3.5 / 5 ( 4 voices)
Many people quite often complain of a sensation that is described as fluttering of the heart. The causes of this condition must be reliably established, because further treatment tactics will depend on this.
Is bird-like heart fluttering the result of emotions or pathological changes in the body?
The information, photos, drawings and videos in this article will help you get an idea of why the heart flutters like a bird, what types of heart “fluttering” there are and the symptoms that accompany it, the dangers of not treating such a disorder, and what are the main methods of treating it in a hospital and at home.
The mechanism of pathology development
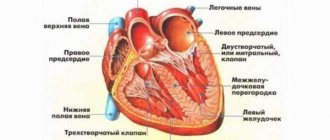
Normally, the heart contracts at a certain frequency in two phases. The first is systole. Maximum tension of cardiac structures. The second is diastole. Relaxation, temporary rest of tissues.
The generation of a signal that ensures muscle work occurs in the sinus node. This is a small collection of cardiomyocytes. Further along the bundles of His, the signal moves to other similar structures and is conducted to the ventricles.
In the case of atrial flutter, an electrical impulse is generated in the atria. Hence the extra contractions outside the normal rhythm.
The intensity of the signals, however, is low, which ensures the relative correct functioning of the myocardium. This is a temporary phenomenon, with a 60% chance of fibrillation occurring within 2-3 years, and eventually death.
There is another mechanism: abnormal movement of the impulse in the right atrium. Develops due to disorders of the conduction system (bundle of His, Bachmann). The signal loops and moves in a circle, provoking repeated excitation of muscle tissue.
Symptoms of atrial flutter
The disease is characterized by common symptoms that occur in many cardiovascular diseases:
- heart rate is increased;
- “interruptions” of cardiac activity, sensations of “fading” and “turning over” of the heart;
- Heart failure is manifested by weakness, shortness of breath, and frequent urination.
With atrial flutter, sinus rhythm is maintained, which is regular and rhythmic, which distinguishes this pathology from atrial fibrillation.
Venous pulsation is another characteristic sign of atrial flutter. When determining it, a difference with heart contractions is visible, which consists in an exaggeration of the pulsation frequency of the veins by two to three times.
Atrial flutter is considered clinically unfavorable if the ratio of atrial and ventricular contraction rates is 1:1. This option is very dangerous due to the high risk of developing ventricular fibrillation.
Forms of flutter
In clinical practice, there are two types of flutter.
The typical form is characterized by normal impulse movement in the myocardium of the right atrium. Usually counterclockwise. Reverse development of the condition is possible, clockwise.
The direction does not play a big role, although it can confuse the young doctor. The heart rate is limited to 150-300 beats per minute. They are incomplete, so they are almost not felt.
The risks of complications are minimal, but this is temporary. There is a possibility of aggravation of the pathological process.
The atypical form is characterized by abnormal movement of the electrical impulse. It also affects the left atrium, as well as the isthmus of the venous mouth.
The heart rate is high and is determined by the figure of 300-450 beats per minute. Symptoms are also minimal; such myocardial movements are not felt as full-fledged.
Normosystole, tachy- and brady-: the concept of how it is reflected on the ECG, norm and deviations
All materials are published under the authorship or editorship of medical professionals (about the authors), but are not a prescription for treatment. Contact the specialists!
The patient cannot always independently interpret the medical terms read in the electrocardiogram protocol. Of course, only a doctor can decipher the cardiogram itself and the resulting conclusion, but what should you do before your appointment? First, decide on the terminology and try to understand for yourself whether your cardiogram is normal or not.
Normosystole refers to sinus heart rhythm, accompanied by a normal heart rate - from 55-60 to 80-90 per minute. It is this heart rate that allows the heart muscle to work without increased load on the myocardium, while at the same time providing the necessary cardiac output to supply blood to the internal organs.
normosystole on ECG
Bradysystole and tachysystole, in turn, indicate a slowdown and acceleration of the heart rhythm, respectively. Read about these abnormalities on the ECG in separate materials - bradysystole, tachysystole.
heart function is normal - in sinus rhythm
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Sometimes the ECG conclusion may include a combination of normosystole and irregular sinus rhythm - “normosystole, irregular rhythm.” The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.
