Atrial fibrillation, or atrial fibrillation (AF), is a heart rhythm disorder characterized by irregular contractions of the atria and ventricles, which in many people is paroxysmal in nature. Such patients often feel the development of paroxysm (attack). In this case, it will be useful for them and their relatives to know how to provide first aid for atrial fibrillation.
It is quite difficult to independently recognize the development of the first attack of atrial fibrillation in your life. However, for most paroxysmal rhythm disturbances, the principles of first aid are the same. Therefore, our article will be useful to read for all people suffering from paroxysmal heart rhythm disturbances (supraventricular or ventricular tachycardia).
Primary diagnosis of heart rhythm disorders
The essence of this heart rhythm disorder is completely irregular heartbeats, which can be independently detected during the initial diagnosis. During an attack of atrial fibrillation, the pulse is usually diagnosed as frequent (on average more than 100 per minute) and irregular. This can be determined by feeling the pulse waves on the wrist, or by measuring blood pressure using a mechanical or semi-automatic blood pressure monitor.
When measuring pressure with an automatic tonometer, most devices display a measurement error message or display an arrhythmia icon on the display. However, this does not mean that atrial fibrillation has occurred; automatic tonometers react this way to any rhythm disturbance that interferes with the correct measurement of pressure.
Some patients do not feel that they are experiencing an episode of rapid, irregular heartbeat. If the normal heart rhythm is not restored, after a few days such patients develop symptoms and characteristic signs of heart failure:
- shortness of breath when lying down, inability to sleep normally, feeling stuffy; the patient goes out onto the street or balcony, sits down, in this position it becomes easier for him;
- weakness, dizziness;
- swelling of the feet and legs, sudden “tightness” of shoes, the appearance of elastic marks from socks on the skin.
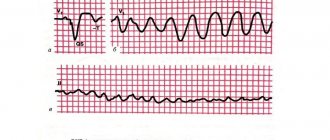
With such symptoms, you must call an ambulance or a doctor at home. The arriving ambulance team will register an ECG, which will show the characteristic signs of atrial fibrillation (atrial fibrillation).
The danger of atrial fibrillation attacks for the heart
The danger of attacks directly depends on the form of atrial fibrillation. If the attacks can be stopped, that is, they can be eliminated, this must be done. Of course, it is better to choose a treatment so that paroxysms occur as rarely as possible. However, gradually, in most cases, the paroxysmal (attack-like) form of atrial fibrillation becomes permanent. In this case, another treatment is necessary - aimed at slowing down the pulse and preventing blood clots.
When an attack (paroxysm) of atrial fibrillation develops, the patient has an increased likelihood of thromboembolic complications, primarily stroke, as well as myocardial infarction.
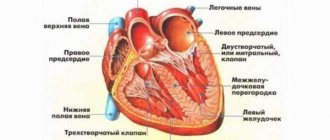
This is because the sudden onset of chaotic heartbeats disrupts the normal flow of blood into the heart and causes platelets to deposit on its inner walls. These cells form clots, which break off and travel to large arteries, such as the brain.
The faster the attack is stopped, the less the risk of complications of atrial fibrillation.
Reasons for the development of pathology
Patients suffering from AF are not always aware of their disease, and often learn about it only during a medical examination.
- All information on the site is for informational purposes only and is NOT a guide to action!
- Only a DOCTOR can give you an ACCURATE DIAGNOSIS!
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist!
- Health to you and your loved ones!
| Paroxysmal | Occurs periodically, the heartbeat normalizes after a few hours without medication. |
| Constant | Unable to stabilize heart rate. |
| Persistent | Needs treatment because the heartbeat cannot recover on its own. |
| Difficulty breathing |
|
| Cardiopalmus | During AF, strong tremors of the heart are felt, it seems that it is about to “jump out” of the chest. |
| Dizziness | A common sign of a dangerous condition. Often accompanied by nausea and can lead to fainting. |
| Increased fatigue | Severe fatigue is explained by the active work of the heart, similar to that during high physical activity. |
| Disorientation | Uneven blood supply to the brain leads to a malfunction in its functioning. Due to the lack of oxygen, confusion may be felt. |
| Chest pain | The progression of AF is accompanied by squeezing and pressing painful sensations. |
Most heart diseases have similar symptoms to atrial fibrillation. Pathologies can be distinguished by the pulse - an uneven and rapid heartbeat is a sure sign of AF.
To date, several causes of AF have been identified. Patients prone to the disease require regular examination. Timely detection of fibrillation ensures fast and productive treatment. While advanced pathology can provoke other heart diseases and lead to stroke.
