ATRIAL SEPTAL DEFECT
Clinical picture
depends on the degree of hemodynamic impairment and changes with the age of the patient. • Complaints - shortness of breath, palpitations, fatigue during physical activity, retardation in physical development and frequent respiratory tract infections. • Examination • Pallor of the skin • Increased cardiac impulse • Auscultation • Systolic murmur in the 2nd and 3rd intercostal spaces to the left of the sternum • Splitting and accentuation of the 2nd tone over the pulmonary artery • Mesodiastolic murmur to the right of the sternum.
Diagnostics
• ECG. Hypertrophy of the right heart, deviation of the EOS to the right and partial blockade of the right branch of the His bundle; sometimes rhythm disturbances (extrasystole, paroxysmal tachycardia, atrial fibrillation). A characteristic sign of a primary ASD is a significant deviation of the EOS to the left. • X-ray examination of the chest organs. The shadow of the heart and the trunk of the pulmonary artery are expanded, the pulmonary pattern is enhanced. • Echocardiography. The right ventricle is enlarged, and paradoxical movement of the interventricular septum is often observed. ASDs can usually be visualized using two-dimensional echocardiography. With color Doppler sonography, the direction of blood shunting is determined and the consistency of the atrioventricular valves is assessed. In adults, transesophageal echocardiography is also performed. • Radionuclide research. Quantitative assessment of radioactivity after the first pass of the radionuclide makes it possible to detect the recirculation of blood in the lungs. • Cardiac catheterization helps to detect an increase in blood oxygenation as the probe passes from the vena cava into the right atrium. Absolutely accurate evidence of the presence of an ASD is the passage of a probe from the right atrium to the left. When a contrast agent is introduced into the left atrium, it refluxes into the right atrium.
Differential diagnosis
• Isolated pulmonary artery stenosis • Famo's triad • Patent ductus arteriosus • Ventricular septal defect • Ebstein's disease • Abnormal drainage of the pulmonary veins • Functional murmur.
Lead tactics. Depending on the size of the ASD and circulatory failure, either outpatient observation or inpatient examination and treatment is indicated. Physical activity after correction of the defect is not limited. Drug treatment. In case of a defect of the primordial septum in combination with mitral regurgitation, prevention of infective endocarditis is indicated. If necessary, correct heart failure.
Surgery
• Indications: • Increase in pulmonary blood flow compared to the total by 2 times or more (excess of arteriovenous discharge by 40% of the minute volume of pulmonary blood flow) • defects of the primordial septum • extensive defects of the secundum septum • concomitant anomalous drainage of the pulmonary veins • Optimal age of the child for testing operations - 4-5 years • The operation consists of suturing the ASD or its plastic surgery; carried out under conditions of artificial circulation or hypothermia. Complications • Heart failure • Arrhythmias • Infective endocarditis • Pulmonary hypertension. Course and prognosis • In early childhood, the course is benign, in rare cases, severe circulatory disorders can lead to death in the first months of life • Spontaneous closure of the defect is possible before the age of 5 • Average life expectancy without treatment - no more than 37-40 years • After After surgical treatment, the prognosis is favorable, the risk of death in the postoperative period does not exceed 1%. Associated pathologies • Mitral stenosis • Abnormal drainage of the pulmonary veins • Multiple congenital heart pathologies. See also: Ventricular septal defect, Patent ductus arteriosus, Tetralogy of Fallot, Atrioventricular canal, Infectious endocarditis.
Abbreviations
• ASD - atrial septal defect
Q21.1 Atrial septal defect Note: A patent foramen ovale is not considered to be a congenital heart disease (in the open foramen ovale there is a valve that closes from the difference in pressure in the atria and prevents pathological discharge of blood).
Choice of treatment tactics
Therapy is divided into conservative and surgical. If you are feeling well and there is no clinic, no treatment is required.
Indications for conservative therapy:
- The defect size is less than 3 mm;
- Arrhythmia;
- Tachycardia;
- Decreased overall body tone.
Drugs used:
- Beta blockers;
- Hypotonics;
- Antiarrhythmic drugs;
- B vitamins;
- Vascular agents and nootropics.
Heart surgery
The operation is performed if complications are present or threatened. Indications :
- Pulmonary hypertension;
- Retarded physical development;
- Right ventricular failure;
- Tendency to respiratory infections.
Types of surgery:
- Excision of the prolapsed area of the septum;
- Installation of a synthetic patch.
Technique
The operation is performed while connecting artificial blood circulation (CPB).
- The patient is put under anesthesia.
- A mid-lateral sternotomy is performed - opening the chest cavity and removing part of the ribs.
- A longitudinal incision provides access to the pericardium.
- The right atrium is opened.
- Its cavity is cleared of blood and the aneurysm is examined.
- The protrusion is removed along the edge of healthy tissue.
- A synthetic patch is applied to the resulting hole.
- The operation is completed by layer-by-layer suturing of the atrium, pericardium and layers of the thoracic cavity.
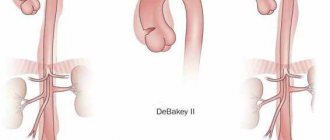
Aorto-iliac prosthetics
The operation is indicated for adult patients with concomitant atherosclerosis. The intervention consists of replacing the aortoiliac branch with a synthetic prosthesis made of inert material. The operation is performed under conditions of artificial circulation. The affected area is removed and replaced with a prosthetic synthetic copy.
If a newborn or older child is sick
If the disease is detected in an infant, treatment is not carried out if the aneurysm occupies no more than a third of the volume of the involved atrium.
A wait-and-see approach is used, since the risk of surgical complications does not always justify surgical intervention. The operation is postponed until the child reaches adolescence . During this period, the newborn is prescribed symptomatic medications, calculating dosages taking into account weight.
In children and adolescents, the need for therapy is determined by the presence of complaints and general condition. In case of pulmonary hypertension above grade 1 and pronounced left-to-right shunt, removal of the aneurysm with the application of a patch is indicated.
When diagnosing an aneurysm, it is very important to follow the rules recommended by your doctor and be attentive to your health. And in order to know more about this disease, we suggest reading important information about what it is, where such lesions of blood vessels and arteries can be located, whether they occur in children, how clipping or removal procedures occur, and what the dangers of this lesion are in such cases. organs and parts of the body such as the brain, lungs, splenic artery, lower extremities, as well as the aorta (ascending, thoracic, descending and arch).
Congenital anomalies [malformations] of the cardiac septum (Q21)
Excludes: acquired cardiac septal defect (I51.0)
Coronary sinus defect
Unclosed or preserved:
- foramen ovale
- secondary hole (type II)
Venous sinus defect
Common atrioventricular canal
Endocardial defect at the base of the heart
Atrial septal defect (type II)
Ventricular septal defect with pulmonary stenosis or artesia, aortic dextroposition and right ventricular hypertrophy.
Aortic septal defect
Eisenmenger's defect
Excluded: Eisenmenger
- complex (I27.8)
- syndrome (I27.8)
Septal defect (heart) NOS
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Short description
Atrial septal defect (ASD) is a congenital heart defect with communication between the atria. Statistical data: 7.8% of all congenital heart disease detected in infancy, and 30% in adults; VSD of the ostium secundum type - 70%, ostium primum - 15%, sinus venosus - 15%; Lutembashe syndrome accounts for 0.4% of all cases of ASD, the combination of ASD with mitral valve prolapse - 10–20%; the predominant gender is female (2:1–3:1).
Code according to the international classification of diseases ICD-10:
- Q21.1 Atrial septal defect
Etiology: factors that form congenital heart disease (see Tetralogy of Fallot).
Pathogenesis • The magnitude and direction of shunt depend on the size of the defect and the relative compliance of the ventricles • In adults, the right ventricle is more compliant than the left, as a result of which shunt occurs from the left atrium to the right • A small shunt leads to a moderate volume overload of the right heart, and pressure in the pulmonary artery remains normal • The severity of pulmonary hypertension may be insignificant even with a large shunt • Only in rare cases does severe pulmonary hypertension develop, leading to right ventricular failure and right-to-left shunt • Unlike VSD, with ASD the shunt is smaller and affects only the right side of the heart.
Congenital heart defect VSD ICD code
- Description
- Additional facts
- Causes
- Classification
- Symptoms
- Diagnostics
- Differential diagnosis
- Treatment
- Course and stages
- Forecast
- Basic medical services
- Clinics for treatment
Q21.0 Ventricular septal defect.
The presence of a defect between the right and left ventricles of the heart.
Description
Ventricular septal defect.
Congenital intracardiac anomaly, characterized by the presence of communication between the right and left ventricles. A ventricular septal defect is manifested by shortness of breath, retarded physical development, fatigue, rapid heartbeat, and the presence of a “heart hump.”
Instrumental diagnosis of ventricular septal defect includes ECG, echocardiography, chest radiography, ventriculography, aortography, catheterization of cardiac chambers, MRI.
For ventricular septal defects, radical (closing the defect) and palliative (narrowing of the pulmonary artery) interventions are performed.
Additional facts
A ventricular septal defect (VSD) is a hole in the septum separating the cavities of the left and right ventricles, the presence of which leads to pathological shunting of blood.
In cardiology, ventricular septal defect is the most common congenital heart defect (9–25% of all congenital heart defects). The incidence of critical illness with ventricular septal defect is about 21%. The defect is found with equal frequency in newborn boys and girls.
A ventricular septal defect may be a single intracardiac anomaly (isolated VSD) or be part of the structure of complex defects (tetralogy of Fallot, truncus arteriosus, transposition of the great vessels, tricuspid valve atresia, etc.).
In some cases, the interventricular septum may be completely absent - this condition is characterized as a single ventricle of the heart.
Features of hemodynamics in ventricular septal defect
The interventricular septum forms the inner walls of both ventricles and makes up approximately 1/3 of the area of each of them. The interventricular septum is represented by membranous and muscular components. In turn, the muscular section consists of 3 parts - inflow, trabecular and outflow (infundibular).
The interventricular septum, along with other walls of the ventricles, takes part in the contraction and relaxation of the heart. In the fetus, it is fully formed by the 4-5th week of embryonic development. If this does not happen for some reason, a defect remains in the interventricular septum.
Hemodynamic disturbances with a ventricular septal defect are caused by communication between the left ventricle with high pressure and the right ventricle with low pressure (normally, during systole, the pressure in the left ventricle is 4-5 times higher than in the right).
After birth and the establishment of blood flow in the systemic and pulmonary circulation, due to a ventricular septal defect, a left-to-right shunt occurs, the volume of which depends on the size of the hole.
With a small volume of shunted blood, the pressure in the right ventricle and pulmonary arteries remains normal or increases slightly. However, with a large flow of blood through the defect into the pulmonary circulation and its return to the left parts of the heart, volumetric and systolic overload of the ventricles develops.
A significant increase in pressure in the pulmonary circulation with large ventricular septal defects contributes to the occurrence of pulmonary hypertension.
An increase in pulmonary vascular resistance causes the development of blood discharge from the right ventricle to the left (reverse or cross-shunt), which leads to arterial hypoxemia (Eisenmenger syndrome).
Long-term practice of cardiac surgeons shows that the best results in closing a ventricular septal defect can be achieved by shunting blood from left to right. Therefore, when planning the operation, hemodynamic parameters (pressure, resistance and volume of discharge) are carefully taken into account.
Causes
Most often, a ventricular septal defect is a consequence of a violation of embryonic development and is formed in the fetus due to disorders of organ formation.
Therefore, ventricular septal defect is often accompanied by other cardiac defects: patent ductus arteriosus (20%), atrial septal defect (20%), aortic coarctation (12%), aortic stenosis (5%), aortic insufficiency (2.5-4. 5%), mitral valve insufficiency (2%), less often - abnormal drainage of the pulmonary veins, pulmonary stenosis, etc. In 25-50% of cases, the ventricular septal defect is combined with malformations of extracardiac localization - Down's disease, anomalies of the kidneys, cleft of the hard palate and cleft lip.
The direct factors causing disruption of embryogenesis are harmful effects on the fetus in the first trimester of gestation: diseases of the pregnant woman (viral infections, endocrine disorders), alcohol and drug intoxication, ionizing radiation, pathological course of pregnancy (severe toxicosis, threat of spontaneous abortion, etc.) . There is evidence of a hereditary etiology of ventricular septal defect. Acquired ventricular septal defects can be a complication of myocardial infarction.
Classification
The size of the ventricular septal defect is assessed based on its absolute size and comparison with the diameter of the aortic opening: a small defect is 1-3 mm (Tolochinov-Roger disease), a medium one is equal to approximately 1/2 the diameter of the aortic opening, a large one is equal to or greater than its diameter .
Taking into account the anatomical location of the defect, the following are distinguished: • perimembranous defects of the interventricular septum - 75% (inflow, trabecular, infundibular) are located in the upper part of the septum under the aortic valve and can close spontaneously; • muscular defects of the interventricular septum – 10% (inflow, trabecular) – located in the muscular part of the septum, at a considerable distance from the valve and conduction systems;
• supracrestal defects of the interventricular septum - 5% - located above the supraventricular crest (the muscle bundle separating the cavity of the right ventricle from its outflow tract), do not close spontaneously.
Source: https://eltransteh.ru/vrozhdennyj-porok-serdca-dmzhp-kod-mkb/
Symptoms (signs)
Clinical picture
Complaints: shortness of breath, palpitations, fatigue during physical activity, retarded physical development, frequent infections, paradoxical embolisms.
Objectively • Pallor of the skin • Harrison's furrows - displacement of areas of the chest as a result of chronic shortness of breath • Splitting of the first tone with a pronounced component of the tricuspid valve • Pronounced fixed splitting of the second tone (pronounced - due to - due to prolongation of the time of blood ejection from the right ventricle; fixed - due to - due to the fact that the dependence of venous return on the phases of breathing is leveled by discharge from the left atrium) • An ejection click and a soft systolic murmur of relative stenosis of the pulmonary artery in the second intercostal space to the left of the sternum • Due to an increase in blood flow through the tricuspid valve, a low-frequency diastolic murmur sometimes occurs above the xiphoid process of the sternum.
Diagnostics
Instrumental diagnostics
• ECG. Signs of hypertrophy and overload of the left sections, and with pulmonary hypertension - also of the right. With ostium primum, there is a sharp deviation of the EOS to the left due to the displacement of the hypoplastic branch of the left leg of the His bundle forward. Various variants of sick sinus syndrome, AV block. With a defect such as sinus venosus - lower atrial rhythm or AV rhythm - junction.
• Jugular venography: equal amplitude of A and V waves.
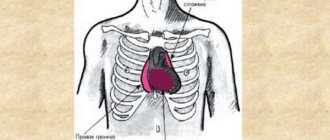
• X-ray examination of the chest organs. Strengthening the pulmonary pattern. Expansion and lack of structure of the roots of the lungs, bulging of the right atrium arch and upward displacement of the right cardiovasal angle. Fluoroscopy reveals increased pulsation of the roots of the lungs (a rather specific sign). The “Turkish saber” symptom with concomitant anomalous drainage of the right pulmonary veins into the superior vena cava.
• EchoCG. Hypertrophy and dilatation of the left sections, and with pulmonary hypertension - also of the right. Visualization of ASD in Doppler and B-mode. Differentiation from an open foramen ovale (the anatomical closure of the latter occurs no later than 2 years of life) is the inconsistency of visualization of the discharge in color Doppler mapping and the presence of a leaflet in the cavity of the left atrium. Diagnosis of associated anomalies (abnormal drainage of the pulmonary veins, valvular defects, etc.). The degree of discharge and the ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) are determined. Adults undergo transesophageal echocardiography. With intravenous contrasting of the right parts of the heart, there is a negative contrast effect (displacement of the contrast agent by a stream of blood from the left atrium).
• Radionuclide angiocardiography (first pass method or equilibrium): registration of pathological discharge and its quantitative assessment, diagnosis of concomitant abnormal drainage of the pulmonary veins and ventricular dysfunction.
• Probing of the cardiac cavities •• Indicated for suspected pulmonary hypertension, before open-heart surgery and with conflicting clinical data •• If the catheter can be passed from the right atrium to the left, then this in itself cannot be a sign of an atrial septal defect: sometimes the catheter it is possible to carry out through the open foramen ovale •• Tests are carried out with aminophylline and oxygen inhalation to determine the prognosis regarding the reversibility of pulmonary hypertension •• The ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) is calculated - a reference indicator of the amount of discharge.
• Right atriography, angiopulmonography: flow of contrast from the right atrium to the left; identification of concomitant abnormal pulmonary venous drainage.
Drug therapy. In uncomplicated ASDs of the ostium secundum type, infective endocarditis prophylaxis is usually not carried out. For ASDs of the ostium primum type, large defects of the sinus venosus type, and a combination of ASDs with mitral valve defects, antibiotics are prescribed before and for 6 months after uncomplicated surgical correction. For right ventricular failure, diuretics are prescribed.
Surgery
Indications: Qp/Qs ratio is 1.5 or more, defects of the ostium primum type, large defects of the ostium secundum type, concomitant hemodynamically significant anomalies (abnormal drainage of the pulmonary veins, mitral stenosis, etc.).
Contraindications: severe concomitant pathology that threatens the patient’s life; end-stage circulatory failure, irreversible pulmonary hypertension, the ratio of total pulmonary vascular resistance to peripheral vascular resistance is 0.9 or more.
Methods of surgical treatment. Endovascular correction with a button or two-patch Sideris device or an Amplatz device is feasible for central defects no larger than 2 cm in size. In the absence of experience in endovascular treatment, small defects are sutured under artificial circulation. In other cases, ASD repair with a synthetic or autopericardial patch under artificial circulation is recommended.
Specific postoperative complications • Sick sinus syndrome (after correction of sinus venosus type defects) • AV block (after correction of ostium primum type defects) • With mitral regurgitation that existed before surgery, symptoms may worsen after correction of ASD • Atrial fibrillation that occurred before surgery , as a rule, persists after it.
Forecast. In early childhood the course is benign. In rare cases, severe circulatory disorders can lead to death in the first months of life. Spontaneous closure of the defect is possible before the age of 5. The average life expectancy without treatment is 40 years. 5–15% of patients die before age 30. 10 - year survival rate - 90%, 20 - year - 88%, 30 - year - 67%; 40 years old - 44%, 50 years old - 25%, 60 years old - 13%, 70 years old - 7%. More than 75% of patients with large defects die from other causes. For uncomplicated defects of the ostium secundum type, perioperative mortality is less than 1%, it is slightly higher for defects of the ostium primum type, the latter also require mitral valve replacement or repair.
Aneurysm of the interatrial septum (ASA): causes, symptoms, diagnosis, treatment, prognosis
Have you been struggling with CHOLESTEROL for many years without success?
Head of the Institute: “You will be amazed at how easy it is to lower your cholesterol just by taking it every day.
Newborn babies can be diagnosed with a variety of congenital defects and abnormalities of the heart. Some of them are incompatible with life, others require surgical correction, otherwise severe hemodynamic disturbances cannot be avoided, others are relatively safe and are asymptomatic.
Aneurysm of the interatrial septum (interatrial septum) is classified as a so-called minor cardiac anomaly that does not cause significant circulatory disorders or changes in heart function. This is a rare defect of newborns, occurring in no more than 1% of cases and usually asymptomatic.
Our readers successfully use Aterol to lower cholesterol. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Young mothers who are faced with such an anomaly in their child should not panic - an aneurysm of the sac is not life-threatening, children develop correctly, and as the aneurysm grows, it may spontaneously disappear. Cases when an aneurysm is combined with a more serious defect, which will determine the symptoms and tactics of managing the baby, should cause concern.
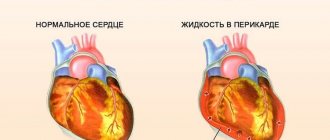
An MPP aneurysm can be isolated, but much more often it is combined with other heart defects and a patent foramen ovale, so the symptoms can be varied, but are not always associated specifically with the aneurysm. An ultrasound examination, which can be performed in the first days and weeks of life, allows one to suspect pathology in a newborn.
From an anatomical point of view, an aneurysm of the interatrial septum is a protrusion of the myocardial wall between the atria in one direction or another. Usually the wall prolapses in the area of the so-called fossa ovale, which remains after the oval window has healed, since the heart muscle there is not strong enough and can protrude under unfavorable conditions.
In the fetus, the pulmonary circulation does not function, because mastering the breathing process is possible only after the birth of the baby. Gas exchange in utero is maintained by a functioning placenta, and the foramen ovale, located in the septum between the atria, is necessary to redirect blood from the right atrium to the left and then the large circle. After birth, the hole closes almost immediately, the newborn breathes with his own lungs, and blood no longer flows from one atrium to the other.
Neonatologists often observe untimely closure of the oval window, which can function for quite a long time - up to a year or more. In such cases, the insufficiently strong myocardium has a greater chance of protruding in one direction or another under the influence of blood pressure. The combination of an aneurysm with a septal defect is more typical than an isolated septal aneurysm, although the latter option is also possible.
The causes of sac aneurysm have not been precisely established, and large-scale studies have not been conducted in this area. The role of both external and internal factors is assumed. This could be an infection suffered during pregnancy or unfavorable environmental conditions. The role of stress, lack of vitamins in the expectant mother, and intrauterine hypoxia cannot be ruled out.
Despite the lack of reliable data on the etiology of MPP aneurysm, most scientists still tend to agree that the development of connective tissue in the prenatal period is of key importance in the occurrence of the anomaly.
The connective tissue base of the heart may be immature, not strong enough, collagen fibers may be insufficient or their ratio may be changed. If these phenomena are not hereditary in nature, but are provoked by individual developmental characteristics, then, most likely, as the child grows, the heart will return to normal. With hereditary connective tissue dysplasia, the situation is much worse: three or more anomalies or more severe defects are found in the heart, and there are also signs of connective tissue dysplasia in other organs.
In preschool children with a functioning foramen ovale, a sudden aneurysm can be detected. After birth, such patients are diagnosed with a defect, but do not have an aneurysm. When the hole quickly becomes overgrown with fibromuscular tissue, the thin wall sag in one direction or another—an aneurysm of the cervical tract occurs.
In adults, atrial aneurysm can be a consequence of a large infarction, but this condition is extremely rare. Infarctions are more characteristic of the ventricular myocardium, while the atria are extremely rarely affected.
Conventionally, an aneurysm is considered to be a protrusion of the wall of the interatrial septum into one of the atria when, according to ultrasound data, it is more than 1 cm, but smaller protrusions will also be conditionally considered aneurysms.
Depending on the direction of deflection of the interatrial septum, three types of atrial septal aneurysms are distinguished:
- With bending into the right atrium (most common);
- Deflection into the left atrium;
- S-shaped aneurysm, when one part of the septum prolapses in one direction, and the other in the opposite direction.
general information
Short description
Approved by the Joint Commission on the Quality of Medical Services of the Ministry of Health of the Republic of Kazakhstan dated April 18, 2019 Protocol No. 62
An atrial septal defect is a communication (a hole in the atrial septum) between the left and right atria that allows pathological shunting of blood between these two chambers of the heart.
Protocol name: Atrial septal defect
ICD-10 code(s):
Date of protocol development/revision: 2013 (2020 revision)
Abbreviations used in the protocol:
Users of the protocol: cardiac surgeons, cardiologists, pediatric cardiologists, interventional cardiologists, neonatologists, pediatricians.
Patient category: children.
Level of evidence scale:
Diagnostics
DIAGNOSTIC METHODS, APPROACHES AND PROCEDURES
Diagnostic criteria
Complaints and medical history: may be asymptomatic, fatigue, symptoms of heart failure, shortness of breath during exercise, frequent respiratory diseases.
Physical examination: External examination: Increased right ventricular cardiac impulse. Auscultation: Constant splitting of the II tone in the II m.r. to the left of the sternum, regardless of the phases of breathing. Weak or moderate intensity systolic murmur of relative stenosis of the pulmonary valve in the second stage of birth. to the left of the sternum. A gentle mesodiastolic murmur of relative stenosis of the tricuspid valve along the left edge of the sternum in the lower third (with a significant left-to-right shunt).
Laboratory research:
- NT-proBNP: elevated natriuretic propeptide levels in the presence of symptoms of heart failure.
Instrumental studies:
- ECG: deviation of the electrical axis of the heart to the right, RV hypertrophy, complete or incomplete blockade of the right bundle branch - rsR' in lead V1.
- Plain radiography of the chest: dilatation of the right atrium and ventricle, dilatation of the pulmonary artery, increased pulmonary pattern.
- Echocardiography (transthoracic and transesophageal): Allows you to determine the location, size, edges of the defect, the size of the left-right shunt: interruption in the image of the interatrial septum, left-right (sometimes right-left) blood discharge during color Doppler examination, dilatation of the RV, sometimes the RA, various degree, dilatation of the pulmonary artery with normal or slightly enlarged right chambers of the heart, systolic pressure in the right ventricle is normal or slightly increased.
- Multislice CT angiography/MRI: according to indications for suspected anomalous pulmonary venous drainage or cardiac catheterization according to indications: for suspected anomalous pulmonary venous drainage or other associated cardiac anomalies.
Indications for consultation with specialists: The indication for consultation with specialists is the presence of concomitant pathologies of other organs and systems in the patient with the exception of the cardiovascular system in order to determine contraindications for surgical correction. Consultations can be carried out both in the pre- and postoperative period.
Diagnostic algorithm
List of main diagnostic measures during hospitalization (patient):
Laboratory research:
- testing for the causative agent of salmonellosis, dysentery, and typhoid fever;
- examination of stool for helminth eggs;
- throat swab for pathological flora;
- microreaction or Wasserman reaction (RW);
- HBsAg, antibodies to hepatitis B, C (ELISA);
- blood test for HIV;
- general urine analysis;
- general blood test (6 parameters);
- determination of total protein, glucose, creatinine, urea, ALT, AST, bilirubin - according to indications;
- TSH, T3, T4;
- With Down syndrome (trisomy 21).
Instrumental studies:
- X-ray of the chest organs in one projection;
- echocardiography;
- ECG.
Indications for consultation with specialists:
- consultation with a pediatric otolaryngologist to exclude foci of chronic infection;
- consultation with a pediatric dentist to exclude foci of chronic infection;
- consultation with a pediatric cardiologist to clarify the diagnosis and prescribe conservative therapy.
List of basic diagnostic measures during hospitalization (accompanying person): Laboratory tests:
- testing for the causative agent of salmonellosis, dysentery, and typhoid fever;
- examination of stool for helminth eggs;
- microreaction or Wasserman reaction (RW).
Instrumental studies:
- fluorography.
Basic diagnostic measures in the hospital: Laboratory tests:
- General urine analysis;
- General blood analysis;
- Biochemical blood test (determination of total protein, glucose, electrolytes, ALT, AST, C-reactive protein, urea, creatinine, bilirubin);
- Coagulogram (prothrombin time, fibrinogen, fibrinogen, INR, APTT, platelet aggregation);
- Determination of blood group and Rh factor;
- Microbiological examination (throat swab), sensitivity to antibiotics.
Instrumental studies:
- ECG;
- Echocardiography (transthoracic);
- Plain radiography of the chest organs.
Additional diagnostic measures:
Laboratory research:
Vps dmzhp mkb 10
Ventricular septal defect (VSD) is a congenital heart defect with communication between the right and left ventricles.
Pathogenesis
Variants of VSD • Membranous VSD (75%) are located in the upper part of the interventricular septum, under the aortic valve and the septal cusp of the tricuspid valve, often close spontaneously • Muscular VSD (10%) are located in the muscular part of the interventricular septum, at a considerable distance from the valves and conduction system , are multiple, fenestrated and often close spontaneously • Supracrestal (VSD of the outflow tract of the right ventricle, 5%) are located above the supraventricular crest, often accompanied by aortic insufficiency of the aortic valve, do not close spontaneously • Open AV canal (10%) is found in the posterior part of the interventricular septum, near the site of attachment of the rings of the mitral and tricuspid valves, often found in Down syndrome, combined with ASD of the ostium primum type and malformations of the leaflets and chords of the mitral and tricuspid valves, does not close spontaneously • Depending on the size of the VSD, small ones are distinguished (Tolochinov-Roget disease ) and large (more than 1 cm or half the diameter of the aortic orifice) defects.
Clinical picture
• Objectively • Pallor of the skin • Harrison's furrows • Increased apical impulse, trembling in the area of the left lower edge of the sternum • Pathological splitting of the second tone as a result of prolongation of the ejection period of the right ventricle • Rough pansystolic murmur at the left lower edge of the sternum • With supracrestal VSD - aortic diastolic murmur insufficiency.
Instrumental diagnostics
• ECG: signs of hypertrophy and overload of the left parts, and with pulmonary hypertension - also of the right.
• Jugular venography: high-amplitude A waves (atrial contraction with a rigid right ventricle) and, sometimes, V wave (tricuspid regurgitation).
• EchoCG • Hypertrophy and dilatation of the left parts, and in case of pulmonary hypertension - also of the right • Visualization of VSD in Doppler and B - mode • Diagnosis of associated anomalies (valvular defects, coarctation of the aorta, etc.) • Determine systolic pressure in the right ventricle, the degree of blood discharge and Qp/Qs • Transesophageal echocardiography is performed in adults.
• X-ray of the chest organs • With small VSDs - a normal x-ray picture • Bulging of the left ventricular arch, increased pulmonary vascular pattern • With pulmonary hypertension - bulging of the pulmonary artery arch, expansion and lack of structure of the roots of the lungs with a sharp narrowing of the distal branches and depletion of the pulmonary vascular pattern.
• Radionuclide ventriculography: see Atrial septal defect.
• Cardiac catheterization • Indicated when pulmonary hypertension is suspected, before open heart surgery and in case of conflicting clinical data • Calculate Qp/Qs • Carry out aminophylline and oxygen inhalation tests to determine prognosis regarding reversibility of pulmonary hypertension.
• Left ventriculography, coronary angiography: visualization and quantification of shunt, diagnosis of CAD in the presence of symptoms or before surgery.
Drug treatment. With an asymptomatic course and normal pressure in the pulmonary artery (even with large defects), conservative treatment is possible for up to 3–5 years of life.
If there is stagnation in the pulmonary circulation, use peripheral vasodilators (hydralazine or sodium nitroprusside), which reduce the discharge from left to right. For right ventricular failure - diuretics.
Before and for 6 months after uncomplicated surgical correction of VSD - prevention of infective endocarditis.
Contraindications:
Methods of surgical treatment. Palliative intervention - narrowing of the pulmonary trunk with a cuff, is performed when emergency surgery is necessary for children weighing less than 3 kg, with concomitant heart defects and little clinical experience in radical correction of the defect at an early age.
In case of a traumatic defect in the area of the membranous part of the interatrial septum, suturing of the defect is possible. In other cases, the defect is repaired with a patch made of autopericardium or synthetic materials.
In case of post-infarction VSD, plastic surgery of the defect is performed with simultaneous coronary bypass surgery.
Abbreviations
Did this article help you? Yes - 0 No - 1 If the article contains an error Click here 1383 Rating:
Source: https://kafros.ru/vps-dmzhp-mkb-10/
What kind of defect is this?
Atrial septal defect in children (ICD-10 code - Q21.1) is a congenital heart pathology in which a hole forms in the septum separating the atrial chambers. The disease occurs during the intrauterine formation of the baby’s organs. The parameters of the hole may be different, which determines the severity of clinical manifestations.
ASD has the following classification:
- Primary. Most often it is distinguished by the large size of the hole, which can reach 5 cm. It is located in the lower zone of the septum, the lower edge is completely absent. This form includes underdevelopment of the primary interatrial septum.
- Secondary. With this type of pathology, the secondary septum is affected. As a rule, a small hole is detected, not exceeding 2 cm. It is formed in the area of the mouth of the vena cava or in the middle of the septum.
- The absence of the partition itself. In the presence of such a disorder, they speak of the formation of a three-chambered heart, since the atria are connected and become one.
There is one pathological way of communication between the atria, which is called a patent oval window. This violation does not apply to ASD; it indicates insufficient development of the orifice valve. In this case, there are no hemodynamic disruptions, so surgical therapy is not performed.
Reasons for the development of pathology
Atrial septal defect in infants is a disease that is transmitted hereditarily. It occurs during intrauterine development of the fetus in the first months of pregnancy. It is during this period of gestation that the baby’s main organs are formed. Therefore, mothers are urged to be especially attentive to their health in the first trimester.
When exposed to unfavorable factors, the formation of the baby's heart may be disrupted. The atrial septum often undergoes pathological changes. The following phenomena can influence the development of the defect:
- Poor environmental conditions.
- Genetic predisposition.
- Viral diseases transmitted during pregnancy.
- Diabetes mellitus in an expectant mother.
- Uncontrolled use of medications by a pregnant woman.
- Maternal drinking and smoking.
- Irradiation of the body of a pregnant woman, the influence of various harmful substances on it.
- Severe toxicosis.
- The mother's age during pregnancy is over 35 years, and the father's age is over 45 years.
Forms of the disease
There are two types of aneurysm: congenital and acquired. The first option develops in childhood and is most often diagnosed in infants. Congenital appears after provoking events and can develop in different ways.
Congenital variant
It occurs in infants; doctors still do not know why the problem occurs. There are several options for the occurrence of the disease. Remember the following:
- Before the baby is born, there is a window in the septum through which blood flows from the right circulation to the left. This is necessary to ensure normal blood flow when the lungs are not yet working.
- After birth, when the baby takes his first breath, the right circle begins to work. The oval window begins to heal, this takes from several days to several weeks, and in its place a small mark remains in the form of a depression.
- Due to various violations and unfavorable factors, the overgrowing process is disrupted. The fabric has insufficient strength, which causes deformation over time.
- Sometimes an aneurysm of the interatrial septum in children is not associated with the oval window and forms in a different way. Most often this happens when blood flow is disrupted, and the deformation appears in a place where blood pressure on the tissue is increased.
The disease is provoked by one of four factors:
- Heredity. When a problem manifests itself in parents, the likelihood of it occurring in a child increases several times.
- Bad habits of father and mother. If you do not maintain a healthy lifestyle, the risk of disease will be much higher.
- Infectious diseases in the mother during pregnancy. Toxoplasmosis is especially dangerous in this regard.
- Unfavorable external conditions: poor ecology, large amounts of toxins in the air or food, ionizing radiation, etc.
Changes in the atrial septum occur against the background of systemic problems in the child’s body. Other organs also suffer, so doctors check the body completely. Cases of isolated aneurysm are quite rare.
Purchased option
In this case, the mechanism of the disease is always the same: the connective tissues are weakened, which causes a protrusion to form. This happens due to cardiovascular diseases: myocarditis, cardiomyopathy and myocardial infarction. The latter option is the most common cause of atrial septal aneurysm in adults. There are several types of disease:
- The acute variant appears within 2 weeks after myocardial infarction. It manifests itself as follows: a person’s condition worsens, the rhythm of cardiac activity is disrupted, and when tests are taken, the level of leukocytes is increased. In addition, people may feel feverish and their health often worsens.
- The subacute variant develops in 3-6 weeks. It develops when the formation of a scar at the site of dead myocarditis is disrupted, and a protrusion forms at this site. The malaise manifests itself gradually: people often experience shortness of breath, swelling of the lower extremities, and high fatigue.
- The chronic version manifests itself after a period of one and a half months or more. Signs of the disorder appear gradually, the nature and characteristics of the disease depend on the type and size of the aneurysm.
Advice! After suffering from the heart problems mentioned above, it is better to undergo an examination, even if the doctor did not prescribe it.
It is important for the doctor to determine the type of disease. This helps to predict the further development of the disease, determine characteristic symptoms and treatment that will be most effective.
Symptoms
Clinical signs of a septal defect begin to bother the patient most often by the age of 30. Despite the fact that the disease develops at the stage of intrauterine formation of the baby’s organs, after birth no symptoms are observed in children.
But there are a number of manifestations that may indirectly indicate heart problems, including ASD. These include:
- Rapid onset of fatigue.
- Weakness.
- Inactivity, refusal to play.
- Frequent development of viral diseases.
- Shortness of breath during physical activity.
These signs do not necessarily indicate the development of heart disease. But if you notice such manifestations in a child, you should consult a doctor and undergo an examination.
With age, the clinical picture becomes brighter, because the load on the heart increases. The development of an atrial septal defect can be suspected based on the following symptoms in adults:
- Difficulty breathing and shortness of breath that occurs even at rest.
- Attacks of dizziness.
- Loss of consciousness.
- Fatigue, weakness.
- Frequent occurrence of respiratory pathologies.
- Heart rhythm failure.
- Swelling of the lower extremities.
- Blueness of the skin.
These signs are more indicative of heart failure, which most often appears due to ASD if it is not treated promptly.
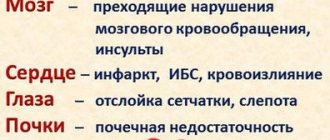
Possible complications
Atrial septal defect can cause serious complications if not treated promptly. After all, the heart is constantly under stress. As a result, it becomes depleted and various disturbances arise in it.
One common consequence is Eisenmenger syndrome. When it occurs, pulmonary hypertension occurs over a long period and is characterized by improper blood discharge. Another complication may be infectious endocarditis, which is an inflammatory process in the inner lining and valves of the heart. The development of this pathology is provoked by the penetration of infection.
Often patients are struck by a stroke. It occurs due to the fact that a blood clot or any other microembolus passes through a defective hole and blocks the vessels supplying the brain.
In addition to these diseases, ASD can lead to the following disorders:
- Failure of heart rhythm.
- Pulmonary hypertension.
- Ischemic heart disease.
- Rheumatism.
- Pneumonia.
- Acute heart failure.
- Disorders of the digestive organs.
The risk of death with an atrial septal defect is quite high if the pathology is not treated at all. With therapy, only half of patients live to be 50 years old, and many are considered disabled.
