Classifications of heart attacks
There are three types of heart attacks. Below are their characteristics. In addition, the table shows the organs in which necrotic processes begin against the background of impaired blood circulation.
| Type of heart attack | a brief description of | The organ that is affected |
| Ischemic (white) | Stopping the movement of blood in the vessels. Dry necrosis appears. Tissues and cells are not supplied with nutrients. | Brain, kidneys, spleen, heart. |
| Hemorrhagic (red) | Occurs due to congestion in the veins. The necrosis zone is saturated with blood, its excess causes cell damage, which is why this type of infarction is called “red”. | Lungs, intestines, brain, spleen. |
| Anemic or ischemic with hemorrhagic belt | It combines two types of lesions - dry necrosis with hemorrhage. The affected area is light with a red rim. | Heart, kidneys, spleen. |
Note: If two main human organs are affected - the brain and heart, the probability of death is up to 90%.
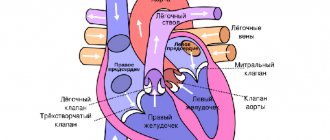
In the classification of myocardial infarction, the following types are distinguished:
- painful;
- painless;
- abdominal;
- cerebral;
- combined;
- atypical.
Depending on the depth of damage to the heart muscle, a heart attack occurs:
- subendocardial (in the deep layers of the myocardium);
- subepicardial (in the outer layers);
- intramural (in the thickness of the muscular walls of the myocardium);
- transmural infarction (on the anterior wall of the heart).
Depending on the affected area, focal or extensive infarctions are distinguished. Focal infarction leads to shallow necrosis and affects minor areas. Areas of necrosis subsequently become scarred. With timely assistance provided, there is no serious threat to the patient’s life.
With an extensive infarction, the zone of necrosis extends to all layers of the heart muscle and affects large areas. The condition is complicated by cardiac ruptures, painful shock, thromboembolism, symptoms of “acute abdomen,” and pericarditis. Most of the heart cells die and are no longer restored. This leads to the patient's postmortem diagnosis of “death from a heart attack” in 80% of cases.
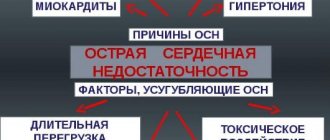
Factors of occurrence
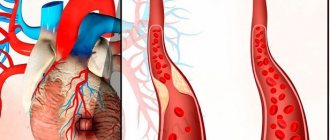
The main cause of a heart attack is a disruption in the functioning of the circulatory system. This can be influenced by several factors, which include:
- Abrupt cessation of arterial blood flow through a coronary vessel (when the lumen of the vessel closes).
- A discrepancy between the need of the myocardium (the middle muscular layer of the heart) for oxygen and the ability of the coronary vessels to provide this necessary need. Under normal conditions, the myocardium takes 70-75% of the oxygen contained in the blood from the blood. For comparison: muscle oxygen demand is about 25-30%. That is why the heart depends so much on the ability of the coronary arteries to adequately respond to changes in workloads in the myocardium itself.
- Arterial hypertension – when high blood pressure causes the heart to work faster, which means the wear and tear on the muscles and blood vessels increases significantly.
- Thrombophlebitis.
- Stagnation and accumulation of fluids of various etiologies between the membranes of the heart muscle.
- Heart damage due to injury or poisoning.
If it is not possible to quickly restore blood circulation, then there will be a threat to life, and everything may end in the death of the patient.
Reasons that worsen the functioning of the heart and circulatory system:
- pathology of lipid metabolism, when the amount of fat, cholesterol and triglycerides in the blood increases. This helps to reduce the lumens of blood vessels, which leads to poor circulation.
- decreased motor activity. In patients who are bedridden, death from a heart attack occurs more often.
- the patient is overweight.
- diseases of the endocrine system (diabetes mellitus).
- presence of bad habits (alcoholism, smoking).
- hypertension.
- burdened heredity.
- history of prolonged or short-term loss of consciousness.
- previous operations on the heart muscle.
- heart failure.
- increased tone of the nervous system.
