibrinolytics;
- Antibiotics.
The drugs can be used orally, intramuscularly, intravenously and even endolymphatically. The latter method allows you to quickly create the necessary concentration of the therapeutic substance in the affected tissues. NSAIDs can be used in the form of gels. Many doctors also advise using Heparin and Troxevasin ointments topically.
Local compresses
The effectiveness of general therapy can be increased by applying compresses. The following tools can be used for this procedure:
- Colloidal silver solution;
- Silver-based ointments (Arghedine);
- Heparin;
- Alcohol solutions.
Such procedures can be carried out if the inflammatory process has begun to subside. Warming compresses are not applicable if the pathology occurs in an acute form.
Any preparations containing silver should be used when a bacterial infection is associated, since this substance is a powerful natural antibiotic to which bacteria are unable to develop resistance.
Surgery
Surgical intervention is indicated if conservative therapy has proven ineffective. The operation is also prescribed in cases where the patient sought help late, and the vein in the limb had time to fester. In this case, surgical intervention is necessary to save the person’s life, since the penetration of pus into the blood will cause sepsis, and even death.
The operation is performed under local anesthesia. Rehabilitation after the intervention takes several weeks. During the recovery stage, the limb must be wrapped with an elastic bandage. Most of the time the limb needs to be raised to body level.
In some situations, your doctor may prescribe physical therapy. However, such procedures are not carried out during the acute period of inflammation and after surgical incisions are made.
Timely treatment of post-injection phlebitis can avoid complications and save a person’s life. The sooner therapy is started, the safer the patient will be.
Source: gribkovnet.ru
Traditional methods of treatment
To speed up the recovery process for post-injection phlebitis, alternative medicine is often used - ointments and compresses based on components of plant origin. However, treatment of inflammation of the vascular walls can be carried out only after consultation with a doctor and testing for the absence of an allergic reaction.
We suggest using the most effective recipes that relieve venous inflammation:
- Honey compress. Lubricate the area of inflammation with liquid honey and wrap it with natural fabric (linen, chintz).
- Applying cabbage leaf. Crumple a cabbage leaf thoroughly washed and scalded with boiling water, spread with honey and apply to the site of inflammation. Secure with a bandage.
- A decoction of beet tops relieves inflammation well. Pour 50 g of dried red beet leaf into 1 liter of boiling water. Let it brew for an hour. Take 150 ml of infusion in the morning on an empty stomach.
- A decoction of currant or rowan leaves. Take the raw material brewed using the above method for venous inflammation 2-3 times a day, 100 ml.
Please note that traditional medicine for inflammation of the vascular walls after injection are additional preventive measures and cannot replace the main treatment of phlebitis with medications.
Sister
Complications after intramuscular injections
05.29.2012 | Author: Sestra
The nurse must clearly understand what complications may occur after intramuscular injections and how to avoid them. If complications arise, the nurse must know the algorithm of medical care for the patient.
So, complications after intramuscular injections may be as follows.
Needle breakage
Not often, but it does happen. The reason is strong muscle contraction due to fear of the procedure, unexpected start of injection, or improper psychological preparation of the patient.
Help: keeping calm, reassure the patient, assure him that everything will be fine. With the 2nd and 2nd fingers of your left hand, press down the tissue on both sides of the broken needle, squeezing it out in this way. Take tweezers with your right hand, carefully grab the tip of the fragment and remove it. The action is repeated several times. If attempts are unsuccessful, urgently call a doctor through an intermediary, remaining with the patient and reassuring him. In the future, follow all the doctor’s instructions.
Damage to the periosteum
Can occur when giving an intramuscular injection with a needle that is too long in a thin patient. Help: referral to a surgeon and implementation of his instructions. Prevention: correlate the length of the needle with the size of the patient’s subcutaneous fat layer at the site of the intended injection.
Traumatization of nerve trunks
Such complications after intramuscular injections can occur when the needle is inserted not into the upper-outer quadrant of the buttock, but, for example, into the lower-outer one. Nerve trunks can also be damaged when the drug acts directly on the nerve tissue. This happens if the drug is injected near the location of the nerve.
Help: referral to a doctor and explanation to the doctor of all the circumstances of the injection.
