Aortic valve regurgitation is the backflow of blood from the aorta into the left ventricle. This pathology occurs due to incomplete closure of the aortic valve. Most often, this pathology is observed in men over 60 years of age.
For aortic regurgitation, treatment can be medication or surgery.
General information
Regurgitation refers to the reverse flow of blood from one chamber of the heart to another. The term is widely used in cardiology, therapy, pediatrics and functional diagnostics. Regurgitation is not an independent disease and is always accompanied by an underlying pathology. The reverse flow of liquid into the original chamber can be caused by various provoking factors. When the heart muscle contracts, there is a pathological return of blood. The term is used to describe disorders in all 4 chambers of the heart. Based on the volume of blood that comes back, the degree of deviation is determined.
Diagnostics
Cardiologists examine patients with problems of this kind. If the process is advanced, a consultation with a specialized surgeon is indicated.
Approximate scheme of events:
- