What it is
The disease was described in 1919 by Ernst Goodpasture as a case of glomerulonephritis associated with pulmonary hemorrhage during a worldwide influenza epidemic.
Alveolar basement membrane
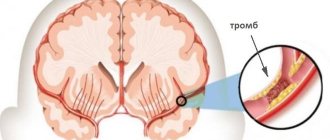
Goodpasture syndrome affects the alveoli of the lungs or the glomeruli of the kidneys. Alveoli are respiratory vesicles located in clusters at the ends of the smallest bronchioles. Their wall consists of one layer of epithelium in contact with air and one layer of endothelial cells lying on the wall of the blood capillary. Between these layers is a basement membrane, permeable to oxygen and carbon dioxide.
The renal glomerulus is the smallest functional unit of the kidneys. It is a network of convoluted capillaries enclosed in a glomerular capsule. The capillaries are lined with a layer of endothelium, and on the side of the capsule there are cells called podocytes. They are separated by a basement membrane, which allows water, salts, and some proteins to pass from the blood into the capsule. It continues below, separating the cells of the renal tubules, which remove primary urine, and the blood capillaries, where the bulk of the liquid from it is absorbed.
Glomerular basement membrane
Thus, the basement membrane is a “biological filter” that ensures the removal of carbon dioxide and metabolic products from the body and the supply of oxygen from the air and liquid with salts and proteins from primary urine. When it is damaged, these processes are disrupted.
With Goodpasture syndrome, antibodies are formed to the cells of the basement membrane - protective substances produced in the body. It acts against its own tissues, which is why this process is called autoimmune. The resulting antibodies and other immune components are deposited on the basement membrane, damaging it. As a result, glomerulonephritis is formed - inflammation of the renal glomeruli, and pulmonary hemorrhage also develops.
Normally, the vascular endothelium in the pulmonary capillaries is impermeable to the antibodies that are formed. Therefore, they reach the basement membrane of the alveoli only when vascular permeability increases. Therefore, for lung damage in Goodpasture syndrome, additional conditions are necessary:
- pulmonary hypertension;
- high oxygen content in the inhaled air;
- sepsis or the presence of toxins in the patient’s blood;
- exposure to vapors of hydrocarbon products (for example, gasoline);
- upper respiratory tract infections;
- smoking.
Autoimmune lesion of the glomerular basement membrane
Causes and risk factors
Goodpasture syndrome develops due to unknown causes. Environmental factors, such as chemical exposure to hydrocarbons, cigarette smoke, or infections such as influenza, may play a role in the development of the disorder. It is not known why simple infections can progress to anti-GBM disease in some people. When an infection occurs, the body's natural defenses (antibodies) fight off the invading organisms (such as viruses or bacteria). In autoimmune diseases, antibodies attack healthy tissue for no apparent reason. Pulmonary hemorrhage is often associated with smoking in individuals with Goodpasture syndrome.
In Goodpasture syndrome, certain antibodies (anti-glomerular membrane [anti-GBM] antibodies) may be produced and circulate in the blood. These antibodies can damage the thin membranes that line the lungs and kidneys or the tiny blood vessels (capillaries) in the lungs and kidneys.
In some cases, patients with Goodpasture syndrome may be associated with human leukocyte antigens (HLA). LACH are proteins that play an important role in the body's immune system; they influence the outcome of organ transplantation and appear to influence a person's susceptibility to certain diseases. However, the implications of such findings are not fully understood.
Anti-GBM disease has been reported in more than one family member (eg, siblings) in several cases, supporting the possibility of genetic susceptibility as a factor in some cases. A person who is genetically predisposed to a disorder carries the gene (or genes) for the disease, but it may not be expressed unless it is caused or "activated" under certain circumstances, such as due to certain environmental factors (multifactorial inheritance).
Causes
The cause of Goodpasture syndrome is unknown. Therefore, measures to prevent it have not been developed.
Some factors have been identified that may be related to the occurrence of the disease:
- viral infections, such as influenza A2c;
- prolonged contact with gasoline and organic solvents;
- smoking;
- shock wave lithotripsy (“crushing stones”) in the ureter for urolithiasis;
- genetic characteristics - the presence of certain genes of the HLA system in a person.
