0
Author of the article: Marina Dmitrievna
2018.07.04
1 315
Heart attack
Recently, doctors are increasingly faced with situations where heart attacks occur in people at a young age. A kind of “rejuvenation” of coronary myocardial disease and deaths after attacks are an alarming signal. About one thousand people, regardless of gender, account for 7% of heart attacks. In pregnant women, a similar situation occurs with a frequency of 1 case per 10 thousand births.
Heart attack at age 20
Causes and factors of myocardial infarction in young people?
The main risk factor for the disease is atherosclerosis of those vessels that are responsible for supplying blood to the heart. But there are other risk factors that are no less common:
- genetics;
- smoking;
- excess body weight;
- high blood pressure;
- passive lifestyle, lack of physical activity;
- taking hormonal contraceptives;
- problems with glucose tolerance.
Despite the extensive list of risks, the reasons often remain unclear. Anything can provoke a violation. To reduce the likelihood of disease, you need to be attentive to your health from a young age, play sports, lead an active life, and give up bad habits.
When a young person has suffered a heart attack, the impact of several factors on the body is often revealed. With poor genetics and a high risk of arterial stenosis, the likelihood of a heart attack is 2 times higher, and the threat of unexpected death is 4 times higher.
In addition to such pathology as early vascular atherosclerosis, heart attacks in young people are caused by:
- disturbance of coronary blood flow, provoking spasm of the coronary arteries;
- bleeding disorder, which leads to thrombosis and thromboembolism;
- dissection of the coronary vessels;
- abnormalities in the structure of arteries;
- problems with the coronary arteries - toxic or infectious-allergic in nature, usually with secondary fibrosis.
Workarounds
The average age of patients who come to our cardiac surgery department is about 70 years.
We joke a lot about this, complain that there are not enough young people, but we are secretly proud of this fact: if a patient undergoes heart surgery at the age of 65–70, this significantly increases his chances of living to 80–90 years, bringing joy to his loved ones. Moreover, the hearts of many elderly patients, even those who have suffered a heart attack, work well: cholesterol plaques in their vessels grew gradually, the body managed to adapt to them and form bypass vascular pathways. This allows the heart to be more resistant to sudden disruption of blood supply, and in the event of a heart attack they have something to save. Another thing is young patients 35–45 years old. The point is not that having a heart attack at such a young age is simply offensive and for such patients it is like a bolt from the blue. Their heart turns out to be completely unprepared for such a turn of events, and the affected area of the heart muscle, which in an elderly person could at the very least last until surgery, quickly dies in young people. It is the young who most often develop complications such as heart rupture or the formation of an aneurysm - a saccular cavity, the walls of which have turned into fibrous tissue incapable of contraction.
Article on the topic No disasters! How to support your heart after a heart attack
Pathogenesis and developmental symptoms
Myocardial infarction is a pathological condition, which is complemented by a disruption in the flow of blood to the heart muscle and the death of its parts. Circulatory problems occur due to the cessation of arterial blood flow when the body cannot meet the oxygen needs of the heart. As a result, the myocardium stops receiving nutrition and a heart attack occurs.
The mechanism of sequential progression of pathology is as follows:
- partial blockage of one or more coronary arteries;
- secondary oxygen starvation of heart tissue, causing a malfunction in its functioning;
- the myocardium does not receive nutrition, and therefore partially dies.
With timely assistance to the victim, the process ends with scarring and subsequent cardiosclerosis.
If left untreated, an acute heart attack can be fatal. Regardless of the age group, it will not be possible to restore myocardial function without professional medical assistance.
Pathogenesis and symptoms
At a young age, a heart attack appears suddenly and becomes the first and only sign of heart problems. In most cases, a person does not even complain of heart pain. And sometimes less than 1 week passes between the symptoms that foreshadow trouble and the attack itself.
Symptoms of myocardial infarction vary depending on the stage of progression of the condition.
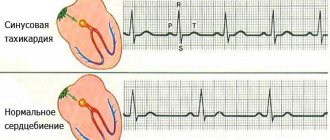
- Pre-infarction period: shortness of breath, rapid heartbeat, cold sweat, pain in the heart under the influence of narrowing of the lumen of the coronary vessel and the formation of a blood clot.
- The most acute stage: necrosis may form within half an hour, severe pain develops behind the sternum, radiating to the arm, shoulder blade and neck on the left, the temperature rarely rises, panic appears, sweating increases, acrocyanosis occurs against the background of pallor of the skin, and the condition is also accompanied by pain in the epigastrium and abdomen, less often vomiting.
- Acute stage: over the course of 2–14 days, the muscle tissue of the heart melts, the pain subsides against this background, but shortness of breath and acrocyanosis persist, chills and dizziness are added to the pathological symptoms, blood tests show an increased ESR, the leukocyte count shifts to the left.
- Subacute stage: scarring of the myocardium occurs, this process can drag on for 1 - 2 months, during which all clinical symptoms of the disease subside, the condition slowly returns to normal.
- Post-infarction stage: complete retreat of symptoms and return of laboratory diagnostic indicators to normal indicates the completion of scarring and the heart’s adaptation to the scar.
Yes, the possibility of recovery after a heart attack remains, but more often the consequences cannot be restored. At a young age, timely diagnosis and assistance are important.