- high heart rate (90 beats per minute), etc.
Symptoms
With an impending myocardial infarction, the following picture can be observed:
- there is severe sudden pain in the chest or behind the breastbone, which radiates (radiates) to the arms, back, stomach, neck, shoulders or even jaw;
- the patient does not have enough air, he begins to inhale forcefully;
- dizziness appears, cold sweat appears, the skin turns pale;
- a feeling of extreme fatigue increases;
- Nervousness, feelings of anxiety, and causeless panic increase.
Having noticed that a person is in a similar condition, it is necessary to urgently call a team of doctors. When talking to the dispatcher, it is necessary to inform that the patient is suspected of having a heart attack. A fully equipped ambulance with a cardiograph and appropriate medications will be sent to such a call.
Often myocardial infarction has no permanent symptoms. This is explained by different zones of localization of necrosis and, depending on this, different intensity of the resulting pain symptom. This state of affairs makes diagnosis difficult. Often the patient and his surroundings do not have time to adequately respond to a heart attack: the absence of heart rhythms occurs very quickly. Sudden cardiac arrest can occur in the complete absence of any symptoms. The absence of characteristic signs makes it difficult to urgently hospitalize the patient. That is why, with a massive heart attack, people die suddenly at home, and often there is no person nearby who can recognize the pathological process and provide first aid.
They don’t call an ambulance or see a doctor
Unfortunately, with the symptoms of a myocardial infarction—pain behind the sternum, difficulty breathing, cold sweat—patients are in no hurry to call an ambulance, waiting for the pain to “dissolve on its own.” Very often, heaviness behind the sternum is attributed to poisoning, osteochondrosis, or change in weather. As a result, 40-50% of heart attack survivors die at home without seeking medical help.
“For any symptoms that suggest the development of acute coronary syndrome, it is important to immediately call an ambulance in order to begin providing first aid to the patient as soon as possible,” says Simon Teimurazovich Matskeplishvili, Doctor of Medical Sciences, Corresponding Member of the Russian Academy of Sciences, Professor, Deputy Director for scientific work of the medical research and educational center of Moscow State University. Lomonosov. “With timely delivery of the patient to the hospital, most of the life-threatening consequences of this condition can be prevented.”
Acute coronary syndrome (ACS) is an exacerbation of coronary heart disease (CHD), which combines conditions such as unstable angina and acute myocardial infarction.
Help with sudden cardiac arrest
However, upon discovering that a person has suffered cardiac arrest, you must immediately call an ambulance, informing the operator that the person has suffered cardiac arrest. It is advisable to independently perform chest compressions and carry out artificial ventilation using the mouth-to-mouth breathing technique. This will allow the body to hold out until the doctors arrive.
In the clinic, in the intensive care unit, measures to bring the patient back to life will include defibrillation of the heart using electric current pulses, intubation of the lungs, and administration of special medications that nourish the heart muscle. If everything is done correctly, and most importantly, quickly, the patient will have a chance to survive.
Important! In women, the symptoms of a heart attack may be vague. It can be confused with the flu or severe fatigue. Pay attention to the heart rhythm and provide immediate assistance, since death from a heart attack occurs very quickly.
Interpretation of death
Death is a natural process of ending our existence. Without it, it is impossible to imagine the evolution of life on earth. What happens when a person dies? This question has interested and will continue to interest humanity as long as it exists.
Passing away proves to some extent that it is survival of the fittest and the fittest. Without it, biological progress would have been impossible, and man might never have appeared.
Despite the fact that this natural process has always interested people, talking about death is difficult and difficult. First of all, because a psychological problem arises. Talking about it, we seem to be mentally approaching the end of our life, which is why we don’t want to talk about death in any context.
On the other hand, it is difficult to talk about death, because we, the living, have not experienced it, so we cannot say what a person feels when he dies.
Some compare death to simply falling asleep, while others argue that it is a kind of forgetting, when a person completely forgets about everything. But neither one nor the other, of course, is right. These analogies cannot be called adequate. We can only say that death is the disappearance of our consciousness.