Of all rhythm disturbances, only this type of arrhythmia, such as fibrillation or atrial flutter, is divided into normo-, tachy- and bradysystolic variants. In this case, the diagnosis “atrial fibrillation, normosystole” indicates a pathology in the form of arrhythmia, but with a normal final heart rate.
normosystolic form of atrial fibrillation - despite the “waves” of atrial flutter/fibrillation, contraction of the ventricles of the heart occurs at a normal frequency
In this case, we are talking about both a permanent form of atrial fibrillation, when a person lives for a long time (months and years) with an irregular or non-sinus rhythm, and a paroxysmal form (paroxysm - attack), when a non-sinus rhythm occurs suddenly and may well recover spontaneously or with the help of medications. Diagnostic criteria are similar to those for normo-, brady- and tachysystole in sinus rhythm - from 60 to 80, less than 60 and more than 80 beats per minute, respectively.
With a permanent form of atrial fibrillation, normosystole is usually more easily tolerated by patients in terms of the sensation of interruptions in the work of the heart, since bradysystole is fraught with a decrease in cardiac output and resulting fainting, and the heart rate during tachysystole sometimes reaches 200 beats per minute, which can lead to severe circulatory disorders.
Treatment of paroxysmal atrial fibrillation with normosystole is strictly necessary, because paroxysm, even with a normal heart rate, requires emergency drug restoration of rhythm. Typically, drugs such as cordarone, procainamide, and a polarizing mixture are administered intravenously.
A patient with normosystole with a permanent form of atrial fibrillation must take drugs such as digoxin, aspirin to prevent blood clots, and sometimes warfarin for the same purpose. Rhythm-slowing therapy for normosystole should be treated with extreme caution, since metoprolol, bisoprolol, verapamil and similar drugs can provoke a significant slowdown in heart rate and cause bradycardia with loss of consciousness.
In conclusion, it should be said once again that normosystole with the correct sinus rhythm is a sign of normal functioning of a healthy heart, therefore this term only indicates that according to a specific ECG everything is in order.
Classification according to the nature of the flow
A more important clinical classification is the course of the pathological process. Based on this criterion, they call:
- Primary atrial flutter. It occurs spontaneously; as a rule, no episodes have been observed before, so it is impossible to determine the etiology, as well as predict the further progression of the process. Requires hospitalization and long-term outpatient observation.
- Paroxysmal form. The most common. Paroxysm of atrial flutter lasts from 10 minutes to several hours. It is characterized by intense symptoms from the cardiac structures, and the patient’s general well-being is disrupted. In case of a prolonged episode, emergency transesophageal electrical stimulation is performed, which stops the attack.
- Persistent type. Characterized by disruption of normal heart rhythm on a regular basis. Unlike previous forms, the duration of episodes can be several days. Such prolonged paroxysms require urgent help, there is a risk of cardiac arrest.
- Permanent form. Stabilization of the condition in a pathological direction requires a number of years of development. In other cases, everything happens faster. Recovery is carried out in a hospital. Conservative methods do not always have an effect; radical help is often required.
A big role is played not by the duration of the attack, but by the severity with which it occurs. The main assessment factors are the frequency of contractions, the general well-being of the patient, the presence of concomitant manifestations of the cardiac structures and nervous system.
Causes of the primary form of TP
Factors in the development of the pathological process are not always cardiac. Depending on the main point provoking the onset of arrhythmia, primary and secondary (extracardiac) forms are distinguished.
- SVC syndrome. Congenital heart defect. It is characterized by the formation of an extra conductive bundle (bundle of Kent), which provides excessive excitation of cardiac structures.
Accompanied by severe symptoms. Atrial flutter is one possibility, but not the most common. According to statistics, the frequency of this form is 0.3-0.5%, fibrillation, which is also probable, is detected in almost 4% of cases.
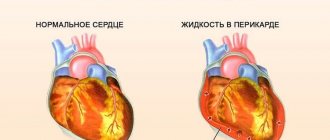
- Infectious-inflammatory or autoimmune lesions of the heart muscle, pericardium. The symptoms are also pronounced, which will not allow you to ignore the condition. Treatment is carried out in a hospital with the use of antibiotics, corticosteroids, and, as necessary, immunosuppressants in minimal dosages.
The acute process entails destruction of the atria in the short term. Recovery in such a situation is surgical with no guarantee of success. The same consequence of a long-term chronic process with frequent relapses.
- Cardiomyopathy. Impaired development of the heart muscle. There are several forms. They are all similar in one thing: normal muscle tone decreases, its volume increases or decreases, depending on the type of process. It is possible to expand the chambers of cardiac structures. Treatment makes sense only in the early stages. Then there is a symptomatic effect, it fights the effect, not the cause.