Treatment of diseases that can lead to AF significantly reduces the risk of its development.
The causes of the paroxysmal form of atrial fibrillation are always associated with cardiovascular diseases. Therefore, people with any heart pathologies are at risk. According to statistics, atrial fibrillation occurs in approximately 9% of all elderly people and in most cases it is provoked by ischemic heart disease (CHD).
The main reasons leading to the development of paroxysmal arrhythmia include:
- valvular heart failure;
- hypertrophic cardiomyopathy;
- inflammation of the heart of infectious origin;
- chronic hypertension;
- rheumatism;
- previous heart attack or ischemic stroke;
- lung cancer, embolism, pneumonia;
- amyloidosis;
- severe forms of anemia;
- thyrotoxicosis;
- hemochromatosis;
- chemical poisoning; drug overdose;
- myxoma of the heart;
- emphysema;
- electric shock;
- weakness of the sinus node.
In addition to the diseases listed above, the onset of the disease can be triggered by the following factors:
- exhaustion of the nervous system;
- abuse of energy drinks, tobacco products;
- pathological changes in the respiratory system;
- regular stress;
- infectious invasion;
- chronic renal failure;
- obesity of the third degree.
Paroxysmal atrial fibrillation sometimes occurs some time after heart surgery. In all cases where the attack was not associated with diseases and did not occur under the influence of certain negative factors, the paroxysm is called idiopathic.
Forms of atrial fibrillation
Atrial fibrillation (atrial fibrillation) can occur in several variants (forms):
- paroxysmal form: usually the patient has a normal sinus rhythm, but periodically it “breaks down” and an attack of irregular heartbeat develops, usually rapid;
- persistent form: the patient’s usual rhythm is atrial fibrillation, but sometimes due to unknown reasons, his normal heartbeat is restored for some time;
- permanent form: only an irregular heartbeat is recorded, sinus rhythm is not restored.
And also, depending on the average pulse frequency, tachysystolic, normo- and bradysystolic forms of atrial fibrillation are distinguished.
Tachysystolic form - an increase in the average heart rate of more than 100 per minute.
Normosystolic form with heart rate from 60 to 100 beats,
Bradysystolic form is a decrease in heart rate of less than 50 - 60 per minute.
In the paroxysmal course of MA, attacks usually have a high heart rate.
Treatment of atrial fibrillation and flutter
What are the recommendations for antithrombotic therapy? How to choose a drug for preventive antiarrhythmic therapy?
Atrial fibrillation (AF) is one of the most common tachyarrhythmias in clinical practice, its prevalence in the general population ranges from 0.3 to 0.4% [1]. The detection of AF increases with age. Thus, among people under 60 years of age it is approximately 1% of cases, and in the age group over 80 years of age it is more than 6%. About 50% of patients with atrial fibrillation in the United States are over 70 years of age, and more than 30% of those hospitalized for cardiac arrhythmias are patients with this arrhythmia [2]. Atrial flutter (AFL) is a significantly less common arrhythmia compared to AF. In most countries, AF and AFL are considered different rhythm disorders and are not combined under the common term “atrial fibrillation.” In our opinion, this approach should be considered correct for many reasons.
Prevention of thromboembolic complications and relapses of atrial fibrillation and flutter
Atrial fibrillation and flutter worsen hemodynamics, aggravate the course of the underlying disease and lead to an increase in mortality by 1.5-2 times in patients with organic heart disease. Non-valvular (non-rheumatic) AF increases the risk of ischemic stroke by 2-7 times compared to the control group (patients without AF), and rheumatic mitral disease and chronic AF - by 15-17 times [3]. The incidence of ischemic stroke in non-rheumatic atrial fibrillation averages about 5% of cases per year and increases with age. Cerebral emboli recur in 30-70% of patients. The risk of another stroke is highest during the first year. The risk of stroke is low in patients with idiopathic AF under 60 years of age (1% per year), slightly higher (2% per year) at the age of 60-70 years. In this regard, most patients with frequent and/or prolonged paroxysms of atrial fibrillation, as well as its permanent form, should be prevented from thromboembolic complications. A meta-analysis of all studies on primary and secondary prevention of strokes showed that indirect anticoagulants reduce the risk of developing the latter by 47-79% (on average by 61%), and aspirin by a little more than 20%. It should be noted that when using aspirin, a statistically significant reduction in the incidence of ischemic stroke and other systemic embolisms is possible only with a fairly high dose of the drug (325 mg/day) [4]. At the same time, in the Copenhagen AFASAK Study [5], the number of thromboembolic complications in the groups of patients receiving aspirin 75 mg/day and placebo did not differ significantly.