Many continue to believe that after his death a person simply passes into another world, where he exists not at the level of the physical body, but at the level of the soul.
It's safe to say that research into death will always continue, but it will never provide a definitive answer about how people feel at this moment. This is simply impossible; no one has ever returned from the other world to tell us how and what is happening there.
What does death from a heart attack look like?
Any cause of death due to myocardial infarction is associated with a malfunction of the circulatory system. A pathological process in the heart muscle leads to irreversible processes, fatal sensations and, as a rule, death.
Processes in the body
Violation of the blood supply to the heart muscle of any etiology, which is the cause of death from a heart attack, is manifested by the following symptoms:
| Cause | Consequence |
| Violation of the rhythm and sequence of the stage of excitation and contraction of the heart muscle | Blood is pumped in insufficient volume, and coronary shock occurs (a sharp decrease in the ability of the myocardium to contract). In this case, clinical death occurs. |
| Stopping venous blood flow | Pulmonary edema occurs and death occurs due to a heart attack. |
| Inconsistency of the heart ventricles | Disorganized series of impulses arise in the ventricles of the heart, their source is in the lower chambers of the heart. Blood pumping stops, which causes death in myocardial infarction. |
| Rupture of the walls of the heart | The heart fills with blood, a rupture occurs and the heartbeat stops immediately. |
External signs of death from a heart attack
By some signs you can understand that a person is no longer a tenant.
They show what death that occurs from a heart attack looks like. In these cases, the following symptoms of impending death are noted:
- tachycardia or bradycardia;
- decrease in blood pressure: pulse becomes very rare;
- the skin acquires a bluish tint, the lips turn blue especially quickly;
- fluid stagnation and swelling occur in the lungs;
- loss of consciousness;
- convulsions;
- dilated pupils - reaction to light is almost completely lost;
- breathing is initially noisy and frequent, then becomes rarer, until it stops completely (apnea is recorded).
- absence of a curve on the electrocardiogram.
Important! Irreversible processes in the body develop 3-5 minutes after clinical death is declared. Only about 3-4% of patients emerge from clinical death without consequences. Other patients do not restore all body functions after resuscitation.
External signs of death from a heart attack are not reflected in any way on the dead body of the patient. Rigor mortis and discoloration of the skin occur at the same time as in patients who die for other reasons.
Incidence of myocardial infarction in Russia
According to P.E. Lukomsky and E.M.
Tareev - cardiologists of the First Moscow State Medical University named after. Sechenov, aged 50-59 years account for 41.2% of heart attack cases. In a Moscow study of men under 60 years of age under the leadership of V. I. Metelitsa - head. Department of Therapy TsOLIUV, mortality from myocardial infarction in the early 90s was 550 people per 100 thousand population.
According to the Russian Scientific Cardiology Center - RNCC, mortality from acute myocardial infarction ranges from 18.5% to 50%. Moreover, among patients over 60 years of age, mortality averages 32.5%.
Some domestic cardiologists argue that mortality from myocardial infarction (MI) has been increasing recently. According to the Orenburg State Medical University, 445 people out of 1 million died from myocardial infarction in Russia in 2020. Despite the fact that in 2012 this figure was at around 385 people out of 1 million.
The statistics from the Russian Scientific Cardiology Center are also sad, showing an increase in mortality from heart attacks among young people. According to their data, mortality from MI in young people aged 20 to 24 years from 2002 to 2020 in the Russian Federation increased by 82%. By the way, among 30-35 year olds, mortality from MI over the same period increased by 63%. The statistics are described in the scientific work “Processing statistical data of myocardial infarction” by cardiologist E.V. Ponomareva.
Other scientists say that the mortality rate from MI is gradually decreasing. Cardiologists from the National Medical Research Center for Preventive Medicine in Moscow and Kemerovo State Medical University note a decrease in mortality from myocardial infarction. Their studies from 2006 to 2020 revealed that mortality from acute MI decreased by 14.3%, and from repeated MI by 12.8%.