- Heart defects, congenital and acquired. The most common disorders are functional activity and anatomical development of valves (aortic, mitral). The correction is strictly surgical, in a short time. According to indications. Going under the knife, so to speak, without sufficient reason is not a good idea.
- Heart attack and subsequent cardiosclerosis. From the point of view of dangerous complications, the threat is posed not so much by the acute death of heart cells itself, but by the subsequent scarring of the affected areas.
Areas of rough connective tissue appear. They do not contract, do not have elasticity, and do not conduct signals.
Hence the disruption of the normal functional activity of cardiac structures. The same effect is provoked by myocarditis, other inflammatory pathologies, ischemic disease, and coronary insufficiency.
Complications
This form of AF can cause complications. Stroke and embolism are the most serious of these. Blood inside the heart can clot and form blood clots. These clots can travel through the bloodstream and, once they reach the brain, cause a stroke. Blood clots can also travel to the lungs, intestines and other sensitive organs, blocking blood flow and causing thromboembolism, which leads to tissue death, which is extremely life-threatening.
If AF persists for a long period of time without treatment, the heart can no longer effectively pump blood and oxygen throughout the body. This could potentially lead to heart failure.
Paroxysmal atrial fibrillation can lead to complications such as pulmonary embolism
Causes of the secondary form of TP
Extracardiac factors also occur, their share in the total number of causes is up to 40%. These are secondary forms of atrial flutter:
- Extrasystole. Not of cardiac origin. The occurrence of spontaneous myocardial contractions of unknown etiology. Over time, it provokes tertiary changes in rhythm.
- Hyperthyroidism. Excessive synthesis of thyroid hormones. Intensifies the work of all body systems. Cardiovascular including. Recovery is carried out under the supervision of an endocrinologist. Therapy lasts from 3 months to a year or more. It is also necessary to address the root cause of the condition.
- Diabetes.
- Respiratory failure in the subcompensation phase or a completely uncontrolled process. Accompanied by hypoxia. Diagnoses vary: asthma, COPD, emphysema, and other conditions.
- Metabolic problems. Characterized by a deviation in the metabolism of potassium, magnesium, sodium (to a lesser extent).
Causes
Causes of atrial flutter may include heart problems or heart disease, diseases in other parts of the body that affect the heart, or substances that modify the way electrical impulses are transmitted through the heart. In some people, the underlying cause of the disease cannot be identified.
Heart diseases or pathologies that may cause atrial flutter include the following:
- Decreased blood flow to the heart (ischemia) due to coronary artery disease, atherosclerosis, or a blood clot;
- High blood pressure (hypertension);
- Disease of the heart muscle (cardiomyopathy);
- Pathologies of the heart valves (especially the mitral valve);
- Enlargement of the chambers of the heart (hypertrophy);
- Disorders resulting from open heart surgery.
Other diseases (in other parts of the body) that may affect the heart:
- Hyperthyroidism of the thyroid gland;
- Blood clot in a blood vessel in the lungs (pulmonary embolism)
- Chronic obstructive pulmonary disease (COPD), which reduces oxygen levels in the blood.
Substances that can contribute to the development of atrial flutter:
- Alcohol (wine, beer or spirits);
- Stimulants such as ephedrine, cocaine, amphetamines, diet pills, and even caffeine;
Atrial flutter is closely related to another type of arrhythmia called atrial fibrillation. These two types of arrhythmias sometimes alternate with each other.
Risk factors
A major role is played by factors that cannot strictly be classified as pathological, but increase the degree of danger:
- Long-term smoking. Experienced tobacco consumers are at greater risk. In this case, not only the duration is important, but also the body’s own resistance. It is assumed that it is genetically determined.
- Senile age. From 60 years and over.
- Being male. According to various estimates, the likelihood of atrial flutter is 6-8 times higher compared to women.
Trigger factors
The onset of an attack can be spontaneous or provoked by triggers:
- Consumption of coffee, tea, alcoholic beverage (does not depend on quantity).
- Smoking.
- Intense stress.
- Physical overload.
- High air temperature, humidity, unfavorable climatic conditions. Especially in the summer months. People with heart disease are advised to go outside as little as possible.
- Excess fluid the day before. Especially against the background of renal pathologies of a dysfunctional nature, when the evacuation of urine is impaired.
- Addiction to drugs, psychoactive drugs, use of drugs of the glucocorticoid group and others.
Prognosis and possible complications
The outcome depends on the stage at which the disorders were detected. In the early stages, the probability of full recovery is close to 100%.
If organic changes occur, the heart grows, the chances of successful treatment drop sharply to 60-70%. The later stages cannot be corrected at all, and maintaining vital functions also does not seem likely. An organ transplant is required.
Complications are also factors in the death of patients:
- Heart failure. Spontaneous or against the background of developed deterioration. In severe general condition there is no prospect of resuscitation.
- Cardiogenic shock.
- Thromboembolism and subsequent stroke or myocardial infarction. Acute nutritional disorder of structures.
Elimination of the consequences of emergency conditions is also futile if the process has been going on for a long time and has been started.
Symptoms
The clinical picture is nonspecific. It is impossible to tell about the nature of the process and its origin based on the manifestations. However, attacks clearly indicate health problems and motivate you to see a doctor.
Approximate symptoms:
- Heart rhythm disturbance. Subjectively, it is felt as a sharp blow, an incorrect, too frequent beating, or missed contractions. Against the background of the course of mixed processes, the intensity of symptoms may increase.
- Chest pain. Burning or pressing. Not high strength. With the development of acute coronary insufficiency, the sensation is more pronounced. Treatment is carried out with analgesics.
- Tachycardia. Acceleration of cardiac activity. Heart rate reaches 110-120 beats or more.
- Dyspnea. Sudden, excludes any physical activity. Outside of an attack, the manifestation is absent for some time. Gradually it becomes persistent and accompanies the patient constantly.
- Fall in blood pressure. Unimportant. 90 to 70 or so.
- Headache, vertigo, spatial disorientation.
- Weakness, drowsiness, decreased activity.
In some cases, symptoms are completely absent. The intensity of the manifestations is determined by the involvement of the ventricles in the process. If they are not affected, symptoms are usually minimal.
First aid for paroxysm
It is carried out at home or in a hospital. At the same time, on your own, at the pre-hospital stage, it is possible to relieve an attack only in the early stages, when there are no organic defects. With concomitant pathologies, the chances of relief are minimal.
In any case, the algorithm is as follows:
- Call emergency medical assistance.
- Measure blood pressure. Heart rate.
- Open a vent or window to ensure adequate ventilation of the room.
- Take prescribed medications. If you have not yet had a consultation with a cardiologist, you can use Anaprilin (half a tablet). But this is an extreme case. You can’t take anything else to avoid complications.
- Take a semi-lying position and place a cushion made from scrap materials under your back.
- Breathe rhythmically (5 seconds for each movement).
- Calm down. In case of an acute panic attack, take a sedative based on herbal ingredients: motherwort or valerian tablets. Just not alcohol tincture.
- Wait for the specialists to arrive, do not make sudden movements and generally move less.
Upon arrival of the brigade, report the condition. Hospitalization is possible, but it is not recommended to refuse it.
Important things to keep in mind:
First aid is pre-medical. It is not aimed at a total cure. Its task is to stabilize conditions before the arrival of doctors, in order to avoid complications.
Diagnostics
Conducted by a cardiologist. If the origin of the process is controversial, it is recommended to involve third-party specialists: neurologists and others.
Scheme of events:
- Oral questioning of the patient regarding complaints, collection of anamnesis. Both methods play a huge role because they allow you to navigate the situation.
- Measurement of blood pressure, heart rate.
- Auscultation. Listening to the sound created by the contraction and relaxation of cardiac structures.
Routine methods do not provide comprehensive information. They are necessary to determine the vector for further diagnosis.
- Electrocardiography. Identification of functional deviations. The main method of examining patients with atrial flutter.
- Echocardiography. Aimed at identifying complications and organic defects.
- Daily monitoring. Measurement of blood pressure and heart rate over 24 hours in dynamics, taking into account circadian rhythms and patient activity.
As part of advanced diagnostics: blood tests, urine tests, assessment of neurological status, electroencephalography, MRI, thyroid scintigraphy, sugar curve.
Atrial fibrillation: diagnosis
As a rule, this disease is diagnosed already during an external examination of the patient and when collecting an anamnesis. With ordinary palpation of the pulse, it is already possible to determine the chaotic and disordered rhythm of heart contractions. When listening with a phonendoscope, the nature of the irregularity of heart sounds is heard. After this, the patient is referred to a cardiologist.
