What is Behçet's disease?
Behçet's syndrome or Behçet's disease is a condition that causes a range of symptoms , including:
- mouth ulcers;
- genital ulcers;
- inflammation of the eyes.
The disease is named after Professor Hulusi Behçet , a Turkish skin specialist (dermatologist) who first suggested that all these symptoms could be related to a single disease. It has since become clear that the syndrome can be associated with many other symptoms.
A syndrome is a group of symptoms (what a person experiences) and signs (what a doctor discovers when examining a person). Doctors tend to say syndrome rather than disease when the cause connecting the various symptoms is unknown to them.
Although many doctors now refer to Behcet's disease, others believe that it may not be a disease with a single cause. That's why we use the term "syndrome", but you will often hear the term "Behçet's disease".
When and which doctor to contact
Symptoms of the disease are varied and do not always appear at the same time, so they are not always associated with one disease.
To identify the disease, you need to make an appointment with a therapist.
At the first signs of an anomaly and damage to the mucous membranes, you should additionally consult a venereologist, infectious disease specialist, ophthalmologist, rheumatologist, or neurologist.
It is also necessary to conduct a complete examination of the entire body.
Symptoms of Behcet's syndrome
The disease has a wide range of possible symptoms, but most people only experience some of them.
Mouth ulcers
About 98% of people with Behçet syndrome have frequent mouth ulcers. They can occur in the mouth, tongue and throat and are often painful. Sometimes there are many tiny sores grouped together. If there are few sores in the mouth, it is very unlikely that the person has Behçet's disease, even if there is a relative who has the syndrome.
Genital ulcers
Women and girls may develop sores on the vulva, vagina, or cervix. Men and boys can get sores on the scrotum and penis. Some men and boys also experience pain or swelling in the testicles. Ulcers and boils may appear around the anus and in the groin.
The herpes virus does not cause mouth or genital ulcers in Behçet syndrome. They are not sexually transmitted and are not contagious, so you cannot get them from someone else.
Skin problems
Skin problems may include:
- spots that look like pimples;
- boils;
- red spots;
- ulcers;
- spots that look like insect bites;
- lumps under the skin.
The skin may become inflamed, ulcerated, or infected.
Eye inflammation
Inflammation in the eye is one of the most serious symptoms of Behcet's syndrome. The inflammation may be in the front or back of the eye, around the iris, or near the retina. Inflammations should be treated as soon as possible to avoid possible vision loss.
Symptoms may include:
- floating dots or specks in the field of view;
- blurred or loss of vision;
- pain;
- redness in the eyes.
Diagnostics
The doctor conducts a thorough history taking and examination. Differential diagnosis is carried out with the following pathologies:
- Other systemic rheumatic diseases (eg, systemic lupus erythematosus);
- Celiac disease.
- Exposure to drugs (methotrexate, nicorandil and others).
- Sexually transmitted diseases (herpes virus, HIV, gonorrhea, chlamydia, etc.).
To establish a diagnosis, a multidisciplinary assessment by a specialist is required.
What studies are carried out for Behçet's disease?
| Mandatory |
| Detailed blood test, urine test, liver function test, bone marrow puncture |
| Inflammatory markers including CRP and ESR |
| Chest X-ray |
| Stool analysis |
| Autoimmune examinations |
| Coagulation profile, antiphospholipid antibodies |
| Oral and genital swabs, cultures, sometimes an eye swab is needed |
| Other tests that may be required |
| Oral diseases – oral biopsy to rule out orofacial granulomatosis and bullous dermatosis (histology and direct immunofluorescence) |
| Diseases of the genital organs - vaginal biopsy to exclude other pathologies |
| Neurovascular Behçet's disease - Doppler studies, CT or MRI of the brain and spinal cord, MRV/CTV, MRA or CTA to evaluate neurological and vascular diseases. CSF, EEG, EMG, NCS, F PET fluorine-2-deoxyglucose studies with CT/MRI localization (for early inflammation in large vessel vasculitis) |
| Musculoskeletal – synovial fluid analysis, x-ray, ultrasound or MRI to evaluate joints |
| Skin lesions - skin biopsy and immunofluorescence |
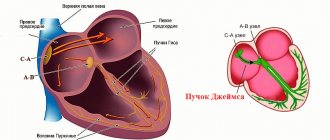
| Cardiac BD – electrocardiogram, echocardiogram |
| Chest CT – evaluates mediastinal disease, fibrous mediastinitis, aneurysms, pleural effusions, complications of venous thrombosis and collaterals |
| Gastrointestinal tract – stool sample for stool calprotectin, endoscopy and biopsy |
| Ear, nose and throat diseases – nasal endoscopy |
| Eyes – OCT, VEP, fluorescein angiogram, Schirmer test, intraocular fluid to rule out infections |
| Cystoscopy and CT scan of the bladder for urological diseases |
BD = Behçet's disease; CRP = C-reactive protein; CSF = cerebrospinal fluid; CT = computed tomography; CTA = computed tomographic angiography; CTV = computed tomographic venography; EEG = electroencephalogram; EMG = electromyography; ESR = erythrocyte sedimentation rate; MRA = magnetic resonance angiography; MRI = magnetic resonance imaging; MRV = magnetic resonance venography; NCS = nerve conduction study; OCT = optical coherence tomography; PET = positron emission tomography; VEP = visually evoked potentials
Causes of Behçet's syndrome
Behcet's syndrome is caused by inflammation, although it is not yet clear why this occurs. It is possible that a viral or bacterial infection may trigger the condition, but no specific infection has been identified. It is also possible that the disease could be an autoimmune disease, where the immune system attacks the body's own tissues, but this has also not yet been confirmed.
Behcet's syndrome cannot be passed on to other people. It is not associated with any other condition, any specific diet, or any specific lifestyle.
Risk factors
- Age . Behcet's disease most often develops in men and women between the ages of 20 and 30, although children and people in older age groups can also be susceptible to the disease.
- Region of residence . People from countries in the Middle and Far East, such as Turkey, Iran, Japan and China, are more likely to have this disease.
- Floor . The disease is usually more severe in men.
- Genes . Having certain genes is associated with a higher risk of developing the disease.
brief information
1.1 Definition
Behçet's disease (BD) is a chronic systemic vasculitis:
- with recurrent mucosal ulcers
- damage to the central nervous system
- damage to other organs.
1.2 Etiology and pathogenesis
Behçet's disease to a greater extent:
- typical Th-1-mediated inflammatory disease
- associated with an imbalance of innate immunity and activation of T-helper type 1 (Th-1)
- characterized by an increase in Th-1 cytokines - IFN-γ, IL-2, TNF-α, IL-1α, IL-1β, IL-6, IL-12, IL-13, IL-15
Development requires a combination of genetic predisposition and environmental factors:
- infections
- disorders of the microbiome of the oral cavity and gastrointestinal tract
- stress
- environmental pollution.
Evidence of genetic predisposition to BD:
- geographical distribution of the disease
- family aggregation
- positive correlation with HLA class I (HLA B5101)
- polymorphism of genes that control the immune response.
1.3 Epidemiology
The disease occurs in countries along the historical Great Silk Road.
Prevalence per 100 thousand:
- Türkiye 80-600 (mostly men)
- Iran and Iraq 70 (mostly men)
- Korea 35
- China 14
- Japan 11.9 (predominantly women)
- Russia 10 (natives of the North Caucasus)
- Europe 3.3 (predominantly women)
Debut between 20 and 39 years old.
Forecast:
- most often favorable
- in 25% of patients with eye damage without adequate therapy, a significant decrease in visual acuity
- mortality rate 9%, usually due to damage to the central nervous system and large vessels.
Risk factors for severe disease:
- debut under 25
- male gender.
1.4 Coding according to ICD 10
M35.2 - Behçet's disease
1.5 Classification
There is no special classification.
BB classification criteria ( ISGBD):
Recurrent oral ulcers
- Small or large aphthae, or herpetiform ulcers,
- Recur at least 3 times a year.
To diagnose Behçet's disease, there are 2 additional signs in addition to the above:
Recurrent genital ulcers; Eye damage:
- anterior, posterior uveitis and cells in the vitreous (in the slit lamp)
- retinal vasculitis (on examination)
Skin damage:
- Erythema nodosum (discovered by a doctor or self-reported by the patient)
- pseudofolliculitis and papulopustular rashes
- acne-like rash (in the postpubertal period without glucocorticoids (GC)
Positive pathergy test.
“Minor” criteria for the disease:
- Gastrointestinal lesions: ulcers in the ileocecal intestine
- Orchiepididymitis
- Arthritis without deformities and ankylosis
Clinical variants of Behçet's disease:
1. Complete type with 4 major features 2. Incomplete type:
- 3 big signs
- 2 large + 2 small signs
- typical eye symptoms with 1 major or 2 minor signs
3. Likely:
- only 2 big signs
- 1 large + 2 small signs
Classification characteristics:
International Consensus Classification of Neurological Disorders in Behçet's Disease (ICR)
Damage to the central nervous system
Parenchymatous
- Multifocal/ diffuse
- Brainstem lesion
- Spinal cord lesion
- Cerebellar lesion
- Asymptomatic (silent) lesion
- Optic neuropathy
Non-parenchymal
- Thrombosis of the cerebral venous sinuses: intracranial hypertension
- Cerebral artery aneurysms
- Aneurysms/dissection of extracranial arteries
- Acute meningeal syndrome
Damage to the peripheral nervous system (relationship with BD is uncertain)
- Peripheral neuropathy or multiple mononeuritis
- Myopathy or myositis
Mixed parenchymal and non-parenchymal lesions.
Definite neurological disorder with 3 criteria:
1. The patient meets the international criteria for BD (ISGBD) 2. Neurological syndromes are caused by BD and are confirmed by:
- neuroimaging
- cerebrospinal fluid (CSF) examination
3. There are no other causes for neurological manifestations other than BD
Probable neurological disorder if 1 criterion is present and there are no other causes of neurological impairment:
1. Neurological syndrome is characteristic of a significant neurological lesion, combined with systemic manifestations of BD, but the patient does not meet the international criteria for BD 2. Uncharacteristic neurological syndrome occurring in the context of international criteria for BD (ISGBD)
Assessment of overall BB activity using the BDCAF index proposed by ISBD.
Determination of the severity of BD according to the Zouboulis Ch classification. et al.
Low severity:
- aphthae of the oral mucosa
- genital ulcers
- typical skin lesions (erythema nodosum, papulopustular rashes, folliculitis, leukocytoclastic vasculitis)
- arthralgia
- recurrent headaches
- epididymitis
- minor gastrointestinal symptoms (chronic diarrhea, recurrent pain)
- pleural chest pain
- superficial venous thrombosis.
Moderate severity:
- arthritis
- deep vein thrombosis of the lower extremities
- anterior uveitis
- gastrointestinal bleeding.
Severe form:
- posterior uveitis, panuveitis, retinal vasculitis
- arterial thrombosis or aneurysm
- thrombosis of large veins (inferior vena cava, hepatic vein)
- neurological manifestations (hemiparesis, psychoemotional disorders, etc.)
- intestinal perforation.
Treatment of Behçet's disease
There is currently no cure for the disease. For mild cases of the disease, your rheumatologist may suggest ongoing use of medications to control flare-ups. In some cases, there is no need to take medications between flare-ups.
Treatments used:
- Creams, gels and ointments . Topical glucocorticoid medications are used for skin and genital rashes to reduce inflammation and pain.
- Mouth rinses . Special mouthwashes containing glucocorticoids and other agents that reduce mouth pain may also reduce discomfort.
- Eye drops . Eye drops containing glucocorticoids or other anti-inflammatory drugs eliminate signs of inflammation.
Systemic methods of treatment.
If topical medications don't help, your rheumatologist may recommend a drug called colchicine, which in addition to controlling the disease, also reduces signs of arthritis.
Severe cases of Behçet's disease require more aggressive treatment with the following medications:
- Glucocorticoids to control inflammation . Glucocorticoids, such as prednisolone, reduce inflammation. Side effects include weight gain, persistent heartburn, increased blood pressure, and decreased bone density (osteoporosis).
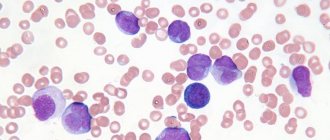
- Medicines that suppress the immune system (immunosuppressants) . Immunosuppressants reduce inflammation by stopping the immune system's aggressive response to healthy tissue. Immunosuppressive drugs that help control Behçet's disease include azathioprine, cyclosporine, and cyclophosphamide. Because these medications suppress the activity of the immune system, they increase the risk of infections in the patient. Other possible side effects include liver and kidney problems and effects on the hematopoietic system.
- Medicines that alter the immune system's response . Interferon-alpha (Intron A) regulates the activity of the immune system and the inflammatory response itself. It can be used alone or with other medications to help control skin conditions, joint pain, and eye inflammation. Side effects: flu-like conditions such as muscle pain, fatigue, fever.
- Medicines that block tumor necrosis factor (TNF) are effective in treating Behçet syndrome, especially in people with more severe or persistent symptoms. The world has accumulated experience in the use of infliximab and etanercept for this disease.
Etiology
The causes of Behçet's disease are not fully understood. There are several theories about the origin of the pathology:
- Hereditary - the disease is genetically determined. Cases of familial morbidity and hereditary continuity of the disease have been proven.
- Infectious - pathogenic biological agents play a certain role in the development of pathology. Herpes viruses and streptococci are the main infectious agents.
- Autoimmune - circulating immune complexes and antibodies to the body's own cells are found in the blood of patients.
Factors that provoke the formation of pathology include:
- Regular drinking of alcohol for 5 years,
- The presence in the body of foci of chronic infection - tonsillitis, sinusitis, otitis,
- Unreasonable use of medications,
- Uncontrolled vaccination and immunization,
- Insolation,
- Hypothermia,
- Physical overexertion,
- Stress.
Prognosis for Behçet's disease
Most people with Behçet's disease can lead productive lives and control symptoms with proper medications, rest, and exercise. Doctors may use many medications to relieve pain, treat symptoms, and prevent complications.
When treatment is effective, outbreaks usually become less frequent. Many patients eventually go into remission (disappearance of symptoms). For some people, treatment does not relieve symptoms and more severe symptoms, such as eye problems, gradually appear.
Severe symptoms may appear months or years after the first signs of Behçet's disease appear.
Sex and pregnancy
Genital ulcers associated with Behçet's disease can sometimes make sex uncomfortable or even painful. However, they are not sexually transmitted and are not contagious.
Some medications used to treat Behçet's syndrome can affect sperm, eggs, fertility or even the baby, for example thalidomide is known to be harmful to an unborn baby. It is important to discuss your plans with your doctor if you are thinking about having a baby. This applies to both men and women with Behçet's syndrome. However, there is no reason why you shouldn't have a family, and the chance of children inheriting the condition is slim.
Additional information affecting the course and outcome of the disease
- Information about the effect of pregnancy on BD is contradictory.
- The risk of pregnancy and childbirth complications is higher in women with BD and a history of thrombosis.
- There is evidence of exacerbation of BD in the 3rd trimester in women with painful genital ulcers.
- A number of studies have not noted the effect of BD on the outcome of gestation, and pregnancy on the course of BD.
Organization of medical care
Indications for hospitalization:
- High degree of BD activity with multiple organ lesions and/or resistance to therapy;
- Atypical course of BD;
- Severe comorbid diseases;
- The need to select and/or adjust the dose of GCs and immunosuppressants;
- The need for therapy with high doses of GC (pulse therapy) and immunosuppressants;
- Resolving the issue of prescribing/replacing a GIBP;
- The need for a course of complex treatment and rehabilitation in patients with decreased visual acuity and/or difficulty moving;
- Development of severe complications of BD and/or drug therapy.