In this regard, patients with AF who are at high risk for thromboembolic complications: heart failure, EF 35% or less, arterial hypertension, ischemic stroke or transient ischemic attack in history, etc., should be prescribed indirect anticoagulants (maintaining the International Normalized ratio - INR - on average at the level of 2.0-3.0). For patients with non-valvular (non-rheumatic) atrial fibrillation who are not at high risk, continuous use of aspirin (325 mg/day) is advisable. There is an opinion that in patients under 60 years of age with idiopathic AF, in whom the risk of thromboembolic complications is very low (almost the same as in people without rhythm disturbances), preventive therapy may not be required. Antithrombotic therapy in patients with AFL should obviously be based on taking into account the same risk factors as in AF, since there is evidence that the risk of thromboembolic complications in AFL is higher than in sinus rhythm, but somewhat lower than in AF [ 6].
International experts offer the following specific recommendations for antithrombotic therapy for various groups of patients with atrial fibrillation, depending on the level of risk of thromboembolic complications [7]:
- age less than 60 years (no heart disease - lone AF) - aspirin 325 mg/day or no treatment;
- age less than 60 years (heart disease, but no risk factors such as congestive heart failure, EF 35% or less, arterial hypertension) - aspirin 325 mg/day;
- age 60 years or more (diabetes mellitus or coronary artery disease) - oral anticoagulants (INR 2.0-3.0);
- age 75 years or more (especially women) - oral anticoagulants (INR up to 2.0);
- heart failure - oral anticoagulants (INR 2.0-3.0);
- LVEF 35% or less - oral anticoagulants (INR 2.0-3.0);
- thyrotoxicosis - oral anticoagulants (INR 2.0-3.0);
- arterial hypertension - oral anticoagulants (INR 2.0-3.0);
- rheumatic heart defects (mitral stenosis) - oral anticoagulants (INR 2.5-3.5 or more);
- artificial heart valves - oral anticoagulants (INR 2.5-3.5 or more);
- history of thromboembolism - oral anticoagulants (INR 2.5-3.5 or more);
- the presence of a thrombus in the atrium, according to TPEchoCG, - oral anticoagulants (INR 2.5-3.5 or more).
The international normalized ratio should be monitored with indirect anticoagulants at the beginning of therapy at least once a week, and subsequently monthly.
In most cases, patients with recurrent paroxysmal and persistent atrial fibrillation in the absence of clinical symptoms of arrhythmia or their insignificant severity do not need to be prescribed antiarrhythmic drugs. In such patients, prophylaxis of thromboembolic complications (aspirin or indirect anticoagulants) and heart rate control are carried out. If clinical symptoms are pronounced, anti-relapse and relief therapy is required, combined with heart rate control and antithrombotic treatment.
In case of frequent attacks of atrial fibrillation and flutter, the effectiveness of antiarrhythmics or their combinations is assessed clinically; in case of rare attacks, TES or VEM is performed for this purpose after 3-5 days of taking the drug, and when using amiodarone - after saturation with it. To prevent relapses of AF/AFL in patients without organic heart disease, antiarrhythmic drugs of classes 1A, 1C and 3 are used. In patients with asymptomatic LV dysfunction or symptomatic heart failure, and possibly with significant myocardial hypertrophy, therapy with class 1 antiarrhythmics is contraindicated due to the risk of worsening life prognosis.
To prevent paroxysms of atrial fibrillation and atrial flutter, the following antiarrhythmics are used: quinidine (kinylentine, quinidine durules, etc.) - 750-1500 mg/day; disopyramide - 400-800 mg/day; propafenone - 450-900 mg/day; allapinin - 75-150 mg/day; etacizin - 150-200 mg/day; flecainide - 200-300 mg/day; amiodarone (maintenance dose) - 100-400 mg/day; sotalol - 160-320 mg/day; dofetilide - 500-1000 mcg/day. Verapamil, diltiazem and cardiac glycosides should not be used for anti-relapse therapy of AF and AFL in patients with Wolff-Parkinson-White syndrome (WPU), since these drugs reduce the refractoriness of the accessory atrioventricular conduction pathway and can cause aggravation of the arrhythmia.
In patients with sick sinus syndrome and paroxysms of atrial fibrillation and flutter (bradycardia-tachycardia syndrome), there are expanded indications for implantation of an electrical pacemaker (pacemaker). Permanent pacing is indicated in such patients both for the treatment of symptomatic bradyarrhythmia and for the safe administration of preventive and/or curative antiarrhythmic therapy. To prevent and relieve attacks of AF and AFL in patients without pacemakers, class 1A antiarrhythmics with anticholinergic effects (disopyramide, procainamide, quinidine) can be used. In hypertrophic cardiomyopathy, amiodarone is prescribed to prevent tachyarrhythmia paroxysms, and beta-blockers or calcium antagonists (verapamil, diltiazem) are prescribed to reduce the frequency of ventricular contractions.