Further diagnosis includes electrocardiographic examination. 24-hour ECG monitoring is also often used, and tests are carried out with various modes of physical activity (treadmill test, bicycle ergometry).
Structural abnormalities of the heart are determined using echocardiography. Magnetic resonance imaging is also quite effective.
Signs on ECG
Typical features of flutter on a cardiogram:
- Normal ventricular complexes (if these chambers are not affected).
- Absence of P waves.
- Presence of F peaks.
- Acceleration of heart rate to 200-450 beats per minute.
- QRS < 0.12 sec.
- Short PR interval.
The characteristic model of the pathological process is noticeable even to an inexperienced doctor. Gross changes occur even in the early stages. Atrial flutter on the ECG is supplemented by data from 24-hour Holter monitoring.
Treatment methods
Therapy is carried out in three stages:
- Relief of an acute condition.
- Eliminate the root cause.
- Symptomatic effects.
The last two are carried out in parallel.
Solving the problem of bringing the patient out of paroxysm:
- Use of medications. Beta blockers (Anaprilin, Carvedilol have high therapeutic activity, others like Metoprolol are also effective, but give more side effects), calcium channel blockers (Diltiazem as the main one). Also antiarrhythmics (Amiodarone or Hindin) in strictly adjusted dosages.
- If ineffective, electrocardioversion is performed. Elimination of paroxysm by external conduction of current. Effectiveness varies.
- Transesophageal pacing (TEPS) is also possible. The essence remains the same. The technique has a greater effect due to its invasiveness.
Then there is time for advanced diagnostics. Symptomatic therapy with the use of antiarrhythmic, cardiac glycosides in short courses.
In the absence of action, a radical surgical technique is indicated. The main one is radiofrequency ablation - cauterization of the focus that generates an abnormal signal or elimination of the path that conducts the impulse in a circle.
Drug treatment of atrial flutter is the primary measure; surgery is used in extreme cases due to the presence of risks.
Treatment of atrial flutter
Attacks of atrial flutter with the use of modern treatment methods are effectively stopped in most cases. Such areas of medicine as drug therapy and surgical treatment are used. Also important is emergency care in the form of restoration of sinus rhythm, used to stop severe attacks.
Restoration of sinus rhythm
It is an emergency treatment that is performed for atrial flutter by medical personnel. There are several ways to restore sinus rhythm: drug and non-drug cardioversion.
Drug cardioversion is rarely used for AFL because it is not as effective as for atrial fibrillation. Cardioversion begins with intravenous administration of ibutilide, which has the desired effect on average in 60% of cases. If there are contraindications to the use of ibutilide (hypersensitivity to it), amiodarone and sotalol are administered. If there is no result from drug cardioversion, then they resort to heart rate control, which uses calcium antagonists and digoxin.
Non-drug cardioversion is based on electrical impulse therapy. A defibrillator creates a shock of 100 J, which is effective in 85% of cases. For comparison, if you perform cardioversion with a shock of 50 J, then the effectiveness is achieved at 75%. In some cases, with type 1 AFL, it is better to pace the patient using an electrode passed through the esophagus. Sometimes digoxin or an antiarrhythmic drug is additionally administered, which increases the overall effectiveness of the procedure.
With any type of cardioversion, thromboembolism prophylaxis must be carried out, especially if AFL persists for 48 hours.
Drug therapy
Indications for drug treatment are poor patient tolerance to an attack, as well as the presence of a risk of complications.
It is based on the use of beta blockers (metoprolol) under the guise of antiarrhythmic drugs (ibutilide, amiodarone). The administration of the latter drugs is necessary to prevent the occurrence of ventricular fibrillation.
When WPW syndrome develops, beta blockers, cardiac glycosides and other similar drugs cannot be used so as not to provoke a complication of the condition. The only thing is that you can use anticoagulants and antiarrhythmic drugs.
Catheter ablation
Indicated for type 1 atrial flutter, when the impulse circulates counterclockwise. In the area of the isthmus, radiofrequency catheter ablation is performed, which is effective in 95% of cases.
Another type of catheter ablation, cryothermal, has also proven effective, and the procedure is not as painful as radiofrequency ablation. The only thing is that any such interventions are accompanied by a subsequent relapse of tachycardia. In addition, after the procedure, the risk of developing atrial fibrillation increases. This is due to structural changes in the heart chambers. Therefore, surgical treatment should be performed only in extreme cases when other methods, in particular drug treatment, do not help.