A decrease in mortality in men was observed at all ages. For women, the exception was the age groups 20-29 and 80-89 years old - in these groups, on the contrary, mortality increased. In men aged 20-29 years and 80-89 years, the number of heart attacks decreased by 47% and 6.6%, respectively. At the same time, in women 20-29 years old, mortality from myocardial infarction during the study period increased by 32.28%. The scientific work was prepared by cardiologists Samorodskaya I.V., Barbalash O.L., Starinskaya M.A. The work was published in the Russian Journal of Cardiology No. 11 (151).
According to the Ministry of Health, from 2010 to 2020, mortality from myocardial infarction decreased by 14%. At the end of 2020, this figure was 858 thousand people. This is 5% less than in 2020. Reported on the Rosstat website.
According to Professor L.A. Alekseeva, Ph.D. Dorofeeva E.V. and Professor Makhovskaya T.G. from the “Polyclinic for the Administration of the President of the Russian Federation,” the incidence of myocardial infarction decreased from 0.95% in 2000 to 0.26% in 2014. This decrease led to a decrease in mortality from myocardial infarction. Over the same period, mortality from MI decreased from 0.19 to 0.06%.
The same doctors studied the incidence of heart attack in patients under 70 and after 70 years. Between 2000 and 2014, it decreased from 0.38 to 0.08% in subjects under 70 years of age. In people over 70 years of age, this figure also decreased, but remained relatively high. Thus, from 2.4% in 2000, the figure decreased only to 1.3% in 2014.
Statistics were also collected in the capital itself. Information collected by the organizational and methodological department of the Moscow Department of Health shows that the creation of a heart attack network in the city has reduced the number of deaths from myocardial infarction. From 2012 to 2014, the number of deaths from MI in Moscow decreased by 36.4%. This was reported in the journal “Analytical Bulletin” No. 44, dedicated to the problem of cardiovascular diseases.
Analysis of the incidence of myocardial infarction, carried out by cardiologists Bunova S.S., Usacheva E.V. and Zamakhina O.V., revealed a decrease in the incidence of heart attacks. From 2002 to 2012 the incidence of MI decreased by 10.8%. At the same time, the recurrent incidence of myocardial infarction over the same period increased by 14.9%.
On top of this, there are mixed data regarding cardiac pathologies. Scientists from the Russian Cardiology Research and Production Complex (RCNPC) have collected their statistics on myocardial infarction. A group of doctors led by Oshchepkova E.V., Efremova Yu.E. and Karpov Yu.A. found that mortality from myocardial infarction in the Russian Federation from 2000 to 2011 increased by only 3.8%. At the same time, the number of deaths from primary MI decreased by 5.3%. However, mortality from recurrent heart attack increased by 33.7%.
Cardiologist Chazova I.E. from the Ministry of Health of Russia together with Professor Oshchepkova E.V. from the Department of Cardiovascular Disease Registries state that the cause of a heart attack is most often hypertension. Information about this is also presented in the journal “Analytical Bulletin - On current issues in the fight against cardiovascular diseases” for 2020.
Specialists from the Saratov Research Institute of Cardiology studied the relationship between repeated myocardial infarction and the time of day. Scientific work with the participation of doctors Rakovsky M.E., Rybak O.K., Sorokina E.N., Morozov I.A. found that the maximum risk of MI of 28.3% occurs from 1:00 to 5:00. The minimum probability of a heart attack - 6.7% - is observed in the daytime from 12 to 17 hours. High-risk hours are considered to be from 8 a.m. to 12 a.m. The results of the scientific work were published in the Russian Journal of Cardiology No. 1 for 2003.
RKNPK specialists also noted that the mortality rate from MI in a hospital setting is 60%. Moreover, 40.4% of them die from complications of a heart attack in the next 24 hours after arriving at the hospital. The data are presented in the scientific work “Morbidity and Mortality from Myocardial Infarction in the Russian Federation”, published in the journal “Therapeutic Archive” No. 4 (85) in 2013.
