Granulocytes are a group of white cells that contain granules in their cytoplasm. They are also called granular leukocytes. Granulocytes include neutrophils, basophils and eosinophils. They make up about 60% of all white blood cells. The most numerous group is neutrophil granulocytes, the least in the blood are basophils.
These cells are produced in the bone marrow from precursor cells, which divide within four days, then morphological maturation occurs, which takes five days. As soon as granulocytes enter the bloodstream, they are immediately divided into parietal (temporarily adhering to the walls of blood vessels) and actively circulating. They remain in the blood for about one week, and after release into the tissue they live for about two days.
Granulocytes contain a large number of granules in the cytoplasm, which is why the cells got their name
Types of granulocytes
Granulocytes are divided into neutrophilic, basophilic and eosinophilic depending on how they perceive standard dyes. The size of these cells is 9-12 microns.
Neutrophils are the most numerous group of granular leukocytes. Their name is due to the fact that according to the Romanovsky method they are stained with both a basic dye and an acidic dye (eosin). Mature neutrophil granulocytes are polymorphonuclear cells because their nucleus consists of four to five segments. In the blood of a healthy person, mainly mature segmented forms and a small number of band granulocytes circulate.
Eosinophils get their name due to the fact that they stain only with an acidic dye (eosin) and do not absorb the basic one. Their core consists of two lobes.
Basophilic granulocytes are intensely stained only with basic dye and do not perceive acidic dye, which is why they got their name. These granular leukocytes are characterized by a high content of histamine, prostaglandins, heparin, serotonin and others. Their core is vague, structureless, and usually consists of two segments. It is difficult to see due to the large number of histamine granules in the cytoplasm.
Causes of appearance in the blood
In a healthy person, there should be no myelocytes or other immature cells of the myelocytic lineage of hematopoiesis in the blood test. Even minor concentrations of dividing and maturing cells are considered a variant of the pathological condition.
The detection of juvenile forms of granulocytes indicates that the body is at risk and is struggling with one of the following diseases or pathological processes:
- acute bacterial and viral infections, most often complicated by purulent inflammation. These may be purulent tonsillitis, other severe infections of the ENT organs, acute pyelonephritis, pneumonia, cholera, sepsis, scarlet fever, tuberculosis, typhoid fever, brucellosis, paratyphoid fever, measles, mumps, rubella, etc.
- conditions after severe infectious and inflammatory processes;
- appendicitis and other acute surgical pathology;
- gangrene;
- severe burn disease;
- strokes, heart attacks;
- acute blood loss of any origin;
- metastasis to the bone marrow;
- tumor collapse syndrome;
- consequences of chemotherapy, radiation treatment;
- long-term use of cytostatic, immunosuppressive medications;
- lead poisoning;
- alcoholism;
- all types of coma;
- acidosis;
- shock;
- heavy and constant physical activity;
- many types of anemia;
- leukemia;
- myeloid leukemia;
- deficiency of cyanocobalamin and/or folic acid.
If the concentration of blast cells in the blood is increased slightly - up to 2% of the total leukocyte mass - then we are talking about chronic leukemia.
High values of blasts in the blood are a sign of severe disruptions in the activity of the bone marrow, which indicates acute leukemia.
An excess of the number of blast cells in the blood of more than 5% indicates the development of a blast crisis in patients with chronic myeloid leukemia, as well as the terminal stage in oncological pathology.
The detection of myelocytes, promyelocytes and metamyelocytes in the blood of no more than 5% does not indicate the presence of hematological diseases, but still indicates the presence of certain health difficulties.
But a significant increase from 10% and above is a very unfavorable indicator; it is a marker of myeloproliferative diseases - chronic leukemia, which originate from young cells of the myeloid lineage of hematopoiesis.
The most common reason for the detection of myelocytes and other maturing cells of leukocytopoiesis is chronic myeloid leukemia, the substrate of which is predominantly immature neutrophil myelocytes and other young forms.
At the initial stages of the disease, the growth of myelocytes is not pronounced. The progression of myeloid leukemia is accompanied by a significant increase in myelocytes in the blood, as well as mature eosinophils and basophils. A sharp increase in immature neutrophils, i.e., neutrophilic myelocytes, is an extremely unfavorable sign that worsens the course of leukemia and the prognosis.
Functions of neutrophils
Neutrophils are capable of active movement and can move outside the blood vessels. Mostly they move to the site of inflammation. Neutrophils can carry out phagocytosis, but are able to absorb only small particles, so they are classified as microphages. After absorption of foreign cells, they die, and a large number of active substances are released, which lead to damage to harmful microorganisms, enhance inflammatory processes and the movement of immune cells to the site of infection.
From neutrophils, tissues destroyed as a result of inflammation, and microorganisms that caused this process, a mass is formed, which is known to everyone as pus. The main function of these granulocytes is protection against fungal and bacterial infections. They protect significantly less against viruses and do not take part in protection against helminths and tumors. In acute bacterial infections, the very first immune response is neutrophilic. It is always ahead of the specific lymphocytic one. At the same time, in chronic processes the role of neutrophils is small; in this case, the lymphocytic response predominates.