As a rule, treatment with antiarrhythmics requires monitoring the width of the QRS complex (especially when class 1C antiarrhythmics are used) and the duration of the QT interval (when treated with class 1A and 3 antiarrhythmics). The width of the QRS complex should not increase by more than 150% of the initial level, and the corrected QT interval should not exceed 500 ms. Amiodarone has the greatest effect in preventing arrhythmia [14, 15, 16, 17]. A meta-analysis of published results from placebo-controlled studies involving 1465 patients showed that the use of low maintenance doses of amiodarone (less than 400 mg/day) did not cause an increase in lung and liver damage compared with the placebo group [8]. Some clinical studies have demonstrated a higher preventive effectiveness of class 1C drugs (propafenone, flecainide) compared to class 1A antiarrhythmics (quinidine, disopyramide). According to our data, the effectiveness of propafenone is 65%, ethacyzine - 61% [9, 10].
Choice of drug for prophylactic antiarrhythmic therapy of paroxysmal and persistent atrial fibrillation and flutter
We can agree with the opinion expressed in international recommendations for the management of patients with atrial fibrillation [7], according to which anti-relapse therapy in patients without heart pathology or with minimal structural changes should begin with class 1C antiarrhythmics (propafenone, flecainide). Let's add to them domestic drugs of the same class (allapinin and etacizin), as well as sotalol; they are quite effective and devoid of pronounced extracardiac side effects. If the listed antiarrhythmics do not prevent relapses of AF/AFL or their use is accompanied by side effects, you should proceed to prescribing amiodarone and dofetilide. Then, if necessary, class 1A drugs (disopyramide, quinidine) or non-pharmacological treatments are used. Probably, in patients with so-called “adrenergic” AF, one can expect a greater effect from therapy with amiodarone or sotalol, and in “vagal” AF it is advisable to start treatment with disopyramide.
Coronary heart disease, especially in the presence of post-infarction cardiosclerosis, and heart failure increase the risk of manifestation of the arrhythmogenic properties of antiarrhythmic drugs. Therefore, treatment of atrial fibrillation and flutter in patients with congestive heart failure is usually limited to the use of amiodarone and dofetilide. While the high efficacy and safety of amiodarone in heart failure and coronary artery disease (including myocardial infarction) has been proven for a long time, similar results for dofetilide were obtained in the recent placebo-controlled studies DIAMOND CHF and DIAMOND MI [11].
For patients with coronary heart disease, the recommended sequence of prescribing antiarrhythmics is as follows: sotalol; amiodarone, dofetilide; disopyramide, procainamide, quinidine.
Arterial hypertension, leading to hypertrophy of the left ventricular myocardium, increases the risk of developing polymorphic ventricular tachycardia “torsades de pointes”. In this regard, to prevent relapses of AF/AFL in patients with high blood pressure, preference is given to antiarrhythmic drugs that do not significantly affect the duration of repolarization and the QT interval (class 1C), as well as amiodarone, although it prolongs it, but extremely rarely causes ventricular tachycardia . Thus, the algorithm for pharmacotherapy of this rhythm disorder in arterial hypertension appears to be as follows: LV myocardial hypertrophy of 1.4 cm or more - use only amiodarone; There is no left ventricular myocardial hypertrophy or it is less than 1.4 cm - start treatment with propafenone, flecainide (bear in mind the possibility of using domestic class 1C antiarrhythmics allapinin and etacizin), and if they are ineffective, use amiodarone, dofetilide, sotalol. At the next stage of treatment (ineffectiveness or occurrence of side effects of the above drugs), disopyramide, procainamide, and quinidine are prescribed [7].
It is quite possible that with the emergence of new results from controlled studies on the effectiveness and safety of antiarrhythmic drugs in patients with various diseases of the cardiovascular system, changes will be made to the above recommendations for the prevention of relapses of paroxysmal and persistent AF, since at present the relevant information is clearly insufficient.