Scientists from the same cardiology center provide data on the number of heart attacks in the federal districts of Russia. According to RKNPK cardiologists, the leader in the number of MIs is the Ural Federal District - 81,500 cases annually. The Volga Federal District is in second place with 63,800 cases of MI per year. The position below is the Siberian Federal District - 38,300 cases annually. More details are described in the table below.
| Federal District | Number of cases of myocardial infarction (thousand people per year) |
| Ural | 81,5 |
| Privolzhsky | 63,8 |
| Siberian | 38,3 |
| Southern | 33,1 |
| Northwestern | 30,5 |
| North Caucasian | 22,1 |
| Crimean | 10,0 |
| Far Eastern | 9,6 |
| Central | No data |
The scientific work of Dr. Kulaeva A.S., published on the website of the Youth Scientific Forum, presents a survey among people who have suffered a myocardial infarction. The purpose of the survey was to identify factors influencing the risk of developing MI. The factors themselves and the likelihood of their influence on the occurrence of a heart attack are shown in the table.
| Risk factor | Probability of developing myocardial infarction |
| Age 30-40 years | 8% |
| Age 40-50 years | 18% |
| Age 50-60 years | 30% |
| Age over 60 years | 44% |
| Hypertonic disease | 54% |
| Excess weight | 64% |
| Abundance of fatty foods in the diet | 56% |
| Increased levels of “bad” cholesterol | 58% |
| Weekly alcohol consumption | 24% |
| Smoking | 34% |
| Heredity | 42% |
Thus, looking at the table, you can calculate the risk of a heart attack in the presence of the factors described above.
The same scientific work indicates the relative number of deaths and survivors after MI who took medications in advance. Information about this is presented in the table.
| Group of drugs | MI survivors | Died as a result of myocardial infarction |
| Diuretics | 14,0% | 10,5% |
| Beta blockers | 23,9% | 16,8% |
| ACEI | 36,9% | 30,4% |
| Antiplatelet agents | 16,2% | 13,6% |
| Statins | 2,2% | 1,1% |
| Calcium antagonists | 8,2% | 5,8% |
Specialists from the National Medical Research Center for Preventive Medicine of the Russian Ministry of Health analyzed the incidence of myocardial infarction in all federal districts of the Russian Federation. It was found that the minimum incidence of acute and recurrent MI was observed in the Southern Federal District - 0.12 and 0.017% of the district's population, respectively. Despite the fact that the maximum incidence of heart attack was recorded in the Volga Federal District - 0.15% of the population. By 2012, the Volga Federal District became the first in the number of repeated cases of heart attack. This year in the district, the number of patients with a second heart attack reached 0.032% of the total population. The opposite picture was observed in the Far Eastern Federal District. In 2012, the incidence of acute and recurrent myocardial infarction was 0.11% and 0.02%, respectively. Morbidity statistics by district were published in the journal “Social Aspects of Population Health” (2014, No. 6).
In 2012, a Rosstat study was published in the Russian Journal of Cardiology No. 97, which provided information on excess mortality in men. Medical analysts have calculated that mortality from myocardial infarction in the stronger sex is 9.1 times more common than in women.
According to the results of the MONICA program conducted by WHO in Russia in 1997, the risk of death from acute myocardial infarction within 28 days after its occurrence was 49% in men and 51% in women. Moreover, this indicator was valid for 29 populations aged 35 to 64 years. The same study showed that 33% of cases of acute myocardial infarction are fatal within an hour after the development of the first symptoms. The results of the MONICA program are presented in the 19th issue of the journal Preventive Medicine for 2016.
Research by the Federal State Budgetary Institution Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev" led by cardiologist L.A. Bokeria. and Academician of the Russian Academy of Sciences Gudkova R.G. found that 19.4% of the adult population of Russia have an increased risk of myocardial infarction. Interestingly, this scientific work also analyzed the likelihood of MI in children under 17 years of age. According to scientists, about 1% of children in Russia are at risk of having a heart attack at such an early age. In addition, these same experts claim that the risk of having a myocardial infarction between the ages of 45 and 60 is 30.5%. Data are presented for 2014 in the 44th issue of the journal “Analytical Bulletin - On current issues in the fight against cardiovascular diseases.”