Symptoms
The classic (typical, anginal) form of myocardial infarction is characterized by the following symptoms:
- Chest pain. It can occur gradually, as with angina pectoris. Over time, the pain intensifies. Its duration is more than 30 minutes. The pain is constant, stabbing, pressing or burning, radiating to the shoulder blades, teeth, jaw, neck or shoulder. Unlike an attack of angina, during a heart attack the pain syndrome does not disappear after taking nitrates.
- Paleness of the skin.
- Weakness.
- Cardiopalmus.
- Dyspnea.
- Anxiety.
- Increased sweating.
- Increased body temperature.
- Anxiety.
- Frequent breathing.
- Feeling of fear of death.
- Loss of consciousness.
Signs of pulmonary edema and arrhythmia often appear. The acute period lasts only 2 hours. Symptoms are due to myocardial necrosis. The acute period of a heart attack lasts up to 10 days or more. It is followed by subacute and post-infarction periods.
Atypical forms of heart attack are becoming increasingly common. They are distinguished by specific symptoms and the absence of severe chest pain. The disease can occur under the guise of asthma, arrhythmia, gastrointestinal pathology, collapse and stroke. The following symptoms are observed:
- dizziness, headache, nausea, vomiting, speech impairment, visual disturbances, paresis and tinnitus (signs of a cerebral form of infarction);
- edema (occurs with the edematous form of the disease);
- shortness of breath and attacks of suffocation (characteristic of the asthmatic form of myocardial infarction);
- dyspepsia (abdominal pain, bowel dysfunction, bloating).
The severity of symptoms in young people depends on the depth and size of the necrosis zone. Extensive transmural myocardial infarction is the most severe. Symptoms of heart attack in women do not have specific features.
Diagnostics
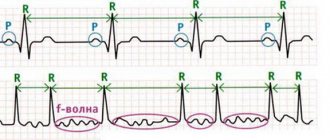
If necrotic damage to myocardial tissue is suspected, an electrocardiogram is immediately prescribed. The examination will confirm or refute abnormalities in the heart, will help establish the rhythm of its work and the presence of necrotic foci.
Conducting a survey
Immediately after admission to the hospital, blood is drawn for laboratory diagnostics and analysis to detect necrotic changes.
If time permits, MRI, vascular ultrasound with Doppler, angiography, and echocardiography are organized. Typically, these methods help determine the extent of necrosis and its exact location.
Treatment of pathology
The very first signs of a heart attack require immediate first aid:
- calling an ambulance;
- ensuring fresh air enters the room;
- laying the victim horizontally, with a pillow under the head, to reduce the volume of blood circulating in the brain;
- eliminate any tight clothing;
- give an Aspirin tablet to prevent thrombosis;
- give Nitroglycerin to relieve pain;
- measure blood pressure, periodically repeating measurements, recording the level to transmit information to health workers.
While waiting for the medical team, it is important to monitor your heartbeat and breathing. In case of an unexpected stop, artificial ventilation of the lungs and indirect cardiac massage are required.
First aid
The purpose of subsequent inpatient treatment:
- stop a painful attack;
- prevent dangerous life-threatening complications;
- normalize coronary circulation;
- limit the progression of necrosis.
Complete rest, strict bed rest, taking narcotic analgesics, and oxygen inhalations are prescribed for 3–4 days. Thrombolytic treatment and reducing cholesterol concentrations during this period will help improve blood composition, and nitroglycerin and beta blockers will begin to restore and regulate heart function.
Inpatient therapy lasts approximately 1 month, then is carried out on an outpatient basis. The doctor definitely recommends special nutrition and an active lifestyle.
Modern technologies help diagnose disorders in a timely manner, so cardiologists can assess the condition of the myocardium even before an attack, prescribing effective treatment that prevents the problem.
If, after admission to the hospital and assistance, the pain in the heart does not subside, inhalation anesthesia is performed with a gas mixture of nitrous oxide and oxygen. Then oxygen therapy is organized and all necessary medications are administered. Also included in medications are:
- nitro-containing drugs to reduce the load on the myocardium;
- anticoagulants to prevent thrombosis;
- beta-blockers - to reduce the load on the myocardium, relieve tachycardia;
- antiarrhythmic drugs - to maintain proper heart function;
- ACE inhibitors to normalize high blood pressure;
- sedatives, hypnotics to reduce anxiety and normalize sleep.
Depending on concomitant diseases, the doctor may supplement therapy with other medications.
In severe cases, surgery may be prescribed: coronary artery bypass surgery, balloon angioplasty. This will prevent deterioration of health and reduce the risk of death.
If the vessel is completely blocked and stent placement is prohibited, an open operation is first performed, which involves replacing the valves with artificial ones. Only then is the stent inserted.
Recovery after a heart attack
It is allowed to get out of bed only from the 3rd day, provided there are no complications.
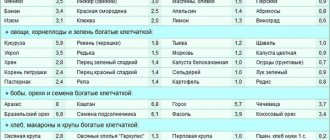
In the first month after a heart attack, the patient is prescribed a low-calorie diet and is required to give up fatty foods, foods with fiber, salt and large amounts of liquid. In the first days, only pureed food is allowed.
In general, according to statistics, the mortality rate from heart attacks in young people is not too high. But at the same time, relapse often occurs due to the more aggressive course of the pathology compared to older people.