Development of the disease
Goodpasture syndrome is an autoimmune disease caused by the formation of antibodies to the body's own cells. Antibodies formed to the glomerular basement membrane participate in its development. They are aimed at binding to a certain (fourth) type of collagen, and to one of the sections of its molecule - the non-collagen domain of the 3rd chain.
The structure of type IV collagen
There are different types of collagen. The 4th type is a network of connected spirals, each of which consists of 3 threads. It is a specific fragment of such a biopolymer that pathological autoantibodies are aimed at. This fragment is called Goodpasture antigen, and does not cause any pathological reactions in healthy people.
Goodpasture antigen is present in large quantities in the renal glomeruli, alveoli, as well as in the walls of the capillaries of the retina, cochlea of the inner ear, and choroid plexuses of the brain.
Antibodies bind to the Goodpasture antigen, which causes activation of the complement system - special immune proteins. A cascade protein reaction consistently unfolds, as a result of which inflammatory cells - leukocytes - are attracted to the site of contact of antibodies with antigens.
Leukocytes infiltrate the affected tissues and destroy them. In response to a complex immune response, there is ultimately an increase in the number of epithelial cells that are deposited on the basement membrane in the form of microscopic crescents. As a result, kidney function is significantly impaired, and they cannot fully eliminate toxic products. The same reaction in the pulmonary vessels leads to their damage and blood entering the cavity of the alveoli.
Symptoms
At the onset of the disease, nonspecific symptoms of Goodpasture syndrome appear:
- malaise, unexplained weakness, fatigue;
- increased body temperature for no clear reason;
- pain in various joints without swelling or redness;
- weight loss.
Already at this stage, even in the absence of pulmonary bleeding, the patient develops anemia.
Nonspecific symptoms in Goodpasture syndrome are usually less pronounced than in other rheumatological diseases. Often the patient does not see a doctor, and the disease begins to progress rapidly.
In almost 70% of patients, the first symptom of the disease is hemoptysis. This is especially true for smokers. Now doctors are noticing a decrease in the frequency of this symptom, which may be due to a decrease in the prevalence of this bad habit.
In addition to hemoptysis, symptoms include shortness of breath and cough, and later pulmonary hemorrhage develops.
Pulmonary hemorrhage does not necessarily occur against the background of hemoptysis and does not depend on its severity. In many patients it develops suddenly and causes death within a few hours. This condition is accompanied by severe shortness of breath and bluish skin. It may be complicated by pulmonary edema or pneumonia.
A few months after the onset of the first pulmonary symptoms, a patient with Goodpasture syndrome develops rapidly progressive glomerulonephritis, which causes renal failure. This condition also often leads to death within the next two years.
The main symptoms of kidney damage:
- weakness, lack of appetite, pale skin;
- headache and lower back pain;
- various pains in the heart area;
- increased blood pressure;
- widespread swelling;
- blurred vision;
- decrease in urine volume.
These symptoms of Goodpasture syndrome fully manifest themselves within 4 to 6 weeks after their onset. Therefore, such glomerulonephritis is called rapidly progressive.
Signs and symptoms
The main symptoms of Goodpasture syndrome are excessive bleeding into the lungs (pulmonary hemorrhage) and inflammation of the filtering structures (glomeruli) or kidneys (glomerulonephritis). In some cases, an upper respiratory tract infection may precede the development of the disorder. Common symptoms associated with the syndrome may include:
- fever;
- nausea;
- fatigue.
Pulmonary hemorrhage can lead to episodes in which patients cough up blood (hemoptysis). The severity of this sign can range from a few spots to an excessive amount of blood. Those affected may also have difficulty breathing (shortness of breath), lethargy, chest pain, a dry, rough sound from the throat, and/or a frequent cough. In rare cases, those affected may experience an abnormal accumulation of fluid (edema) in the lung tissue. Pulmonary abnormalities are usually present before or simultaneously with renal abnormalities in about 70 percent of cases.
Inflammation of the filtering structures (glomeruli) of the kidneys (glomerulonephritis) can cause the kidneys to be unable to process waste from the blood and eliminate it in the urine (acute kidney failure). Kidney failure usually results in a decrease in the amount of urine the body produces. Additional symptoms associated with kidney failure may include:
- pale skin;
- drowsiness;
- nausea and/or vomiting.
Goodpasture's syndrome in children
Cases of Goodpasture syndrome in children are rarely reported. This disease is responsible for 0.4–1% of cases of severe renal failure in patients under 20 years of age. The average age of such patients is 17 years. The mortality rate from Goodpasture syndrome in children ranges from 0 to 3%, and their prognosis is better than in adults.
The incidence of girls and boys is approximately the same. But the disease does not only affect teenagers. The youngest known patient was 11 months old.
Only a few dozen cases of the disease are given in the literature. Goodpasture syndrome in children affects the kidneys and causes glomerulonephritis, which subsequently causes kidney failure. One of the early signs of the disease is the appearance of red blood cells in the urine. Therefore, it is important to regularly undergo preventive examinations and tests with your child. If you suspect kidney damage, you should be thoroughly examined by a nephrologist and, if necessary, agree to a biopsy of this organ.
Treatment is carried out in the same way as for adult patients.
Goodpasture syndrome: diagnosis
If Goodpasture syndrome is suspected, it is necessary to conduct an enzyme-linked immunosorbent assay (ELISA) of blood to determine antibodies to the glomerular basement membrane. In addition, all patients with rapidly progressive glomerulonephritis must undergo a kidney biopsy. During histological examination of biopsy material under a microscope, specific changes are determined, which, in combination with the detection of antibodies, make it possible to reliably make a diagnosis of Goodpasture syndrome.
Diagnosis of Goodpasture syndrome
Additional research:
- sputum analysis: siderophages are detected - cells that have absorbed red blood cells and the hemoglobin they contain;
- blood test: increased ESR, increased number of leukocytes, decreased concentration of hemoglobin and red blood cells;
- biochemical blood test: increased levels of creatinine, potassium and uric acid, impaired lipid metabolism;
- urine test: red blood cells and protein are detected;
- Reberg's test: decreased glomerular filtration rate.
Diagnosis of Goodpasture syndrome must be accompanied by the exclusion of other diseases. Their list is quite extensive. Therefore, if this disease is suspected, the patient should be referred to a rheumatologist as soon as possible, and also examined by a nephrologist and pulmonologist.
What diseases are used for differential diagnosis:
| Rheumatological diseases | Kidney pathology | Lung diseases |
|
|
|
An accurate diagnosis can only be made based on the results of a kidney biopsy; less commonly, a lung biopsy is performed.
Diagnostic measures
Diagnosis of pathology involves, first of all, collecting complaints and anamnesis of the patient’s illness and life. In identifying the syndrome, the initial examination plays an important role, and the results of laboratory tests are decisive. During the procedure, the doctor notes pallor of the skin, pastiness and swelling of the face. Wet and dry wheezing can be heard in the lungs, the number of which increases at the time of hemoptysis.
Laboratory methods
- Immunological studies of blood serum to detect BMK antibodies.
- Sputum analysis to identify siderophages and increased concentrations of hemosiderins.
- A general blood test to detect leukocytosis, pronounced acceleration of ESR, and iron deficiency anemia.
- General urine analysis to detect hematuria, proteinuria, cylindruria.
- Rehberg's test.
- Blood chemistry.
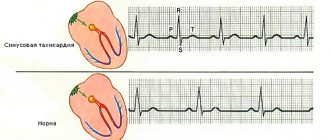
Instrumental methods
- tissue biopsy;
- immunofluorescence examination of biological material;
- X-ray of the lungs;
- sonography of the kidneys to determine their boundaries;
- CT scan of the chest;
- ECG and EchoCG;
- blood gas analysis;
- plethysmography;
- peak flowmetry to assess bronchial patency;
- pneumotachography;
- spirography.