Who is at risk of a heart attack
We can distinguish groups of patients whose risk of death from myocardial infarction is very high:
- resuscitated after cardiac arrest, clinical death;
- people with acute heart failure (the contraction function of the heart muscle is not fully restored);
- persons with a history of myocardial ischemia (reduced blood flow to certain areas of the heart);
- patients with pronounced hypertrophy (thickening) of the left ventricle, which is visible during examination;
- patients with congenital or fatal diseases or those with irreversible anatomical changes in the heart (valve prolapse, athlete's heart, congenital anomalies in the coronary vessels, sarcoidosis);
- patients with any neoplasms of the myocardium;
- suffering from apnea (stopping breathing) during sleep.
Types of disease
A heart attack often means a pathological focus in the main muscle of our heart - the myocardium. In fact, it can develop in any organ - kidneys, spleen, lungs, brain, intestines. It is customary to distinguish three types of this condition.
- Ischemic. It develops with severe ischemia as a result of disruption of the flow of normal blood volume. It is noted in the GM, heart, and spleen.
- Hemorrhagic. Occurs due to congestion in the veins, resulting in hemorrhage into the tissue. Develops in the lungs, intestines, and spleen.
- Ischemic with hemorrhagic belt. It combines the symptoms of both diseases and develops in any organ.
Any ischemia poses a dangerous threat to human life and health. You need to understand that even short-term hypoxia of the myocardium or GM can have unpleasant long-term effects.
When you don't die from a heart attack
A favorable prognosis is given to patients with minor, localized myocardial damage, when only part of the organ is susceptible to necrosis. In this case, the cells that remain unharmed take over the functions of the entire organ, and the person, having undergone the necessary therapy and rehabilitation measures, continues to live. However, it is extremely important to follow all the recommendations of your doctor.
Medicine does not stand still: scientists are working to create drugs and techniques that will reduce mortality from heart attacks. Until this happens, a person must take care of his health to avoid a heart attack.
Mortality statistics
About 30-35% of those admitted to the hospital with this pathology die. It is important to know that among sudden deaths, death from heart attack is up to 20%. According to statistics, in the United States alone, 140 people die every day from this pathology.
Research shows that a heart attack can lead to death in 48% of the fairer sex and 52% of the stronger sex.
What is myocardial infarction
There are studies showing that if not hospitalized, the chance of death is fifteen to twenty percent, while if hospitalized, another 15% die. The greatest probability of death of the patient is in the first 48 hours - that is why it is necessary to have time to carry out professional manipulations in this period of time. Experiments prove that if perfusion is restored within the first six hours from the onset of pathology, the size of the scar can be minimized. In this case, there is a high probability of increasing general and local contractility of the left ventricle. Post-infarction complications with timely intervention occur much less frequently. By restoring perfusion in the first hour or two, we can hope for a rapid recovery of patients.
Mortality statistics from myocardial infarction
When calling an ambulance, it is important to insist on the arrival of a cardiac team. It is quite possible that such persistence will save the patient’s life.
What determines life expectancy?
Life expectancy after a heart attack varies widely. Scientists analyzed cases of death and compiled a list of factors that increase the risk of death.
There are several approaches to determine the prognosis. The TIMI system, which determines the risk of death in the next 2 weeks, has gained the most popularity. It is very easy to use and quite accurate. Each risk factor is assigned a certain score. Based on the sum of points, you can determine the probability of death.
Extensive heart attack:
- diabetes mellitus, arterial hypertension, angina attacks – 1 point;
- systolic pressure {amp}lt; 100 mmHg Art. – 3 points;
- heart rate more than 100 beats/min – 2 points;
- heart failure of 2-4 classes according to Killip – 2 points;
- body weight less than 68 kg – 1 point;
- age over 75 years – 3 points;
- age 65-74 years – 2 points.
Risk of death with a major heart attack (based on total points)
| Points | Probability of death, % |
| 0 | 0,8 |
| 1 | 1,6 |
| 2 | 2,2 |
| 3 | 4,4 |
| 4 | 7,3 |
| 5 | 12 |
| 6 | 16 |
| 7 | 23 |
| 8 | 27 |
| 9-14 | 36 |
Predictors of death for microinfarction are:
- age over 65 years – 1 point;
- 3 or more risk factors for the development of atherosclerotic plaques – 1 point;
- established narrowing of the artery lumen by more than 50% – 1 point;
- use of aspirin over the past 7 days – 1 point;
- serious attack of angina in the last 24 hours – 1 point;
- increased level of markers of cardiac muscle necrosis – 1 point;
- ST wave deviation more than 0.5 mm – 1 point.
Risk of death in small-focal infarction (according to the sum of points)
| Points | Probability of death, % |
| 0-1 | 3-5 |
| 2 | 3-8 |
| 3 | 5-13 |
| 4 | 7-20 |
| 5 | 12-26 |
| 6-7 | 19-41 |
Long-term assessment of life expectancy takes into account:
- timeliness and completeness of medical care during a heart attack;
- level of physical activity;
- person's weight;
- presence of bad habits, especially smoking;
- condition of the valves, chambers of the heart, especially the left ventricle;
- quality of blood pressure control.
The most favorable prognosis is associated with:
- early restoration of normal blood circulation using percutaneous coronary intervention or through the use of thrombolytics;
- preserved left ventricular function;
- timely use of aspirin, beta blockers, ACE inhibitors.
How to influence the forecast?
How many years a person lives after a heart attack largely depends on the person himself. Disciplined adherence to doctor's recommendations significantly increases life expectancy. To live longer, you need to undergo a rehabilitation course and make its principles the basis of your life (3):
- Give up cigarettes. Smoking increases the likelihood of death by 35-43%. since tobacco smoke promotes thrombus formation due to spasm of the vascular wall;
- Physical exercise. Daily physical activity reduces heart attack mortality by 26%. It is useful to alternate different types of exercise: walking, performing physical therapy exercises, working in the garden, around the house;
- Normalize weight. People with a BMI of more than 30 kg/m2 and/or a waist circumference of 88 cm (women), 102 cm (men) are at risk of developing fatal complications.
- Monitor blood pressure (BP). The presence of uncontrolled hypertension significantly increases the chances of developing a recurrent heart attack, as well as other cardiovascular pathologies.
- Prevent the development of influenza. With this viral disease, the likelihood of heart complications is high. People who have had a heart attack are recommended to be protected by vaccination.
- Follow a diet. Minimizing the amount of salt, fried, fatty foods, pickles, marinades, and alcohol increases the chances of a long life.
Psychological assistance does not affect life expectancy, but increases its quality. If socialization is difficult for you, you cannot overcome your fears, you may have developed depression - a common complication after a heart attack. Contact a cardiologist, he will write out an appointment with a psychologist.
Which artist suffered a heart attack?
One of those who once survived a heart attack is the famous Russian film director and TV presenter Tigran Keosayan. The artist felt severely unwell on June 18, 2010. Afterwards he was taken to the Research Institute named after. Bakulev, where he underwent emergency surgery.
It is noteworthy that before this Koesyan suffered a heart attack in 2008. Each time, doctors managed to miraculously save the director.
According to some reports, the famous performer Boris Grebenshchikov also suffered a heart attack. Information about this appeared in blogs after the concert of the leader of the Aquarium group in Samara as part of the Rock over the Volga festival. Then he became ill right during the performance, as a result of which, according to an unofficial version, he was hospitalized.
The terrible pathology did not spare the famous actress Natalya Krachkovskaya. Her health began to rapidly deteriorate in 2015: then she was hospitalized with hydrostatic pulmonary edema.
A year later, on February 28, 2020, Krachkovskaya was admitted to intensive care with acute myocardial infarction. The actress died there a few days later. On March 5, she was buried at the Troekurovsky cemetery.