Possible consequences and complications
The atria are chambers with small volume and low shock force, so the presence of a protrusion in the wall between them rarely leads to hemodynamic disturbances. In the absence of blood discharge, the main consequence is damage to the conductive fibers. Complications :
- Atrial fibrillation (atrial fibrillation);
- Atrial flutter;
- Extrasystoles;
- Attack of tachycardia.
Complications in the presence of blood discharge:
- Chronic cardiopulmonary failure;
- Stagnation in the systemic circulation (edema, enlarged liver);
- Oxygen starvation of the brain, kidneys.
Complications are observed in 3-5% of patients.
Diagnostic measures
If signs of an atrial septal defect are detected, you should consult a physician. He will prescribe the necessary examination and, if heart problems are confirmed, refer you to a cardiologist who will begin treatment. It is impossible to detect pathology during a routine doctor's examination. Even when listening, no noise is observed.
Therefore, the patient needs to undergo a comprehensive heart examination. The following methods are used:
- Chest X-ray. Thanks to it, signs of heart failure arising from ASD are detected. The pictures clearly show that the right side of the heart is significantly increased in size. There is stagnation of blood in the lungs, so the artery is somewhat dilated.
- Ultrasound examination of the heart. With its help, the stage of development of the pathology, the direction of movement and the volume of blood that passes through the defect are determined. It is also possible to check the activity of the heart for failures.
- Electrocardiogram. An ECG allows you to diagnose disturbances in the functioning of the heart, which are characteristic of an interatrial defect.
- Magnetic resonance imaging. This method is not always used, but only if it is necessary to clarify the diagnosis or it was not made at all using ultrasound.
Secondary atrial septal defect in a newborn must be distinguished from other pathologies. The same signs can be present in diseases such as pulmonary artery stenosis, ventricular septal defect, and Fallot's triad.
If the atrial septal defect in a newborn is small, treatment may not be necessary. The patient is monitored. It often happens that the hole closes up on its own by about 1.5–2 years. When choosing observational tactics, a systematic visit to the doctor and an examination are required.
Conservative therapy
There are no medications in medicine that could help heal the defective hole. But medication is prescribed to stabilize the rhythm of the heart, eliminate symptoms, and improve the general condition of the patient.
The following medications can perform these tasks:
- Cardiac glycosides that help normalize blood pressure, heartbeat, and rhythm.
- Anticoagulants, which reduce blood clotting, prevent blood clots.
- Diuretics, which allow you to remove excess fluid from the body, stabilize blood pressure, and prevent swelling and blood stagnation.
- Inhibitors that help reduce the pathological size of the heart chambers and improve cardiac output.
- Only surgical intervention can completely eliminate the defect.
Endovascular method
Endovascular therapy is very popular in modern medicine. This method is characterized by increased safety, has virtually no contraindications, is quickly performed, and does not bring discomfort to the patient. The operation is intended to correct a septal defect.
To do this, large vessels are punctured, and a special device is installed through them to the area of the defect. Over time, it becomes covered with tissue, completely closing the opening of the ASD. Surgery is carried out under X-ray control.
After endovascular treatment, the patient becomes a completely healthy person. Rehabilitation takes place in a short time, no complications arise. This technique guarantees high efficiency and safety.
Open surgery
This operation is given the least preference, but is still performed in necessary cases. The intervention is performed under general anesthesia. The patient is connected to an artificial respiration apparatus. Then the chest is cut open, the heart is opened and the defect is repaired.
The pathological hole is simply sutured if it is less than 3 cm in size. If the defect is larger, then a special flap is sewn on. After the intervention, the patient remains in intensive care for a day, and then moves to the general ward, where he must be observed for 10 days. The prognosis after therapy is favorable.
Preventive measures
To prevent the baby from developing an atrial septal defect, a pregnant woman needs to register with a gynecologist as early as possible. During pregnancy, especially in the first trimester, you need to be careful about your health.
The expectant mother should not smoke, drink alcohol, strain excessively, or take medications uncontrollably or spontaneously. If relatives or the mother herself have a history of heart disease, this should be reported to the gynecologist who is managing the pregnancy.
Atrial septal defect (CHD) (congenital heart defect), which develops unnoticed over a long period of time. Therefore, you should be regularly examined by a cardiologist for timely detection of heart disease.
How to live with an atrial septal aneurysm?
The lifestyle of patients changes slightly. It is recommended to exclude physical overexertion, overeating and bad habits . There are no contraindications to physical labor and training according to the standard program.
It is recommended to reduce salt intake to 3 g per day and exclude from the daily diet:
- Transgenic fats;
- Products with dyes;
- Marinades;
- Butter pastries;
- Foods that affect the functioning of the heart (hot peppers, excessively hot food, ginger, spices).
Maintaining weight within age norms is the key to preventing complications.
Do they take you into the army? Do they give you disability?
Pathology is not a contraindication to military service. Disability is not registered.
Is it possible to play sports?
There are no contraindications to playing sports. The preferred types are swimming, race walking and gymnastics.
Will it affect pregnancy?
The presence of an aneurysm of the bladder does not affect the condition of the pregnant woman or the fetus and is not a contraindication to pregnancy if there are no associated defects.
Recommendations for parents of pediatric patients
Recommendations are preventive in nature:
- Register the child with a cardiologist;
- Regularly undergo medical examinations, including x-rays, ECG, consultations with a cardiologist, therapist, surgeon;
- Eliminate stress;
- Take multivitamins, magnesium and calcium supplements twice a year;
- Closely monitor the general condition of the child.
Atrial septal aneurysm is a rare cardiac anomaly. In most cases, the condition remains asymptomatic throughout life and does not require specific treatment. When making a diagnosis, patients are advised to adhere to general preventive measures and be attentive to their health.