If there is no effect from monotherapy, combinations of antiarrhythmic drugs are used, starting with half doses. An addition, and in some cases an alternative to preventive therapy, as mentioned above, may be the prescription of drugs that worsen AV conduction and reduce the frequency of ventricular contractions during paroxysms of AF/AFL. The use of drugs that impair conduction in the AV junction is justified even in the absence of effect from preventive antiarrhythmic therapy. When using them, it is necessary to ensure that the heart rate at rest is from 60 to 80 per minute, and with moderate physical activity - no more than 100-110 per minute. Cardiac glycosides are ineffective for controlling heart rate in patients leading an active lifestyle, since in such cases the primary mechanism for reducing the frequency of ventricular contractions is an increase in parasympathetic tone. Therefore, it is obvious that cardiac glycosides can be chosen only in two clinical situations: if the patient suffers from heart failure or has low physical activity. In all other cases, preference should be given to calcium antagonists (verapamil, diltiazem) or beta-blockers. In case of prolonged attacks of atrial fibrillation or flutter, as well as in their permanent form, combinations of the above drugs can be used to reduce heart rate.
Relief of paroxysms of fibrillation and atrial flutter
The primary task during an attack of the tachysystolic form of AF/AFL is to reduce the heart rate, and then, if the paroxysm does not stop on its own, stop it. Control of the ventricular contraction rate (decrease to 70-90 per minute) is carried out by intravenous administration or oral administration of verapamil, diltiazem, beta-blockers, intravenous administration of cardiac glycosides (preference is given to digoxin), amiodarone. In patients with reduced LV contractile function (congestive heart failure or EF less than 40%), heart rate is reduced only with cardiac glycosides or amiodarone. Before stopping tachysystolic forms of atrial fibrillation and atrial flutter (especially atrial flutter) with class 1A antiarrhythmics (disopyramide, procainamide, quinidine), conduction blockade in the AV node is required, since the above-mentioned antiarrhythmic drugs have an anticholinergic effect (most pronounced with disopyramide) and can significantly increase the frequency contractions of the ventricles.
Considering the risk of thromboembolism during prolonged paroxysm of AF, the issue of stopping it must be resolved within 48 hours, since if the duration of an attack of AF exceeds two days, it is necessary to prescribe indirect anticoagulants (maintaining the INR at the level of 2.0-3.0) for 3-4 weeks before and after electrical or drug cardioversion. Currently, the most widely used indirect anticoagulants are coumarin derivatives: warfarin and syncumar. If the duration of AF is unknown, the use of indirect anticoagulants before and after cardioversion is also necessary. Similar prevention of thromboembolic complications should be carried out in case of atrial flutter.
For pharmacological cardioversion, the following antiarrhythmics are used:
- amiodarone 5-7 mg/kg - intravenous infusion over 30-60 minutes (15 mg/min);
- ibutilide 1 mg - intravenous administration over 10 minutes (if necessary, repeated administration of 1 mg);
- novocainamide 1-1.5 g (up to 15-17 mg/kg) - intravenous infusion at a rate of 30-50 mg/min;
- propafenone 1.5-2 mg/kg - intravenous administration over 10-20 minutes;
- flecainide 1.5-3 mg/kg - intravenous administration over 10-20 minutes.
The international recommendations for cardiopulmonary resuscitation and emergency cardiac care [12] and the ACC/AHA/ECC recommendations for the treatment of patients with atrial fibrillation [7] note that it is advisable to relieve paroxysm in patients with heart failure or EF less than 40% mainly with amiodarone. The use of other antiarrhythmics should be limited due to the rather high risk of developing arrhythmogenic effects and the negative impact of these drugs on hemodynamics.
The use of verapamil and cardiac glycosides is contraindicated in patients with AF/AFL and Wolff-Parkinson-White syndrome. In the presence of the latter, AF/AFL is treated with drugs that impair conduction along the Kent bundle: amiodarone, procainamide, propafenone, flecainide, etc.
Oral relief of atrial fibrillation and flutter with quinidine, procainamide, propafenone, flecainide, dofetilide, etc. is possible.
Atrial flutter (type 1) can be relieved or converted to AF by frequent transesophageal or endocardial atrial pacemaker. Stimulation is prescribed for a duration of 10-30 seconds with a pulse frequency that is 15-20% higher than the frequency of atrial contractions, i.e. 300-350 (400) pulses per minute.
When AF/AFL is accompanied by severe heart failure (cardiac asthma, pulmonary edema), hypotension (systolic pressure less than 90 mm Hg), increased pain and/or worsening myocardial ischemia, immediate electrical pulse therapy (EPT) is indicated.
In case of atrial fibrillation, EIT begins with a discharge with a power of 200 J; for biphasic current, the energy of the first discharge is less. If it turns out to be ineffective, discharges of higher power (300-360 J) are successively applied. Atrial flutter is often relieved by a low-energy shock (50-100 J).