Infiltrates
Reasons: rapid administration of the drug, low temperature of the administered drug, insufficient needle length, injections into areas located next to a recently made injection or with old infiltrate.
Help . applying a semi-alcohol compress or the same with the addition of a 25% solution of magnesium sulfate, informing the attending physician.
Abscesses
Reasons: non-compliance with the rules of asepsis and antisepsis, injections into infiltrates, intramuscular injections using a short needle.
Help: urgent referral to a surgeon.
Hematomas
Causes: damage to blood vessels from a needle.
Help: referral to a doctor and fulfillment of his appointments.
Emboli
Oil and suspension embolisms occur when a needle enters the lumen of a blood vessel with subsequent administration of a drug. If there is insufficient air displacement from the syringe, there is a risk of an air embolism if the entire contents of the syringe are injected into the blood vessel where the needle entered.
Help: place the patient in a lateral position with the head raised, immediately call a doctor through an intermediary.
Prevention: complete displacement of air from the lumen of the syringe, “pulling back” the piston when the needle is inserted with the intention of introducing oil or suspension solutions.
Thrombophlebitis and necrosis
Such complications after intramuscular injections are rare, but they do occur. Thrombophlebitis occurs when blood vessels are damaged, often multiple times, followed by necrotization of soft tissues.
Help: if the patient complains of severe pain and the presence of hematomas, immediately consult a surgeon.
Infection with HIV, parenteral hepatitis
Reasons: gross violation of the rules of asepsis and antisepsis when administering intramuscular injections, including hand washing, pre-sterilization cleaning and sterilization of instruments.
Prevention: strict adherence to all existing regulations and sanitary standards when carrying out invasive manipulations.
Allergic reactions
When any drug is administered, the patient may experience an allergic reaction from urticaria to anaphylactic shock . The treatment room should be equipped with an anti-shock first aid kit and instruments to assist in respiratory arrest.
Knowing the possible complications after IM injections, the nurse should make every possible effort to prevent them. And if any complication arises, be ready to take the necessary actions on your part.
More interesting things on the site:
Source: heal-cardio.ru
Causes
Post-injection thrombophlebitis, as a rule, is a complication of compression sclerotherapy if the technique of this procedure is not followed.
If local compression of the vein in the area of sclerosant injection or weak elastic compression is insufficient, the vessel may become inflamed. As a result, a blood clot often forms in the lumen of the vein, which poses a threat of pulmonary embolism.
To prevent the development of such problems, special adhesive bandages and latex or foam rubber pillows are used.
An example of the occurrence of such a complication, which is caused by insufficient compression of the vein, is the occurrence of so-called intravenous hematomas.
In appearance, they resemble dense areas of veins, which cause pain and resemble thrombosed vessels. In the lumen of such veins there is a tar-like mass, which includes a mixture of blood and sclerosant.
If measures are not taken in time, intravenous hematomas can lead to the development of acute thrombophlebitis. Through the use of local compression and ointments containing heparin, it is possible to achieve gradual resorption of hematomas.
Sometimes a special puncture helps speed up the process. This procedure removes the mass that is present in the lumen of the vein.
In what cases is radical therapy required?
If drug therapy does not give positive results in the fight against phlebitis and the disease lasts for a long time, then surgical intervention would be a reasonable solution. This occurs when the affected area is inflamed, suppuration begins, blood clots form, and post-injection thrombophlebitis occurs.
The operation is performed in a hospital setting. Under local anesthesia, the patient has the resulting suppuration removed. The next day after surgery, it is recommended to wrap your arm with an elastic bandage and try not to disturb the limb.
If phlebitis, especially its acute form, is not treated, a complication of the inflammation process (for example, blood poisoning) may occur and lead to death.
Symptoms
The first manifestation of post-injection phlebitis is acute pain, which is localized in the area of the affected vessel. At the same time, body temperature increases significantly and the general condition of a person greatly worsens.
On the first day after the onset of the disease, severe swelling of the limb develops in the girth. As the disease progresses, it covers an increasingly larger area.
After 3 days, soft pasty edema develops, which affects the hand and forearm. At this stage, it is very important to make a correct diagnosis. This will avoid surgical intervention if phlebitis is mistaken for phlegmon of the veins of the extremities, which are superficial.
The most severe type that post-injection thrombophlebitis of the hand can have is periphlebitis.
Often the pathology is the result of withdrawal syndrome. In this situation, the person experiences increased anxiety and complains of severe pain in the limbs. These symptoms make it difficult to make an accurate diagnosis.
In such a situation, in addition to the distinctive symptoms of the disease, you should pay attention to additional manifestations:
- skin redness;
- partial doubling of limb size;
- local tension of muscle tissue.
After 4 days, the tissue in the affected area acquires a softer consistency, and fluctuation is observed.
The appearance of a blood clot in the central trunk of a vein can lead to a reflex spasm of the artery that is located nearby. In such a situation, the patient may be misdiagnosed, namely acute arterial obstruction.
Symptoms of the disease
The first signs of inflammation appear in the first 24 hours; the symptom complex includes the following changes:
- pain when bending, straightening or turning the arm, radiating to the fingertips and shoulder;
- compaction of tissues located near the site of placement of the venous catheter;
- change in skin color from slight redness to a burgundy or bluish tint;
- increase in tissue edema.
In the absence of adequate therapy, on the third or fourth day the patient is unable to move his arm due to severe pain. Body temperature rises to 39-40°C, complaints of headaches, weakness, fatigue, and chills arise.
After a week, if the course of phlebitis is unfavorable, inflammation covers not only nearby tissues, but also switches to the axillary lymph nodes. The walls of the affected vein become suppurated, which requires surgical intervention.
Diagnostics
First of all, the doctor must palpate the affected vein. As a result of the examination, an infiltrate may be detected, which indicates that the inflammatory process has spread to a large area of subcutaneous tissue.
In addition, blood and urine tests have high diagnostic value.
If necessary, radiography and ultrasound examination may be performed. In order for the doctor to be able to make an accurate diagnosis as quickly as possible, he must have a complete medical history of the patient.
Also important is the study of the vessels of the lower extremities - rheovasography.
Treatment of post-injection thrombophlebitis
In most cases, to eliminate post-injection thrombophlebitis, conservative therapy is used, which includes the following components:
- treatment with non-steroidal anti-inflammatory drugs - these include Ibuprofen, Nimesulide;
- use of anticoagulants;
- use of antibacterial drugs;
- local treatment - in particular, dressings using silver preparations.
If a more serious process occurs, which is complicated by a bacterial infection, complex treatment is indicated.
It should solve the following tasks:
- stop inflammation;
- eliminate spasm and increased tone of the vascular wall;
- increase venous blood flow;
- reduce blood viscosity;
- cope with the formation of blood clots;
- stabilize the tone of smooth venous muscles;
- eliminate swelling and improve lymph circulation.
Non-steroidal anti-inflammatory drugs are used to treat the inflammatory process. They can be used either orally or in the form of ointments. Preference should be given to new generation non-steroidal drugs. However, in addition to this, drugs such as Butadione, Nimesulide, etc. are successfully used.
If an infection occurs, it is necessary to determine the type of pathogen and prescribe antibacterial treatment. Medicines can be administered by the endolymphatic route. Due to this, it is possible to increase their content in the source of infection.
Ointments containing substances such as Heparin and Troxevasin should be applied to the site of inflammation. They help reduce inflammation and improve vascular permeability. To prevent the formation of blood clots, Trental and other modern medications are used.
Therapy of thrombophlebitis with intravenous injections and infusions should be carried out exclusively in a hospital setting. This is associated with the risk of serious complications - thromboembolism or phlegmon.
If phlebitis becomes chronic, there is a risk of liver failure. That is why it is so important to carry out adequate therapy in a timely manner for any conditions that are caused by damage to the veins or intravenous administration of drugs.
Self-medication of phlebitis that appears in the area of intravenous injections is very dangerous. It poses a threat not only to human health, but also to human life. That is why it is so important to consult a doctor in a timely manner.
People who have suffered from this pathology or are at risk need to make adjustments to their lifestyle. They need to combine relaxation with walking. It is very important to stop smoking and eliminate any factors that can lead to vasospasm.
Phlebitis of the vein on the arm: after the catheter, treatment, inflammation
Treatment of vein phlebitis should be timely.
Phlebitis is an inflammatory process of the vein walls. During the development of the disease, the walls of blood vessels in the arm or leg, after a certain period of inflammation, are destroyed.
Are you having any problem? Enter “Symptom” or “Name of the disease” into the form, press Enter and you will find out all the treatment for this problem or disease. The site provides reference information.
Adequate diagnosis and treatment of the disease is possible under the supervision of a conscientious doctor. Any medications have contraindications.
Consultation with a specialist is required, as well as detailed study of the instructions! Here you can make an appointment with a doctor.
The disease comes in acute and chronic forms.
Phlebitis often accompanies varicose veins. It appears after unsuccessful injections or the influence of pathogenic microorganisms.
Treatment methods for phlebitis of the veins on the arm
During the treatment of phlebitis of the vein in the arm, conservative methods are used:
- Use of non-steroidal anti-inflammatory drugs;
- Antibacterial medications;
- Use of anticoagulants;
- Local measures - elastic bandage to restore blood flow.
If an infection is added to simple inflammation, then treatment consists of complex effects:
- Relief of the inflammatory focus;
- Prevention of spasms and hypertonicity of the walls;
- Increased venous blood flow;
- Qualitative improvement of blood viscosity;
- Fighting the formation of blood clots;
- Stabilization of the tone of the smooth muscles of the veins;
- Getting rid of puffiness and normalizing lymph circulation.
If an infection appears, then after determining the type of pathogen, specialized treatment measures are prescribed. Heparin and troxevasin ointments are used in the form of local preparations.
During the treatment of post-injection phlebitis of the veins in the arm, non-steroidal anti-inflammatory drugs are used, both orally and with the help of ointments.
Self-medication of phlebitis is fraught with complications for the patient, but poses a direct threat to his life.
If a focus of inflammation occurs on the arm after an injection or due to other reasons, it is necessary to seek specialized help for comprehensive treatment.
Causes of phlebitis
Phlebitis can be superficial or internal. The first form is not dangerous, but the second leads to the formation of blood clots in the vessels, which is fraught with consequences.
Phlebitis most often affects the vessels of the legs, there are cases of its appearance on the arms, the inflammatory process affects different parts of the walls , they are distinguished:
- Periphlebitis is mostly inflammation of the tissue around the lesion in combination with phlebitis and thrombosis.
- Endophlebitis is inflammation of the inner surface of a vessel, a consequence of infection or injury to the wall.
- Panphlebitis - damage to all parts of the vein.
More often on the hands there is endophlebitis - a lesion after a catheter, the needle even slightly irritates the walls of the vessel, the nerve endings contained in it. As a result, a spasm occurs, reducing the outflow of blood, promoting its thickening.
In the same way, substances introduced into a vessel can affect its walls and worsen the quality of blood. Post-injection phlebitis is complicated by thrombophlebitis, which is manifested by the formation of clots.
Phlebitis of the hand may result from infection. During or after a puncture, an infection enters the injection site, which leads to inflammation. If this process is not stopped, an abscess or phlegmon develops, which requires surgical intervention.
The cause of phlebitis on the arm will not be injections and IVs, but a long-lasting bruise, but this is rare.
Inflammation of superficial veins
There is another method for classifying phlebitis, which affects superficial vessels:
- Allergic phlebitis - exposure to allergens, sluggish without bright bursts.
- Infectious – a consequence of the influence of infections.
- Painful – often occurs in women after childbirth.
- Migratory is a chronic form, the foci of which can appear in different places of the body.
Each type of phlebitis of the superficial veins occurs as a result of a specific preceding cause, for example:
- Phlebeurysm;
- Diseases in which the walls of blood vessels are stretched, which is a favorable environment for the manifestation of phlebitis;
- Many injections, frequent use of a catheter;
- Violation of norms for the use of medical procedures;
- The presence of a focus of infection - purulent formations, boils, inflammation of internal organs.
- Injuries, heavy physical labor;
- Sedentary, sedentary lifestyle;
- Pregnancy and the ensuing consequences;
- Artificially provoked - during sclerotherapy, inflammation of the superficial wall of the vein is specially provoked.
Post-injection form of pathology
Post-injection phlebitis of the hands occurs as a result of the use of catheters that injure the walls of the veins.
Many factors influence the degree and nature of injury:
- The material from which the instrument is made;
- Length, needle diameter;
- Time of continuous use;
- Volume, speed and concentration of the infused substance;
- Compliance with hygiene standards.
The reason will be the increased concentration of components injected using a dropper; it plays the role of an irritant.
//feedmed.ru/bolezni/serdechno-sosudistye/flebit-ruke.html
For example:
- Doxycycline hydrochloride solution;
- Calcium chloride;
- Potassium;
- Glucose.medicines.
The use of drugs causes a spasm that affects nerve tissue, the lumen of the vein narrows, and inflammation develops. If an infection is added to everything, phlebitis worsens, then urgent therapy will be required.
Often phlebitis after injections occurs due to the use of IVs outside the hospital walls, when:
- They get out of binge drinking on their own at home.
- When performing active detoxification processes.
- IV injections for suicide attempts.
- Use of aggressive components by drug addicts.
During these moments, endophlebitis occurs, which leads to inflammation of the lining inside the vein, then a progressive process appears and severe consequences occur.
In determining the diagnosis, they rely on clinical signs and histological studies, using them to determine the degree of replacement of smooth muscle cells with fibrous formations, which characterizes chronic phlebitis based on post-injection.
Symptoms and manifestation of the problem
The first signs of phlebitis are redness at the site of the catheter, redness, and swelling of the skin.
Often all these symptoms go away quickly after the catheter is removed.
But when the process worsens:
- The skin is hyperemic, which actively spreads along the injured artery.
- Severe swelling appears.
- The temperature rises extremely.
- During the examination, inflammation and infiltration of the subcutaneous tissue and soft tissues are noticeable.
- There is a noticeable increase in regional lymph nodes - axillary, elbow.
- The vein will become like a thick cord, akin to connective tissue.
The patient's condition worsens extremely due to elevated temperature, inflammation at the injection site, and after 2-3 days the lower third of the forearm and hand are affected. If treatment is not started immediately, the adjacent vessel will succumb to damage.
At this stage, deviations in the correctness of the established diagnosis are allowed, phlebitis is similar to phlegmon, the reason for this is blockage of the central venous trunk, resulting in a reflex spasm of the adjacent artery, which is perceived as arterial obstruction.
Diet for phlebitis of the upper extremities
Phlebitis is a disease that affects the veins and is accompanied by their inflammation. The root cause of the formation of this condition in the body is in most cases considered to be varicose veins; the causes may include infectious agents, excess body weight, and an unbalanced diet.
Since with phlebitis the venous wall suffers, to which unnecessary substances stick over and over again, the diet should be based on healthy foods, you should avoid eating foods:
- Fatty, canned, smoked foods;
- Fast food;
- Carbonated drinks, spirits;
- Animal fat;
- Lots of flour, confectionery, chocolate, chips, snacks;
- Margarine and butter.
For phlebitis of the upper extremities, you need to drink a daily dose of clean water. The range of foods consumed should be expanded; the main complication of phlebitis is clogging of the lumen of the veins, the formation of thrombotic masses, this occurs due to an increase in the density of the blood fluid.
There is a list of products that can cope with the problem of the formation of thrombotic masses:
- Lemon, which contains vitamin C and potassium, thanks to these elements, reduces blood density. You can take the zest or the pulp, and all together. It is not forbidden to use lemon with tea, water, pureed with sugar or honey.
- Ginger root, which is best used in the form of ginger tea, but you should not drink more than a liter of such tea per day; there are contraindications if a person suffers from kidney, liver, or heart diseases.
- Cranberries are used in their original form and in dried form. You can eat ripe fruits and make teas, decoctions, and juices based on them. Do not eat berries if you have gastritis or ulcers.
- Garlic prevents blood clotting; you can eat it in its pure form or as a food additive. Contraindications exist in the case of gastritis, stomach ulcers, hemorrhoids, and heart disease.
Due to the fact that an excess of the presented products can provoke the appearance of unwanted side effects, the intake and course of treatment, the need to use the product will be determined by the attending doctor.