A heart attack was also named as the cause of death of the famous Russian performer and composer Alexander Barykin, a member of the Gems group. The first alarming “bell” was an acute hypertensive crisis that the singer experienced in the fall of 2010. Afterwards he underwent treatment at the Bryansk Cardiological Dispensary.
Barykin died in March of the following year. According to representatives of the Bryansk production center, with which the singer collaborated, the cause of death was a repeated massive heart attack during the concert. According to official data, the performer barely finished the last song and went backstage, from where he was taken to the hospital by ambulance. There he underwent surgery, and in the morning Barykin died.
According to unconfirmed information, a heart attack killed the famous poet and singer-songwriter Vladimir Vysotsky. It is impossible to accurately determine the cause of his death, since the singer's father refused to conduct an autopsy. However, many argue that he died as a result of an acute heart attack.
Signs of clinical death
If you carefully observe a person, you can quite easily determine the onset of clinical death. She has the following symptoms:
- There is no pulse.
- Breathing stops.
- The heart stops working.
- Severely dilated pupils.
- There are no reflexes.
- The person is unconscious.
- The skin is pale.
- The body is in an unnatural position.
To determine the onset of this moment, you need to feel the pulse and look at the pupils. Clinical death differs from biological death in that the pupils retain the ability to react to light.
The pulse can be felt in the carotid artery. This is usually done simultaneously with checking the pupils to speed up the diagnosis of clinical death.
If a person is not helped during this period, then biological death will occur, and then it will be impossible to bring him back to life.
Stages of death
Death may take different periods of time. This can last minutes, or in some cases hours or days. Dying is a dynamic process, in which death does not occur immediately, but gradually, if you do not mean instant death.
The following stages of dying can be distinguished:
- Preagonal state. The processes of blood circulation and breathing are disrupted, this leads to the fact that the tissues begin to lack oxygen. This condition can last for several hours or several days.
- Terminal pause. Breathing stops, the work of the heart muscle is disrupted, and brain activity stops. This period lasts only a few minutes.
- Agony. The body suddenly begins to fight for survival. At this time, short pauses in breathing and weakening of cardiac activity occur, as a result of which all organ systems cannot function normally. A person’s appearance changes: the eyes become sunken, the nose becomes sharp, the lower jaw begins to sag.
- Clinical death. Breathing and blood circulation stop. During this period, a person can still be revived if no more than 5-6 minutes have passed. It is after returning to life at this stage that many people talk about what happens when a person dies.
- Biological death. The body finally ceases to exist.
After death, many organs remain viable for several hours. This is very important, and it is during this period that they can be used for transplantation into another person.
Signs of death
It is possible to identify initial and reliable signs that indicate that a person has died. The first group includes:
- The body is motionless.
- Pale skin.
- There is no consciousness.
- Breathing stopped, no pulse.
- There is no reaction to external stimuli.
- The pupils do not react to light.
- The body becomes cold.
Signs that indicate 100% death:
- The corpse is numb and cold, and cadaveric spots begin to appear.
- Late cadaveric manifestations: decomposition, mummification.
The first signs can be confused by an ignorant person with loss of consciousness, so only a doctor should pronounce death.
Clinical death
It can be called a transitional stage between the final death of the organism and life. The heart stops working, breathing stops, all signs of the body’s vital functions disappear.
Within 5-6 minutes, irreversible processes have not yet started in the brain, so at this time there is every chance of bringing a person back to life. Adequate resuscitation actions will make the heart beat again and the organs function.
Body temperature and death
Many people are interested in the question of at what temperature a person dies. Most people remember from biology lessons in school that for humans a body temperature above 42 degrees is considered fatal.
Some scientists associate deaths at high temperatures with the properties of water, the molecules of which change their structure. But these are only guesses and assumptions that science has yet to deal with.
If we consider the question of at what temperature a person dies, when hypothermia of the body begins, then we can say that already when the body cools down to 30 degrees, a person loses consciousness. If no measures are taken at this moment, death will occur.
Many such cases happen to people who are intoxicated, who fall asleep right on the street in winter and never wake up.