Electropulse therapy can also be chosen for the planned restoration of sinus rhythm in patients with prolonged paroxysms of AF/AFL. Medical cardioversion is recommended if EIT is not possible, undesirable, or fails to restore sinus rhythm. In case of an attack of AF/AFL lasting more than 48 hours, indirect anticoagulants before cardioversion can not be used for a long time if transesophageal echocardiography (TPEchocardiography) excludes the presence of thrombi in the atria (in 95% of cases they are localized in the left atrial appendage). This is the so-called early cardioversion: intravenous administration of heparin (increase in aPTT by 1.5-2 times compared to the control value) or short-term administration of an indirect anticoagulant (bringing the INR to 2.0-3.0) before cardioversion and four weeks of indirect administration anticoagulants after restoration of sinus rhythm. According to preliminary data from the ACUTE multicentre study [13], the incidence of thromboembolic complications is significantly lower when using TPEchoCG and short courses of preventive therapy with heparin or warfarin (in the absence of a thrombus) or longer-term administration of an indirect anticoagulant (if a thrombus is re-detected after three weeks of warfarin treatment) before EIT, than with traditional therapy carried out “blindly” with indirect anticoagulants for 3-4 weeks before and after electrical cardioversion, and is 1.2% and 2.9%, respectively. In patients who do not receive anticoagulants before cardioversion, thromboembolic complications develop in 1-6% of cases.
For severe paroxysms of AF and AFL, refractory to drug treatment, non-pharmacological treatment methods are used: destruction of the AV connection with implantation of an electrical pacemaker, “modification” of the AV connection, implantation of an atrial defibrillator or special pacemakers, radiofrequency catheter destruction of the impulse circulation path in the right atrium during AFL and sources ectopic impulses in patients with focal atrial fibrillation, “corridor” and “labyrinth” operations.
Literature
1. Kastor JA Arrhithmias. Philadelphia: WB Saunders company 1994. P.25-124. 2. Bialy D., Lehmann MN, Schumacher DN et al. Hospitalization for arrhythmias in the United States: importance of atrial fibrillation (abstr) // J. Am. Coll. Cardiol. 1992; 19:41A. 3. Wolf PA, Dawber TR, Thomas HE, Kannel WB Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study // Neurology. 1978; 28: 973-77. 4. The Stroke Prevention in Atrial Fibrillation Study Group Investigators. Stroke prevention in atrial fibrillation study: final results//Circulation. 1991; 84:527-539. 5. Petersen P., Boysen G., Godtfredsen J. et al. Placebo-controlled, randomized trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study // Lancet. 1989; 1: 175-179. 6. Biblo LA, Ynan Z, Quan KJ et al. Risk of stroke in patients with atrial flutter // Am. J. Cardiol. 2000; 87: 346-349. 7. ACC/AHA/ESC guidelines for management of patients with atrial fibrillation//Circulation. 2001; 104: 2118-2150. 8. Vorperian VR, Havighurst TC, Miller S., Janyary CT Adverse effect of low dose amiodarone: a meta-analysis // JACC. 1997; 30: 791-798. 9. Bunin Yu. A., Fedyakina L. F., Bayroshevsky P. A., Kazankov Yu. N. Combined preventive antiarrhythmic therapy with etatsizin and propranolol for paroxysmal fibrillation and atrial flutter. Materials of the VII Russian National Congress “Man and Medicine”. Moscow, 2000. P. 124. 10. Semykin V.N., Bunin Yu.A., Fedyakina L.F. Comparative effectiveness of combined antiarrhythmic therapy with propafenone, verapamil and diltiazem for paroxysmal fibrillation and atrial flutter. Materials of the VII Russian National Congress “Man and Medicine”. Moscow, 2000. pp. 123-124. 11. Sager PT New advances in class III antiarrhytmic drug therapy. Curr. Opin. Cardiol. 2000; 15: 41-53. 12. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care // Circulation. 2000; 102 (suppl I): I-158-165. 13. Design of a clinical trial for the assessment of cardiversion using transesophageal echocardiography (the ACUTE multicenter study) // Am. J. Cardiol. 1998; 81: 877-883. 14. Bunin Yu. A., Firstova M. I., Enukashvili R. R. Maintenance antiarrhythmic therapy after restoration of sinus rhythm in patients with a permanent form of atrial fibrillation. Materials of the 5th All-Russian Congress of Cardiologists. Chelyabinsk, 1996. P. 28. 15. Bunin Y., Fediakina L. Low doses of amiodarone in preventing of paroxysmal atrial fibrillation and flutter. International academy of cardiology. 2nd international congress on heart disease. Abstract book of the congress, Washington, USA, 2001. 16. Gold RL, Haffajec CI Charoz G. et al. Amiodarone for refractory atrial fibrillation // Am. J. Cardiol. 1986; 57: 124-127. 17. Miller JM, Zipes DP Management of the patient with cardiac arrhythmias. In Braunwald E., Zipes D., Libby P. (eds). Heart disease. A textbook of cardiovascular medicine. Philadelphia: WB Saunders company. 2001. P. 731-736.
