General information
In simple words, heart block is a violation of the conduction of nerve impulses along the pathways.
The conduction system of the heart is represented by several structures:
- Sinus or sinoauricular node. It is a pacemaker; it is in it that impulses are generated that determine the heart rate. Located in the right atrium.
- Atrioventricular node. Transmits impulses from the pacemaker to the underlying structures.
- Bundle of His. Along the legs of this bundle, impulses pass into the right and left ventricles through the smallest structures - Purkinje fibers.
Causes of 1st degree AV block
These are mainly external factors. They can be eliminated by the patient himself, with rare exceptions.
- Intense physical activity, excessive activity. There is such a thing as a sports heart. Conduction disorders are the result of the development of cardiac structures. Such causes account for up to 10% of all clinical situations. But such a diagnosis can be made after long-term observation and exclusion of organic pathologies.
- Excess of medications. Cardiac glycosides, psychotropic drugs, calcium channel blockers, antispasmodics, muscle relaxants, narcotic analgesics, corticosteroids.
- Violation of the processes of inhibition of the nervous system. A relatively harmless factor. Usually it is part of a symptom complex of a disease.
Pathogenesis
The functioning of the cardiac conduction system depends on several factors:
- Blood supply to the myocardium. During ischemia, a shift in the acid-base balance occurs, which provokes a slowdown in neuromuscular conduction.
- State of the sympathetic and parasympathetic nervous system. The sympathetic transmitter Norepinephrine accelerates the conduction of impulses, and the parasympathetic transmitter Acetylcholine , on the contrary, slows it down.
- Hypo- and hyperkalemia .
- Hormonal background.
Under the influence of factors that change the intensity of the conduction system of the heart and with the development of pathological conditions, various disorders called heart blocks develop.
Classification
I Sinoauricular ( sinoatrial, CA ) block. A slowdown or complete cessation of the electrical impulse that comes from the sinus node through the sinoatrial connection is recorded. dizziness , sensations of interruptions in heart function , and fainting may occur .
II Interatrial (intraatrial) block. It manifests itself in a violation of the conduction of impulses along the conduction pathways in the atrium. It is asymptomatic. The ECG shows splitting and an increase in the duration of the P wave (more than 0.11 s). No specific therapy is provided.
III Atrioventricular, atrioventricular block. It is characterized by slowing down or stopping the conduction of impulses coming from the atria to the ventricles.
Degrees of heart block:
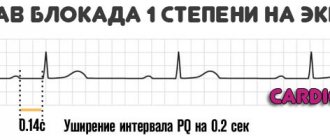
- 1st degree . It does not manifest itself clinically; it is characterized by a slowdown in the conduction of impulses from the atria to the ventricles, which is recorded on the ECG as a prolongation of the PQ interval by more than 0.2 seconds.
- 2nd degree . Divided into 2 types. Patients may experience pauses in the work of the heart in the form of darkening of the eyes and dizziness. With the loss of several ventricular complexes in a row, clinical symptoms increase. Mobitz I or proximal block. The ECG shows a gradual increase in the PQ interval with Samoilov-Wenckebach periods (loss of the ventricular complex). The QRS complex itself is not changed. Mobitz II or distal block. On the ECG, the QRS complexes appear randomly or regularly, the PQ interval is not prolonged.
- 3rd degree (complete heart block). There are no impulses to the ventricles. However, in the ventricles themselves, their own heterotopic focus of idioventricular rhythm is formed.
1st degree AV block does not require nonspecific treatment, but periodic examinations are recommended. For AV block II-Mobitz I, Atropine 0.6 mg is administered subcutaneously or intravenously 2-3 times a day. In case of complete AV block and AV block II-Mobitz II, implantation of a pacemaker is indicated.
IV Block of the branches of the His bundle ( Intraventricular block ). One, two or three branches may be affected, corresponding to mono-, bi- and trifascicular forms. Clinically, the His bundle block does not manifest itself in any way.
- Intraventricular blockade of the right bundle branch. Complete block of the right bundle branch - QRS complex more than 0.12 seconds, Incomplete block of the right bundle branch - less than 0.12 seconds. The consequences are minor. An incomplete blockade does not manifest itself symptomatically.
- Left bundle branch block. A complete block of the left bundle branch is characterized by a QRS expansion of more than 0.12 seconds, and an incomplete block of the left bundle branch is less than 0.12 seconds. Incomplete or partial blockade does not manifest itself symptomatically.
Local blockade of terminal branches (local, arborization, perifocal, nonspecific, focal). This subtype is often caused by an acute injury - myocardial infarction . Focal blockade is characterized by the presence of an acute “damage block” represented by necrotic cardiomyocytes. Necrosis prevents the passage of impulses along the pathways.
Treatment
Treatment of AV blockade consists of prescribing drugs to improve myocardial conduction and eliminate the underlying disease. In case of severe blockade, installation of an artificial pacemaker is required.
A first degree block does not require special treatment. Only observation of the patient and periodic Holter monitoring are indicated to determine the dynamics of the development of blockades.
In the second degree, the use of medications, for example, Corinfar, is indicated. The patient is also monitored.
A necrotic or fibrotic area of the myocardium can no longer be restored. In this case, first a course of beta-adrenergic agonists is administered, and then a pacemaker is implanted.
Causes
All causes of heart block are divided into several groups depending on the leading mechanism of their development.
Functional. Such blockades are caused by dysregulation and can be triggered by:
- neuroendocrine disorders;
- vegetative failures;
- psycho-emotional stress;
- maladaptive breakdowns.
The blockade can be caused reflexively by:
- cholelithiasis;
- gastritis;
- ulcerative lesions of the gastrointestinal tract;
- intervertebral hernia;
- pancreatitis;
- renal colic;
- neoplasms of the mediastinum;
- traumatic brain injuries;
- after surgical interventions.
Organic. These blockades are associated with myocardial damage due to ischemic heart disease, arterial hypertension , heart defects , and heart failure .
Toxic. Blockades are formed after poisoning with salts of heavy metals, narcotic substances, alcohol-containing drinks, as well as after an overdose of medications (cardiac glycosides, antibiotics , diuretics). This group also includes endogenous intoxication, which develops during infectious lesions and cancer.
Electrolyte shifts.
Changes in hormonal levels during pregnancy , hypothyroidism , thyrotoxicosis , puberty and menopause.
Congenital disorders in the structure of the cardiac conduction tract and impulse conduction (idiopathic calcinosis , ventricular preexcitation, short and short QT syndrome).
Mechanical . They occur after therapeutic and diagnostic manipulations on the heart, after injuries.
Idiopathic causes of heart block.
Causes of 2-3 degree blockade
Much more serious. Possible factors include:
- Myocarditis. Inflammatory pathology of the muscular layers of an organ of infectious or autoimmune (less commonly) origin. Occurs as a consequence in most cases.
Treatment in a hospital, the clinical picture is clear. A terrible complication - destruction of the ventricles is determined in every tenth case.
Especially without special antibacterial and supportive effects.
- Heart attack. Acute disturbance of trophism of cardiac structures. Occurs at any age, mainly in elderly patients. Also against the background of current ischemic heart disease, as a complication.
It ends with necrosis of cardiomyocytes (heart cells), replacement of active tissue with scar tissue. It is unable to contract and conduct a signal. Hence the AV block.
Depending on the extent, we can talk about the degree of severity. The more structures damaged, the more dangerous the consequences.
Complications of a major heart attack are described in this article, the symptoms of a pre-infarction condition are here, the causes and risk factors are here.
- Rheumatism. Autoimmune process affecting the myocardium. The treatment is long-term, lifelong maintenance therapy is the result.
It is possible to slow down the destruction and prevent relapses, but complete relief is unlikely.
The neglected phenomenon ends with damage to the His bundles and conduction disturbances.
- Ischemic disease. It is similar in nature to a heart attack, but the process does not reach a certain critical mass, since the blood supply still remains at an acceptable level. However, necrosis of the muscle layer will not take long to occur without treatment. This is the logical conclusion of IHD.
- Coronary insufficiency. As a result of atherosclerosis with narrowing or occlusion of the corresponding arteries supplying cardiac structures. Manifestations occur in later stages. Blockade is one of the organic disorders. Read more about coronary insufficiency here.
- Cardiomyopathy. The generic name of a group of processes. Arises as a consequence of severe somatic pathologies.
The essence lies in dystrophy of the muscular layer of the heart. Contractility decreases, the signal is transmitted through damaged tissues worse than in the normal position.
Weakened hemodynamics, ischemia, multiple organ failure as a consequence. Types of cardiomyopathy, causes and treatments are described in this article.
The presence of pathologies of the adrenal glands of the deficient type, the thyroid gland, and blood vessels, including the aorta, also affects.
The list goes on. There is an opinion about the participation of a hereditary factor in the process. Whether this is true or not is not entirely clear. In recent years, the role of the genetic component has been actively studied.
Symptoms of heart block
The main signs indicating a violation of cardiac conduction:
- a feeling of interruptions in the work of the heart;
- feeling of “fading”, cardiac arrest;
- periodic fainting states;
- slow heartbeat;
- pallor and cyanosis of the skin;
- attacks of chest pain.
Symptoms of complete heart block
Clinically, it manifests itself as an increase in the severity of heart failure during physical activity, which is associated with a low pulse. Incomplete heart block upon transition to complete is characterized by:
- loss of consciousness;
- severe shortness of breath;
- inability to determine the pulse;
- convulsions;
- absence of heart sounds;
- involuntary urination, defecation.
The attack can end in 1-2 minutes with the appearance of idioventricular rhythm. If the blockade lasts 3-4 minutes, then the patient’s death occurs.
Diagnostics, ECG for heart block
SA blockade
The ECG records the loss of individual cardiac complexes (QRS and P waves), while the pause between two adjacent RR waves doubles compared to the usual interval. Atropine is administered subcutaneously or intravenously at 0.6-2.0 mg 2-3 times a day. It is possible to use Isoprenaline 2.5-5.0 mg up to 3-4 times a day.
Complete AV block
- uniform alternation of atrial complexes;
- P waves are not related to QRS complexes in any way;
- P waves may overlap the ventricular QRS;
- the ventricular rhythm is correct.
Right bundle branch block on ECG
- QRS complexes are M-shaped as RsR in leads V1 and V2;
- there is depression of the ST segment in the right precordial leads;
- the T wave is biphasic or negative;
- the S wave is widened and jagged in leads I, aVL, V5 and V6;
- the electrical axis is deflected to the right (variable).
Left bundle branch block
- QRS complexes are presented as RsR or the apex of the R wave is widened and split. Complete left intraventricular block - QRS greater than 0.12 s.
- There is ST segment depression in the left precordial leads.
- The T wave is negative or biphasic.
- The ventricular complexes are widened, deformed and presented as rS, QS in leads V1, V2, III and aVF.
- Deviation of the electrical axis to the left.
Diagnostics
The loss of some impulses becomes more obvious in the advanced stages of the blockade. To determine the causative factor, you will need to go to the clinic at your place of residence and make an appointment with a cardiologist. He will conduct a survey to find out disturbing symptoms, the presence of hereditary predisposition and concomitant pathologies, and then examine the patient. Having made certain conclusions for himself, the doctor will refer the patient for examination. The main diagnostic method is electrocardiography (ECG). To identify a blockade, the following manipulations are usually performed:
- The patient is given a dose of Atropine. Conduction disturbances not associated with pathological changes begin to appear after approximately 30 minutes.
- On an electrocardiogram, the doctor will see altered waves that demonstrate how slowly the impulses are moving.
Additionally, you may need to undergo daily ECG monitoring, ultrasound of the heart and tests. Based on the results obtained, the doctor will be able to make a diagnosis and draw up a treatment plan.