In cardiology, there are groups of general terms that include a number of processes. They are equal in origin and similar in flow, but not completely identical. The prognosis and likelihood of cure usually vary. Depending on the severity of the disease, we can talk about one or another method of therapy.
Acute coronary syndrome is one of these conditions, but there is no such name in the ICD-10 classifier. If you understand the essence of the pathological process, it becomes clear what we are talking about.
The described condition is understood as a symptomatic complex, including chest pain, shortness of breath, rhythm disturbances and a number of other manifestations.
Clinical guidelines classify acute coronary syndrome as unstable angina or heart attack, depending on the severity of the symptoms.
Treatment takes place in a hospital. The third name for ACS is heart attack. Confusion in terminology leads to difficulties in understanding the essence of the process. In fact, it's the same thing. Diagnosis is not difficult, but you need to act extremely quickly. We're talking about an emergency.
Development mechanism
The essence of the pathological process is approximately the same, regardless of the type. As already mentioned, there are two types of the described situation: angina pectoris and heart attack. They are similar in nature.
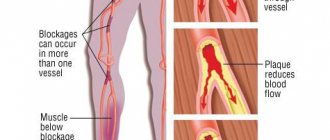
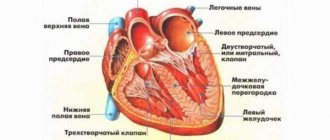
In both cases, there is a disruption in the nutrition of the muscular layer of the heart as a result of stenosis or occlusion (blockage) of the coronary arteries. Often this is a consequence of atherosclerotic changes, less often congenital or acquired defects.
As a result of a decrease in blood flow intensity, toxins accumulate in the organ structures, which inhibit normal myocardial contractility.
On the other hand, the muscle layer cannot work due to ischemia. Accordingly, the chambers of the heart are also unable to function adequately. The left ventricle does not eject blood into the systemic circle with sufficient force.
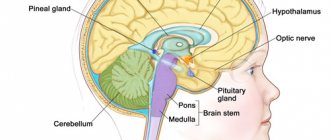
Hence the drop in oxygen saturation, poor supply to the brain, distant organs and systems.
This situation is not normal. Over time, death inevitably occurs. Recovery requires urgent action.
Classification
Typing is carried out according to a group of bases.
Based on the shape, they talk about two varieties:
- Unstable angina. Gradual, chronic malnutrition resulting from narrowing of the coronary arteries (much more common) or blockage.
Recovery requires long-term assistance. The pathological process itself is divided into 4 functional classes, they correspond to the severity of the disease.
The first is treated completely, starting with the second, it will no longer be possible to radically stop the condition. Lifelong therapy.
Unstable angina, a form of acute coronary syndrome, occurs in attacks, usually preceded by some trigger factor. From physical overexertion to hypothermia and others.
- Heart attack. In terms of severity, it is much more dangerous and characteristic. Accompanied by severe pain in the chest, impaired breathing and consciousness.
If angina pectoris develops slowly, stepwise, cardiomyocytes die in small groups, in this case the process is avalanche-like.
Destruction of large areas is possible. The wider the affected area, the more intense the symptoms.
After a certain time from the onset of this form of acute coronary syndrome, the phenomena subside.
Attention:
Imaginary prosperity should be perceived as an alarming sign, since destruction continues at a rapid pace.
The severity is partially affected by the clinical variant of the described condition:
- Primary form. Develops in patients who have not previously experienced angina attacks and have no history of heart attack.
- Progressive variety. Its essence lies in the aggravation of the main process. Usually the reason for this is a complication of the underlying disease, for example, atherosclerosis or an unhealthy lifestyle. Also lack of treatment or its insufficient effectiveness.
- Postoperative form. Accompanied by severe symptoms, but usually occurs over a short period of time. If the intervention is carried out incorrectly, a resistant variety may develop.
- Post-infarction type. Accompanies the rehabilitation period of an emergency condition. Requires mandatory correction, as it increases the risk of relapse.
- Spontaneous angina. The most dangerous from clinical point of view. Provokes frequent episodes of malnutrition in the short term. Up to 5-8 attacks can occur in a week.
ACS severity
Direct classification by severity involves taking into account electrocardiography indicators:
- ACS without ST segment elevation. Evidence in favor of a relatively mild clinical variant of the pathological process. Recovery is likely, the prognosis is relatively favorable. Usually corresponds to angina pectoris or a mild form of heart attack. Inpatient therapy in any case.
- Acute coronary syndrome with ST segment elevation. Accompanies severe organic heart damage. Corresponds to an extensive heart attack or a rapidly progressing process of destruction of cardiac structures. Recovery is strictly in the conditions of a specialized department. The prognosis is much worse and urgent medical attention is required.
Despite the difference between the two described forms in terms of results and outcome, the symptoms do not always correspond.
A patient with a potentially fatal variant of ACS may not feel significant changes in well-being, while minor angina can lead to intense pain and falsely lead a person to think about the severity of the condition.
Not only sensations, but also objective data are subject to evaluation.
Clinical forms of ACS and the degree of risk for the patient
There are two main forms of ACS:
- Unstable angina is chest pain characteristic of a heart attack, which appears for the first time or repeatedly, immediately after physical or emotional stress, or in a calm position.
- Myocardial infarction is death (necrosis) of the muscular wall of the heart. Depending on the area of the lesion, small-focal (microinfarction) and extensive are distinguished, according to localization - according to the accepted names of the walls of the heart - anterior, lateral, posterior diaphragmatic and interventricular septum. The main life-threatening complications are fatal arrhythmias and rupture of the heart wall.
Classification is important both for assessing the severity of the condition and for analyzing the level of risk of sudden coronary death (occurring no more than 6 hours from the onset of the attack).
High risk
presence of at least one of the following signs:
- An attack of angina for more than 20 minutes and to the present;
- Pulmonary edema (difficulty breathing, bubbling breathing, pinkish foamy sputum, forced sitting position);
- On the ECG: decrease or elevation of the ST segment more than 1 mm above the isoline;
- Angina pectoris with decreased pressure in the arteries;
- Laboratory: change in the level of markers of myocardial necrosis.
Medium risk
Discrepancy with high-risk items, or the presence of one of the mentioned signs:
- An attack of angina lasting less than 20 minutes, which stopped when taking nitroglycerin;
- Angina at rest for less than 20 minutes, which stopped after taking nitroglycerin;
- Nocturnal attacks of chest pain;
- Severe angina that first appeared within the last 14 days;
- Age over 65 years;
- On the ECG: dynamic changes in the T wave to normal, Q waves more than 3 mm, decreased ST segment at rest (in several leads).
Low risk
in case of discrepancy with the criteria for high and medium risk:
- More frequent and severe attacks than usual;
- Lower level of physical stress that causes an attack;
- Angina appeared for the first time, from 14 days to 2 months;
- On the ECG: a normal curve in accordance with age, or no new changes compared to previously obtained data.
Causes
The main factor in the development of acute coronary syndrome is atherosclerosis of the corresponding arteries supplying the heart. Depending on the type of deviation from the norm, there are two forms of the described condition.
- Stenosis. It is also a narrowing of blood supply structures. It is somewhat less common when compared with the second type of atherosclerosis. It often results from prolonged smoking, drinking alcohol, or improper treatment of the underlying vascular disease (no matter what). The lumen narrows, and conduction disturbance occurs. Blood cannot circulate normally. The heart increases its intensity to compensate for the resistance. Hence the increase in blood pressure and increase in heart rate. And since there is not enough nutrition, angina pectoris also occurs. The result is generalized dysfunction of the entire system. Treatment is strictly surgical, urgently.
- Occlusion. Blockage of a coronary artery by cholesterol plaque. Lipid structures are soluble in the early stages. Then they calcify and become hard as stone. Removal of such formations requires radical surgical measures.
Causes and risk factors of acute coronary syndrome
The main causes and risk factors are:
- Heredity : Having coronary heart disease in parents or siblings increases the risk of developing acute coronary syndrome.
- Gender: Men are more likely to have coronary heart disease, but only compared to women of childbearing age do estrogens have a protective effect against this disease; Postmenopausal women, on the other hand, have the same risk as men.
- Age : Acute coronary syndrome usually strikes after 45 years of age.
- Smoking : Among heavy smokers (more than 15 cigarettes per day) aged 45 to 54 years, the risk of death from coronary heart disease was estimated to be three times higher than among nonsmokers; this is due to both direct exposure to the smoke itself and a decrease in exercise tolerance.
- Arterial hypertension : definition of blood pressure equal to or greater than 140 mm Hg. maximum (systolic) pressure and 90 mm Hg. minimum (diastolic) pressure.
- Diabetes.
- Obesity: is a chronic disease characterized by one or more of the following parameters: body mass index - BMI = 30 kg/m² - body weight more than 30% of ideal weight - plyometric measurement values above 95° percentile. Central or abdominal obesity is associated with an increased risk of coronary heart disease.
- Hypercholesterolemia: specifically, high levels of low-density lipoprotein (LDL), low levels of high-density lipoprotein (HDL), and an LDL/HDL ratio >3.
- Hyperhomocysteinemia : Excessive presence of homocysteine in the blood (normal values: <13 µmol/L) is considered an important and independent risk factor for cardiovascular disease. It is promoted by poor nutrition: a diet rich in fat.
- Sedentary life : poor physical activity.
- A restless, nervous life.
Predisposing factors
But atherosclerosis does not arise out of nowhere. What factors predispose to the development of acute coronary syndrome:
- Alcohol consumption. The effect of the ethyl compound is pronounced and complex. Vascular stenosis occurs. And as the body gets used to ethanol, a disturbance in the metabolism of fats and their deposition occurs. Cholesterol levels are steadily increasing, and a mixed form of the described process is formed. At a certain point, giving up alcohol becomes not enough, and it is already difficult to stop drinking; there is a physiological need.
- Smoking. Provokes general vascular stenosis. Atherosclerosis, localized in the structures of the lower extremities, brain and heart, are just some of the options. They often occur in the system. Recovery involves giving up a bad habit. Some patients experience unfavorable results from the very first cigarettes. This characterizes the body's low resistance to harmful substances. A typical symptom of abnormal vascular function is a feeling of numbness in the legs and coldness in the fingers.
- Obesity. It is not the culprit of atherosclerosis and acute coronary syndrome, but a disorder of lipid metabolism. The problem lies deeper than it seems at first glance. Thromboembolism. Blockage of a coronary artery can occur not only with plaques, but also with blood clots. This is much more dangerous, since the process occurs in a matter of minutes; if the volume of occlusion is significant, death is inevitable. The blood flow stops at the level of one artery, and a large infarction begins. The prospects for recovery are zero.
- Vasculitis or vascular lesions. Autoimmune origin or, much less frequently, infectious-inflammatory. Therapy is long-term, sometimes lasting for years or a lifetime. There is a chance to transfer the process into a latent, sleeping phase, but a complete cure almost never occurs. The result is scarring and stenosis of the coronary arteries. The method of action in this case is surgical. It consists in restoring the patency of the vessel, and if plastic surgery is not possible, in prosthetics.
- Insufficient physical activity. Easy walks of an hour or two throughout the day are shown. You can do more, but you can’t overwork. This is fraught with another attack and a risk to health and life.
- History of diabetes mellitus.
- Arterial hypertension. It also significantly aggravates the course of acute coronary syndrome and the prognosis.
- Unfavorable heredity. Cardiovascular pathologies are genetically determined. If there was a patient in the family with similar diseases, there is a risk of repeating his clinical fate.
- Blood clotting disorders. The rheological properties of liquid connective tissue are normalized through the use of thrombolytics and antiplatelet agents, but in strictly controlled dosages.
Trigger factors
Factors that directly provoke an attack of acute coronary syndrome are:
- Intense stress, emotional shock. It causes a momentary narrowing of the arteries and manifests itself in different ways.
- Physical overload. For example, jogging, climbing to a floor without an elevator, carrying heavy objects without special equipment, and other options. Based on the nature of the provoking limit, we can talk about the severity of the process.
- Consumption of tobacco, coffee, alcohol, narcotic substances.
- Hypothermia.
The factors are easily identified. Many are subjective in nature and can therefore be eliminated by the patient himself. This is an important point, since activities are part of the prevention structure.
What is acute coronary syndrome?
Acute coronary syndrome (ACS) refers to a group of clinical manifestations defined by acute myocardial ischemia (coronary heart disease), that is, a sudden and critical decrease in blood flow to cardiac tissue.
The most common cause of this sudden drop in blood flow is rupture or erosion of a “vulnerable” coronary atherosclerotic plaque, followed by platelet accumulation and thrombotic occlusion with subsequent reduction or cessation of blood flow.
Symptoms
Depends on the form of acute coronary syndrome.
- Chest pain. Angina pectoris is characterized by the development of moderate discomfort. Moreover, its duration is no more than 30 minutes. Nitroglycerin, when taken, relieves the sensation well. During a heart attack, the pain is much stronger or lasts longer.
- Lack of oxygen. In complete peace. The patient cannot find a position for relief.
- Increased cold sweating.
- Paleness of the skin.
- Cyanosis of the nasolabial triangle as a calling card of cardiac pathologies in general.
- Panic attack. Accompanied by a strong feeling of fear, anxiety, continues throughout the first phase of the attack, then subsides. Treated with tranquilizers, preferably in a hospital setting. Doesn't always happen.
- Motor excitation. The patient cannot find a place for himself and rushes about.
- Confusion. The perception of reality is disrupted.
- Fainting or syncope. Indicate involvement of the brain in the pathological process.
The presented points form the basis of acute coronary syndrome.
The intensity of manifestations and the completeness of the clinical picture are never the same, but depend on the degree of circulatory impairment and the individual characteristics of the human body.
Types of pathology
The classification of ACS takes into account the degree of ischemia, the localization of the necrosis focus, the nature of the symptoms, the picture on the electrocardiogram and other signs. According to this principle, they are divided as follows:
- Acute myocardial infarction (MI) with the presence of a pathological Q wave. It is also called transmural or macrofocal. This type of cardiac circulatory disorder has the worst prognosis.
- Acute non-ST segment elevation myocardial infarction. This region is responsible for ventricular repolarization.
Acute MI without a pathological Q wave. Otherwise it is called small-focal. With it, a small area of necrosis occurs, uncritically disrupting the functioning of the heart.- Acute MI with ST segment elevation. Its presence indicates disturbances in the repolarization of the ventricles of the heart.
- Acute subendocardial MI. It affects the deep layers of the heart.
- Recurrent MI. This type of ACS manifests itself in the period from 3 to 28 days after the appearance of the first signs.
- Repeated MI. With it, the height of the clinical picture occurs after 28 days.
- Chronic coronary insufficiency, or unstable angina. It is called the "slow killer." This form of ACS rarely manifests itself clinically, but greatly depletes the patient's body.
First aid to the patient
It is aimed at stabilizing the patient’s condition, but not at radical treatment. Therefore, the main measure is to call an ambulance.
Everything else is actions aimed at preserving life and preventing the progression of destructive phenomena.
The correct procedure is:
- Measure blood pressure and heart rate. Activities are aimed at assessing objective indicators. Against the background of acute coronary syndrome, a drop in blood pressure and heart rate occurs. The opposite phenomenon is rarely observed.
- Next, a window or window is opened to provide ventilation to the room and partially compensate for oxygen starvation of the myocardium.
- The patient is seated, but cannot be laid down. Is it dangerous. Respiratory activity will be complicated, and blood flow in the myocardium may be further weakened.
- For medications, a Nitroglycerin tablet is given to relieve pain. Other drugs cannot be used.
Next, the person is carefully observed. Loss of consciousness is the basis for monitoring the quality of the heartbeat and the safety of gas exchange. This cannot be done at the prehospital stage.
The emergency care algorithm for acute coronary syndrome involves primary observation and exclusion of obvious risk factors. Unfortunately, there is little you can do on your own.
Reasons for the development of ACS
The mechanisms of development (pathogenesis) are the same for all ischemic, that is, associated with a lack of oxygen, heart diseases, including acute coronary syndrome. There are only two reasons that disrupt the normal movement of blood through the arteries: a change in the tone of the arteries and a decrease in their lumen.
1. Spasm of the vascular wall can occur from an increased release of adrenaline, for example in a stressful situation. The expression “the heart sank in the chest” accurately describes the state of a person with a short-term attack of ischemia. A short-term lack of oxygen is easily compensated for: the heart rate (HR) increases, blood flow increases, oxygen flow increases, well-being and mood become even better.
People who are passionate about extreme sports and recreation constantly receive short adrenaline “attacks” on the heart and associated pleasant sensations - joyful excitement, an influx of energy. A physiological bonus of any, even small, loads is a decrease in the sensitivity of the coronary vessels to spasm, and therefore the prevention of ischemia.
If the stressful situation is prolonged (the time varies depending on the “training” of the heart), then the decompensation phase begins. Muscle cells use up emergency energy reserves, the heart begins to beat slower and weaker, carbon dioxide accumulates and reduces the tone of the arteries, and blood flow in the coronary arteries slows down. Accordingly, the metabolism in the heart muscle is disrupted, part of it may become dead (necrosis). Foci of necrosis of the muscular wall of the heart are called myocardial infarction.
2. A decrease in the lumen of the coronary arteries is associated either with disturbances in the normal state of their inner lining, or with the blocking of blood flow by a thrombus (blood clot, atherosclerotic plaque). The frequency of the problem depends on risk factors, which, with prolonged exposure, lead to metabolic disorders and the formation of blood clots.
Main external factors:
- Smoking – general intoxication, disruption of the cells of the inner layer of arteries, increased risk of blood clots;
- Unbalanced diet – increased lipid levels in the blood; inadequate intake of proteins to the body’s needs; changing the balance of vitamins and microelements; metabolic imbalance;
- Low physical activity - “untrained” heart, decreased force of heart contractions, venous congestion, deterioration of oxygen supply to tissues, accumulation of carbon dioxide in them;
- Stress – constantly increased adrenaline levels, prolonged arterial spasm.
Agree, the name “external” is no coincidence; their level can be lowered or increased by the person himself, just by changing his lifestyle, habits and emotional attitude to what is happening.
Over time, the quantitative effect of risks accumulates and transforms into qualitative changes - diseases that are already considered internal risk factors for acute coronary insufficiency:
- Heredity - structural features of blood vessels, metabolic processes are also transmitted from parents, but as relative risk factors. That is, they can be either aggravated or significantly reduced by avoiding external factors.
- A persistent increase in lipids in the blood and atherosclerosis - deposits in the arteries in the form of atherosclerotic plaques with narrowing of the lumen, myocardial ischemia.
- Obesity - an increase in the total length of blood vessels, increased load on the heart, thickening of the muscle wall (myocardial hypertrophy).
- Arterial hypertension - consistently high blood pressure, changes in the walls of the arteries (sclerosation) with a decrease in their elasticity, congestive manifestations - edema
- Diabetes mellitus - blood viscosity increases and the risk of blood clots forms; changes in arterioles (the smallest arterial vessels) lead to ischemia of organs, including the myocardium.
The combination of several factors increases the likelihood of blood clots that completely block the heart’s own arteries. The consequence of developments in this scenario will be sudden coronary death , the second most common outcome (after myocardial infarction) of acute coronary syndrome.
Diagnostics
It is carried out under the supervision of a cardiologist. If the patient was transported to a hospital, there was minimal time for examination.
Limited to visual data and indicators of blood pressure and heart rate. Occasionally they resort to electrocardiography, but more often every minute counts.
The task is to first stabilize the patient, then engage in diagnostic research.
An approximate therapeutic regimen after restoration of body functions and relief of an attack:
- Oral questioning of the patient, collection of anamnesis.
- Measurement of blood pressure and heart rate. 24-hour Holter monitoring is much more effective. That is, recording indicators for 24 hours. It may be repeated.
- Electrocardiography. Assessment of functional activity of the heart.
- Echocardiography. Tissue visualization.
- General blood test, biochemical, hormones.
- Clinical examination of urine. First of all, we are interested in kidney function and the presence of sugar, as a sign of diabetes.
Unfortunately, most manifestations are smoothed out in bright moments. Only in case of relapse of coronary syndrome they are updated again.
Treatment
Conducted on an ongoing basis. There are three tasks: eliminate the etiological factor, relieve symptoms and prevent relapses. All issues are resolved simultaneously.
The basis of therapy is the use of medications:
- Statinov. To eliminate excess cholesterol and dissolve plaques. In the early stages of atherosclerosis, this is an effective measure. Atoris as a drug option.
- Antiplatelet agents. In order to prevent the formation of blood clots. This is a preventive and symptomatic measure that does not radically affect the situation. Aspirin-Cardio as the main name.
- Nitroglycerin for attacks.
- Mildronate and other supporting drugs that nourish cardiac structures and normalize metabolism.
Other funds are prescribed as needed.
Surgical techniques are required to eliminate congenital and acquired defects, coarse cholesterol deposits in advanced atherosclerosis.
There are several intervention options: excision of formations, ballooning/stenting (mechanical expansion of the lumen of the coronary artery) or prosthetics of the affected area.
Changing your lifestyle, giving up bad habits, adjusting your diet in accordance with table No. 10 and normalizing your physical activity regimen will help prevent relapses.
Treatment of acute coronary syndrome involves conservative tactics and less often surgical ones.
Prevention and recommendations
By adopting a healthy lifestyle, you can make a significant contribution to reducing certain risk factors associated with acute coronary syndromes and coronary heart disease. It is advisable to adhere to the following recommendations:
- quit smoking;
- limit alcohol consumption;
- Do moderate exercise regularly. To reduce the risk of cardiovascular disease, it is recommended to engage in moderate physical activity, such as walking, for at least 30 minutes a day, at least 5 days a week;
- weight loss and weight maintenance. The goal is to achieve a body mass index (BMI) of 18.5 - 24.9 kg/m²;
- Eat a healthy diet: Maintain your intake of fruits and vegetables, avoiding excessive consumption of red meat; in particular, limit the consumption of saturated fatty acids and introduce polyunsaturated fatty acids into the diet;
- keep stress under control.
Particular attention to prevention should be given to patients who are familiar with early coronary artery disease or suffer from diseases that may be associated with heart problems, such as hypertension, hyperlipidemia, diabetes mellitus.
It is important to follow the indications and pharmacological therapy suggested by your doctor to reduce the risk of serious complications.
Possible complications
Possible consequences include:
- Heart failure.
- Heart attack, primary or repeated. Each new one carries a great danger to life.
- Stroke. Poor circulation in brain structures with tissue necrosis.
- Cardiogenic shock. Blood pressure drops to critically low levels. Mortality is close to 100%.
Sudden death or at least disability without treatment is expected within a few years or less.
Prognostic assessments
The prognosis depends on the nature of the condition, lifestyle, age, gender (men can expect a slightly worse outcome), the presence of addictions, heredity, the nature of the treatment, concomitant pathologies, and type of professional activity.
The more negative factors, the worse the prognosis. Only a doctor can give specifics after a comprehensive assessment of all aspects and dynamics of the pathological process.
Attention:
Extremely unfavorable signs are fainting, especially frequent, the presence of heart failure, organic heart defects.
Acute coronary syndrome is a generic name for angina and heart attack. It is diagnosed accordingly, the code is determined according to the ICD. Prospects for cure are present for infarcts of minor severity and the initial stages of angina pectoris.