General rules for first aid
The rules for providing first aid for the treatment of paroxysm of atrial fibrillation are carried out differently depending on several characteristics of the attack:
- blood pressure level;
- shortness of breath at rest;
- duration of the attack;
- heart rate;
- primary or repeated paroxysm.
Depending on this, emergency doctors either try to restore sinus rhythm or reduce the heart rate, while simultaneously preventing the formation of blood clots. For this purpose, medications are used, and, if necessary and conditions exist, electropulse therapy is used.
What you can and cannot do at home during an attack
If an attack of irregular heartbeat develops, you must immediately call an ambulance.
Before the medical team arrives, you can:
- give the patient a semi-sitting position;
- unbutton tight clothes;
- provide fresh air access to the room;
- invite the patient to breathe with his stomach, wipe his face with a handkerchief dipped in cold water;
- give 20 - 30 drops of Corvalol in half a glass of water;
- prepare for the arrival of the team: organize its meeting, prepare medical documents, previous ECGs, think about transporting the patient to the ambulance (such a need may arise, but the duties of the ambulance personnel do not include carrying the patient);
- reassure the patient, tell him to call the doctors.
When detecting an attack of MA before the arrival of the ambulance, you cannot:
- give the patient medications before the ambulance arrives, including nitroglycerin;
- massage the eyeballs or the area of the carotid arteries;
- waste time measuring blood pressure without preparing for the arrival of medical personnel;
- collect things for hospitalization (this will be the time while the doctor examines the patient, relieves the attack, etc.; hospitalization is not always required);
- worry and panic.
How to stop an attack of MA on your own (a pill in your pocket)
Some patients whose diagnosis of “paroxysmal atrial fibrillation” has been established for a long time, and attacks occur less than once a month, can learn to independently stop such paroxysms. This tactic is called “pill in the pocket.”
It is used in intellectually intact patients who can adequately assess their condition. The “pill in your pocket” strategy should not be used if the next attack of arrhythmia caused any new symptoms:
- chest pain;
- dizziness;
- weakness in the limbs;
- facial asymmetry and so on.
In such cases, you should not stop the paroxysm on your own, since these symptoms may be a sign of the development of a heart attack or stroke.
If paroxysmal fibrillation proceeds as usual, the patient can take the drug propanorm at a dosage of 450–600 mg.
The patient should consult his cardiologist in advance about in what cases and in what dose to take this medicine. It is better if the first dose of propanorm is taken in a hospital, under the supervision of medical professionals.
Supraventricular paroxysmal tachycardia
NPTs combine a group of rhythm disorders in which the ectopic pacemaker is localized above the common trunk of the atrioventricular bundle. There are sinoatrial, atrial and atrioventricular (nodal) supraventricular tachycardias. In most cases, they have a similar ECG picture and their accurate diagnosis without special research is difficult. When establishing a diagnosis in the prehospital setting, they are usually limited to the general formulation: supraventricular paroxysmal tachycardia.
Causes
The most common causes of NPT are various heart diseases, an imbalance of the autonomic nervous system, general intoxication, chronic nonspecific lung diseases, the toxic effects of certain medications, and the presence of additional impulse pathways.
Manifestations
NPT is characterized by:
• sudden onset and end of an attack;
• usually a regular rhythm with a frequency of 150-250 per minute;
• the frequency of ventricular contractions corresponds to the frequency of atrial contractions (or less in the presence of A-V blockade);
• the P wave, as a rule, is not differentiated;
• complexes, as a rule, are narrow (they can expand with blockade of the legs of the atrioventricular bundle, Wolff-Parkinson-White syndrome);
First aid and treatment
Relief of paroxysm of supraventricular tachycardia with narrow complexes should begin with vagal tests (irritation of the vagus nerve and slowing of conduction through the atrioventricular node): Valsalva test - sharp straining after a deep breath, immersing the face in cold water, inducing vomiting.
If there is no effect in patients with stable hemodynamics, drug therapy should be used. The drugs of choice are adenosine (ATP) or the calcium antagonist verapamil. The advantages of adenosine when administered intravenously compared with a calcium antagonist or β-blinker are its rapid onset of action and short half-life.