Traditional methods for getting rid of phlebitis on the arm
There are several productive methods of traditional medicine that help solve the problem of inflammatory processes in the walls of the veins; recipes are usually used for this:
- Several horse chestnut fruits should be cut into smaller pieces, dried, and crushed in a mortar or coffee grinder to a powdery consistency. Additionally, the chestnut tree bark should be dried and crushed in the same way. Then you need to take a tablespoon of the resulting horse chestnut powder, a spoonful of the bark, pour two hundred milliliters of red wine (dry), then the infusion sits for 3 days. After 3 days, five hundred milliliters of olive oil is added to it, the mixture is heated over a fire until the wine evaporates, the remaining mass is applied to the affected areas as a compress.
- Dried tops (fifty grams) or fresh tops (100 grams) are doused with a liter of boiling water and left to settle for an hour. The resulting decoction should be consumed half a cup after meals three times a day.
- A tablespoon of dried and crushed hazel leaves is poured with five hundred milliliters of water and sent to a boil over medium heat. After boiling, you need to slightly reduce the gas and leave to simmer for another five minutes. After removing from the stove, you should leave the broth for about five minutes. Drink half a cup of infusion four times a day before meals.
- Crush the dried wormwood leaves and mix a tablespoon with a small amount of kefir until a mixture has the consistency of sour cream. Spread it on thick gauze, apply to the affected area, and leave overnight. Should be done for 4 days with a week break. Fern leaves can be used this way.
- Leaves of currant, bearberry, lingonberry, dried rowan fruits should be brewed like ordinary tea, drink half a mug in the mornings and evenings.
It is important to note that traditional methods act as additional preventive measures, but will never replace complete drug treatment, especially when it comes to the acute course of the disease. Such treatment can be carried out with the permission of the doctor; after making an accurate diagnosis, the blood can be greatly diluted, which is not a good indicator.
Outcome and complications of phlebitis
The central terrible complication of phlebitis is thrombophlebitis. It occurs as a result of an increase in the thickness of the blood, which makes it difficult for it to move through the veins that are subject to destructive effects.
The accumulation of blood clots on the venous wall may be triggered, or a thrombus or embolus may form. The most terrible consequence of these modifications will be the detachment of a blood clot or embolus from the wall and circulation through the blood. As a result, it is introduced into some organs, which leads to a disastrous outcome.
Thrombophlebitis, which has passed into the stage of acute development, can be dangerous due to the manifestation of thromboembolism of the pulmonary artery, that is, clogging of the lung vessels with a detached blood clot, which disrupts the breathing process.
The companions of phlebitis will be abscesses and phlegmon. But various unfavorable outcomes and complications of phlebitis are observed when treatment is not started on time.
If you consult a specialist in a timely manner, inflammatory processes in the veins are easily eliminated and do not cause undesirable consequences.
The main thing is to identify the cause of the lesion, and then try to lead a healthy lifestyle and be guided by the principles of proper nutrition.
Preventive measures against the formation of phlebitis
To avoid or avoid recurrence of this disease, the fundamental condition is to maintain a correct lifestyle.
As a result, there are several central methods for preventing inflammation of the veins:
- An appropriate diet is the exclusion of fatty, high-calorie, junk and fried foods;
- Walking does not need to be long, it is enough that they are carried out regularly;
- Exercise;
- Refusal of bad habits, taboos on drinking alcohol;
- The correct daily routine, you can’t overwork yourself, you need to rest and sleep on time.
In persons with varicose veins, additional treatment with gels and medicinal ointments is necessary. In the occurrence of phlebitis, purulent processes and infectious diseases play a certain role, then if they are detected, their treatment should be started immediately.
Doctor: Olga Shishkina ✓ Article checked by doctor
Source: //FeedMed.ru/bolezni/serdechno-sosudistye/flebit-ruke.html
Possible complications
Often, complications of post-injection thrombophlebitis are caused by the lack of adequate therapy or self-medication. In the latter case, there is a risk not only of causing great harm to health, but also of death.
If acute phlebitis is treated adequately, it usually does not pose a health hazard. In this case, there is a chronic form of the disease that has unexpressed symptoms.
In such a situation, a person simply ignores the manifestations or uses folk remedies. A sudden exacerbation of the disease can provoke serious consequences.