Functions of basophils
The main function of basophils is to participate in the formation of an immediate allergic reaction, an example being anaphylactic shock. They instantly react to insect and snake bites, blocking their venom and preventing it from spreading throughout the body. There are other functions of basophilic granulocytes. They participate in the regulation of blood clotting thanks to the heparin found in their cytoplasm. On their surface, basophils carry immunoglobulin E; they can release the contents of granules into the external environment and dissolve cells upon contact with an allergen. When cells degranulate and dissolve, large amounts of histamine, prostaglandins, serotonin, leukotrienes and other bioactive substances are released. As a result, an allergic reaction to the allergen that has entered the body is observed. Basophils can penetrate and live outside of blood vessels. They are capable of phagocytosis, although this function is not natural for them. Their main purpose is instant degranulation, which increases blood flow, increases vascular permeability, ensures fluid flow and attracts other granulocytes to the site of inflammation.
Morphology
Granulocytes are the most numerous, making up 40-80% of the total number of leukocytes. The biological norm for the content of GRA in the blood is 2 9 thousand per 1 mm3.
Granulocytes grow in the bone marrow from a universal precursor cell, the myeloblast. Under the influence of various inducers of granulocytopoiesis and granulocyte-stimulating factors, the myeloblast goes through several stages of development (promyelocyte, myelocyte, young metamyelocyte, band, segmented). Full ripening occurs in 9 days.
Granulocytes are divided into:
- Immature granulocytes.
- Rods.
- Segmented (mature).
In the dilated AC, neutrophils are arranged in order of increasing cell maturity from left to right: first young, then band-nuclear, and segmented on the right. In extreme situations (infection), a deficiency of neutrophils occurs in the blood. To compensate for the deficiency, immature granulocytes enter the blood en masse. The increase in the total number of neutrophils in this case will be shifted to the left.
After entering the bloodstream, granulocyte cells are divided into 2 groups: freely circulating and parietal. Parietal granulocytes are temporarily adhered to the surface of blood vessels. The ratio of free and adherent granulocytes is regulated by chemokines and corticosteroids. Adherent granulocytes perform the function of a reserve, which is involved in the process of the immune response when agents are released into the blood, under the influence of which granulocytes detach from the walls of blood vessels and rush into the bloodstream.
A granulocyte cell circulates in the blood for no longer than a week. Then it enters the tissue, where it lives for about 2 days. Having fulfilled its function, it dies.
Important! Granulocytes are the main element of innate nonspecific immunity. In their area of competence, immediate granulocyte-dependent immune reactions occur before the onset of a delayed humoral immune response. The result of a decrease in granulocytes is sensitivity to infections.
The absolute value of GRA is determined by subtracting agranulocytes (lymphocytes and monocytes) from the number of total leukocytes. The relative (percentage) amount of GRA is determined by calculating the percentage of granulocytes to the total number of leukocytes.
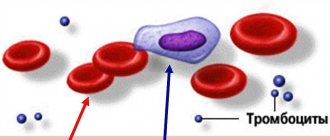
Neutrophils
They got their name because of their ability to be colored with acidic and alkaline dyes. The grain size is fine and dusty. The nucleus is bipartite. In the results, AKs are designated as NEUT, or NE.
Mature neutrophils are phagocytes, but they, unlike monocyte macrophages, are capable of capturing small particles, and therefore are called microphages.
When foreign tissues are detected, neutrophils absorb and dissolve them, after which they die. Dead neutrophils make up the bulk of the pus. Neutrophils die and release substances that damage the membranes of bacteria and fungi, and contribute to increased inflammation and chemotaxis (accumulation) of other immune cells at the site.
The bulk of granulocytes are neutrophils. Of the total number of leukocytes, they range from 42 to 65 percent. Immature (band) neutrophils are normally found in an amount of 1-5% of the total number of leukocytes.
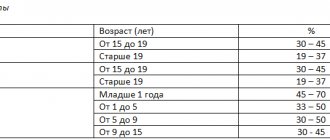
The norm of neutrophils varies depending on age. In children under one year of age, the number of mature neutrophils is smaller due to an increase in the number of lymphocytes and ranges from 15 to 30% of the number of all leukocytes. The number of neutrophils in a child rises to 70% by the age of 15.
Neutrophilia is an increased content of neutrophils, neutropenia is a decreased content. The complete absence of granulocytes is called agranulocytosis.
Eosinophils
They stain with acidic eosin, which is why they got their name. The grain size is large and evenly distributed throughout the cytoplasm. The core consists of 4-5 lobules. In the analysis results it is designated EO, EOS.
Eosinophils are capable of amoeboid movement, penetrate into tissues, and have the properties of a phagocyte. But phagocytosis is not their specific function, like that of neutrophils. After eosinophil degranulation, cytotoxins are released and are therefore considered a major factor in antiparasitic immunity.