If adenosine is ineffective, it is advisable to administer a calcium antagonist - verapamil (extends the refractory period in the atrioventricular node), the duration of action is up to 30 minutes. Verapamil is administered intravenously as a bolus of 5-10 mg (2-4 ml) in isotonic sodium chloride solution over 2-4 minutes. If tachycardia persists and there is no arterial hypotension, verapamil is reintroduced after 15 minutes at a dose of 5-10 mg. It is not recommended to administer intravenous verapamil if a P-blocker was administered within 2 hours before.
In the absence of ATP and verapampl, it is possible to use the P-blocker propranolol or the cardiac glycoside digoxin. However, the effectiveness of these drugs is significantly lower than that of ATP and verapamil, and they also have a more distant onset of action. If tachycardia persists, after 15-20 minutes you can use one of the following drugs:
• procainamide 10% - 10 ml in 10 ml of isotonic sodium chloride solution intravenously over 8-10 minutes;
• or propafenone at a dose of 1-2 mg/kg intravenously over 10 minutes;
• or amiodarone at a dose of 5 mg/kg in 20 ml of isotonic sodium chloride solution or 5% glucose solution intravenously for 8 minutes (is the drug of choice in patients with severe left ventricular dysfunction).
If there are signs of hemodynamic disturbances in patients with NPT, electrical cardioversion (100 J) or transesophageal pacing is indicated.
Patients with newly diagnosed paroxysm of supraventricular tachycardia, intractable paroxysm and paroxysm complicated during treatment are subject to hospitalization.
Algorithm of emergency care for atrial fibrillation
Emergency care during an attack of atrial fibrillation (AF) is provided by a linear ambulance team, or less often by a cardiac team. In any case, it is first recommended to administer a “blood thinning” drug, for example, heparin, then the algorithm of actions will depend on the general state of health and the severity of the attack.
After assessing the patient’s condition, ambulance doctors can apply one of three treatment tactics:
- Antiarrhythmic drugs
- Cardiac glycosides
- Electropulse therapy
Antiarrhythmic drugs (cautious tactics)
Normalizing the pulse rate without stopping the attack is a “cautious tactic” that is used when the patient’s condition is unstable – low blood pressure, the duration of the attack is more than 48 hours, the first episode of atrial fibrillation, shortness of breath at rest, fever. Depending on the heart rate, the patient is given antiarrhythmic drugs and, if necessary, antishock drugs, and hospitalization is suggested. If the pulse rate is from 60 to 100, the patient may not be hospitalized; in this case, on the same or the next day he is visited by a local therapist (he is called by the ambulance team).
Cardiac glycosides (drug treatment)
For drug relief of an attack, cardiac glycosides are used, as well as one of 2 antiarrhythmic drugs, primarily these:
- Cordarone;
- Sotalol.
It is also advisable to administer sedatives and sedatives. Novocainamide is now rarely used to relieve an attack of atrial fibrillation due to its side effects. If the paroxysm is stopped, the patient usually remains at home.
Electropulse therapy (emergency care)
Electrical pulse therapy for paroxysmal AF is a type of emergency treatment used by emergency cardiac teams for urgent indications, for example, arrhythmic shock. In this condition, due to a sudden rhythm disturbance, the contractility of the heart sharply decreases, which leads to a significant decrease in pressure and oxygen starvation of the brain. In this condition, transporting the patient to the hospital is life-threatening, so doctors use electropulse therapy. The method involves applying one or more electrical discharges to the heart area, restoring normal heart rhythm. Before this, the patient is given intravenous painkillers and sedatives.
Complications: what happens if help is not provided in a timely manner?
Not in all cases, the attack can be stopped effectively and quickly - for example, according to doctors, in 10% of cases only electric pulses help, and drugs are powerless. What consequences can result from failure to provide assistance to a patient? In case of atrial fibrillation, emergency assistance must be provided urgently, otherwise a change in the intensity of blood flow will occur, and with it an embolism in the atrium.
Negative consequences also develop, such as:
- Pulmonary edema and acute heart failure - the course of the disease is significantly aggravated;
- Hypoxic shock - it is caused by a sharp decrease in pressure and a disruption in the supply of oxygen to organs. Most often, this consequence provokes too frequent muscle contraction;
- Fainting;
- Heart attack or angina - caused by disturbances in coronary blood flow;
- Formation of blood clots - when urgent medication is ignored, and more than 2 days have passed since the onset of the attack, clots form in the blood. They clog blood vessels, leading to death of limbs, gangrene, and stroke.
However, such severe complications are not a reason to panic. It is quite possible to stop an attack without consequences for your health, you just need to not ignore the signs of an attack that has begun.