Therapy methods
In most cases, conservative treatment is used for the treatment of phlebitis after IV injections, which includes:
- therapy with non-steroidal anti-inflammatory drugs - nimesulide, ibuprofen;
- antibacterial therapy (endolymphatic administration);
- use of anticoagulants;
- local treatment - bandages with silver preparations.
In cases where there is mild damage to the superficial veins caused by IV injections, only conservative treatment is required, aimed at relieving inflammation and relieving pain. If there is a more extensive process with the addition of a bacterial infection, then therapy should be comprehensive, aimed at:
- relief of the inflammatory process;
- fight against spasm and hypertonicity of the vessel walls;
- increased venous blood flow;
- decreased blood viscosity;
- fight against blood clots;
- stabilization of the tone of the smooth muscles of the veins;
- Relieving swelling and improving lymph circulation.
Non-steroidal anti-inflammatory drugs, both orally and in the form of ointments, are used to treat inflammation. Preference is given to new generation NSAIDs, but along with them, butadione, nimesulide and others are successfully used. When an infection occurs, the type of pathogen is determined and specialized antibacterial therapy for phlebitis is prescribed. Drugs can be administered endolymphatically in order to increase their concentration at the site of infection .
Ointments containing heparin and troxevasin are applied to the site of inflammation, reducing inflammation and improving venous patency. Trental and other modern medications are used to prevent blood clots.
Treatment of phlebitis caused by IV injections and infusions is carried out in a hospital setting, due to the risk of life-threatening complications such as thromboembolism or the development of phlegmon.
Self-medication of phlebitis that occurs at the site of intravenous injections can pose a direct threat not only to the health, but also to the life of the patient, so you need to seek medical help in a timely manner. Those who have suffered from this disease or are at risk of developing it (with frequent intravenous infusions) need to adjust their lifestyle, combining rest with walking, quit smoking, and eliminate from their lives all factors that cause vasospasm.
Preventive actions
To prevent the occurrence of thrombophlebitis, you need to prevent this disease. First of all, it is recommended to exclude the use of hormonal contraceptives. This is especially true for people who are prone to vascular diseases.
To prevent the development of thrombophlebitis, special physical exercises should be performed. In this case, walking and squats are very useful. Gymnastics classes are no less effective.
If a person receives long-term treatment using injections or droppers, these areas need to be systematically treated with special ointments. If you suspect the development of phlebitis, you should consult a doctor. A blood clot located in a vessel can break off, leading to instant death.
Post-injection thrombophlebitis is a fairly serious disorder that is accompanied by unpleasant symptoms and can pose a real threat to life.
To prevent the development of dangerous complications or death, you should promptly consult a qualified doctor. Only adequate and timely therapy will help to quickly cope with the pathology and prevent negative consequences.
Source: serdce.hvatit-bolet.ru
Preventive measures
Not a single patient is immune from the post-injection form of phlebitis. Therefore, every person must take responsibility for their health and lead a healthy lifestyle.
What to do to avoid the formation of phlebitis. To prevent vascular inflammation, doctors recommend the following measures:
- regular walks in the fresh air at any time of the year;
- rejection of bad habits;
- daily physical activity (jogging, gymnastic elements, aerobic and cardio exercise);
- adherence to the principles of proper nutrition;
- exclusion from the diet of fatty, salty, spicy foods;
- adherence to a daily routine (full rest and sleep are required).
If you are undergoing treatment using intravenous injections and droppers, lubricate the needle insertion site with venotonics (Venoruton, Troxevasin, etc.) to prevent inflammation of the vascular walls.
Remember that phlebitis does not forgive a frivolous attitude. Therefore, if you suspect venous inflammation, immediately seek help from specialists. Timely measures taken to eliminate phlebitis guarantee complete recovery.
A venous catheter is a medical device intended for regular, long-term intravenous administration of drugs to a patient. After its installation, there is no need to constantly puncture the vessel for drip or jet delivery of medication, which is considered the main advantage of the catheter. If the rules of asepsis are not observed or incorrect concentrations of the drug are used, phlebitis of the vein in the arm develops, the treatment of which cannot be postponed until later.