Patients with rapidly progressive glomerulonephritis must undergo a biopsy of kidney tissue. Histological examination of the material makes it possible to determine specific changes that, in the presence of antibodies, make it possible to verify the development of pathology. During the examination, it is necessary to adhere to certain criteria. For Goodpasture syndrome, differential diagnosis is carried out to exclude the following diseases:
- tuberculosis;
- lung abscess;
- hemorrhagic diathesis;
- bronchiectasis with pneumosclerosis;
- uremic lung;
- periarteritis nodosa;
- Libman-Sachs disease;
- oncopathology of the lungs and kidneys;
- sarcoidosis;
- antiphospholipid syndrome;
- lymphoid granulomatosis;
- eosinophilic angiitis;
- rheumatic purpura;
- cryoglobulinemia;
- respiratory-renal form of nodular pernarteritis.
Goodpasture's syndrome should also be differentiated from systemic lupus erythematosus, hemorrhagic vasculitis, and Wegener's granulomatosis. These diseases are of an autoimmune nature and have a similar clinical picture. Diagnosis and treatment should be carried out jointly by several highly specialized specialists - therapist, rheumatologist, nephrologist, pulmonologist, endocrinologist.
Treatment
Without treatment, Goodpasture syndrome quickly leads to the death of the patient, mainly from renal failure, less often from pulmonary hemorrhage.
There are no dietary restrictions, except in cases of renal failure.
Almost all patients are prescribed complex therapy, which includes prednisolone, cyclophosphamide and plasmapheresis sessions. This treatment is aimed at removing autoantibodies and suppressing the inflammatory process in the kidneys. It is effective in 80% of patients.
Plasmapheresis is necessary to remove autoimmune components
If the level of creatinine in the blood exceeds 600 µmol/l, the effectiveness of treatment is significantly reduced, and in this case, therapy is supplemented with regular lifelong hemodialysis sessions. Without this, the prognosis of the disease is unfavorable.
Under the influence of therapy, antibodies to the basement membrane disappear within 1 - 1.5 years. The disease goes into remission. However, 2–10% of patients subsequently develop an exacerbation. It occurs within the first 10 years after recovery and is characterized by pulmonary hemorrhage or kidney damage. Treatment is carried out in the same way as at the onset of the disease.
After antibodies to the basement membrane are not detected in the blood for six months, a kidney transplant is considered. Relapse of the disease in the transplanted organ develops in 1-10% of cases.
Mortality during the first episode of the disease reaches 40%. The earlier treatment is started, the greater the patient’s chances of recovery. When the pathology recurs, the patient is already familiar with its symptoms, treatment begins earlier, and therefore the prognosis is better.
The average 5-year survival rate for this disease is 80%. Less than 30% of surviving patients require regular hemodialysis sessions. However, the average life expectancy is only about 6 years, and older age and pulmonary hemorrhage are factors that reduce it.
Thus, survival with Goodpasture syndrome depends almost entirely on the timing of diagnosis and initiation of therapy. The sooner a patient sees a doctor, the sooner he is in the hands of a specialist rheumatologist or nephrologist, undergoes a kidney biopsy procedure and begins full treatment, the greater the likelihood of recovery.
Diagnostics
Confirmation of the problem begins with a history and examination. The skin and mucous membranes of patients are pale, swelling is present on the limbs and face. Auscultation reveals moist rales in the lungs. Diagnosis of Goodpasture syndrome also requires blood and urine tests, which reveal changes characteristic of anemia, inflammatory lesions and impaired renal function. An X-ray, which allows you to take a photo of the lungs, is also important in confirming the disease. The images show multiple pathological lesions. This is due to the formation of peculiar cavities, as well as changes in the structure of the vascular pattern. An X-ray for Goodpasture syndrome, although not of key importance, helps to differentiate the problem from a number of others accompanied by similar symptoms.
Examination for this autoimmune disorder necessarily includes a specific test for the determination of antibodies to the basement membrane of the glomerular apparatus of the kidneys. Morphological analyzes are also used, which require sampling material using a biopsy. Ultrasound, echocardiography and ECG are used as additional methods.