Eosinophils are not as numerous as neutrophils. Normal values are 120-350 cells per 1 microliter (1-1.5%).
Basophils
Painted with basic dye. They contain a basophilic (unsegmented) S-shaped nucleus. Granules of different sizes, non-uniformly distributed. The granules consist of allergomediators (histamine, serotonin, prostaglandins). Designated BA. Basophils differ from other granulocytes in size. They are much larger.
Despite the fact that basophils are considered microphages, phagocytosis is not their main function. Their main task is instant degranulation and release of allergomediators at the site of inflammation. This increases vascular permeability, increases blood flow, which ultimately enhances the mobilization of other leukocytes to the area of inflammation.
Basophils, interacting with IgE antibodies, carry out an immediate reaction. An example of such a reaction is anaphylactic shock.
The normal number of basophils is 0-1%.
Functions of eosinophils
Eosinophilic granulocytes are able to actively move and penetrate beyond the bloodstream. They can be called phagocytes, although phagocytosis is not their main function. They can only absorb small cells, so they are classified as microphages. They have cytotoxic properties, so their main function is to participate in antiparasitic immunity. They absorb and bind histamine and other mediators of inflammation and allergies. Like basophils, they can release these substances. Thus, eosinophilic granulocytes are capable of both suppressing an allergic reaction and performing a pro-allergic function.
Basophils increase in the blood during allergies
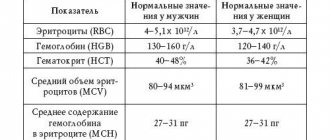
Normal granulocytes
The content of granulocytes is determined during a general blood test, both absolute and relative quantities are calculated.
The norm of granulocytes for adult men and women is from 1.2 to 6.8X10⁹ per liter of blood. Relative content (percentage of the total number of leukocytes) – from 47 to 72%.
Elevated granulocytes during pregnancy are considered a physiological norm, but if their level is high and continues to increase, there is a high probability of developing pathology. You can read about the reasons for the increase in white blood cells during pregnancy here.
The norm for children may differ under the age of 12 years. This is especially true for the percentage of certain types of granulocytes. After 12 years, the norm for a child is the same as for adults.
Analysis for the content of basophils in the blood
As a rule, the content of basophils in the blood is determined during a general blood test. To do this, blood is most often taken from the patient's finger. Biological fluid from a vein is also suitable for such analysis. The essence of the method is to count all leukocyte units under a microscope. It is called the leukocyte formula.
When performing this analysis, the number of not only basophilic granulocytes, but also other leukocytes is determined. The result is most often given as a percentage of the cellular elements of leukocytes to each other.
Why are granulocytes elevated?
We also recommend: Why are basophils in the blood low?
The reasons for the increase in granulocytes may be different. Most often they are elevated due to inflammatory processes occurring in the body. The most common include:
- acute infectious diseases;
- parasitic infections;
- diseases accompanied by necrotic processes;
- intoxication;
- malignant tumors;
- recent infectious disease;
- vaccinations;
- taking certain medications;
- allergies.
Neutrophilia is caused by the following factors:
- acute bacterial infections;
- endogenous and exogenous intoxications;
- acute hemorrhages;
- myeloproliferative diseases;
- taking medications.
This is what neutrophilia looks like on a blood smear
Eosinophilia indicates the development of:
- parasitic diseases;
- allergic reactions;
- tumors;
- non-parasitic infections;
- skin diseases;
- immune diseases;
- endocrine disorders;
- heart pathologies;
- systemic connective tissue diseases.
Causes of basophilia:
- ulcerative colitis and other gastrointestinal inflammations;
- Hodgkin's syndrome;
- allergy;
- blood diseases;
- hemolytic anemia;
- taking medications.
What to do if basophils are elevated
If you receive unpleasant test results, do not panic. Perhaps the reason for the increase in white blood cell levels is not so terrible. You should take a second test in a couple of days to draw any conclusions. If everything is confirmed, you should immediately consult a doctor. In the case of basophilia, you should not self-medicate, because this can harm the health of both an adult and a child. Only a specialist has the right to prescribe competent treatment, depending on the diagnosis and individual characteristics of the body.
How to reduce basophils
This problem is an indicator of various diseases. That is why it is necessary to make an accurate diagnosis and carry out effective therapy. Then the level of white cells will decrease. What treatment may the doctor prescribe:
- In severe cases, such as leukemia, a bone marrow transplant is required.
- For allergic reactions leading to respiratory diseases, antihistamines may be prescribed.
- Bacterial infections are treated with antibiotics.
If the doctor did not identify any pathology, but the analysis showed an increased content of basophils, the diet should be normalized, perhaps go on a diet, increase the intake of foods containing iron (animal liver, beans, seafood). In order for the microelement to be absorbed faster, it is better not to eat foods that interfere with the absorption of iron (for example, milk). Doctors often prescribe vitamin B12 injections. It promotes hematopoiesis, improves bone marrow function, and destroys “bad” cholesterol.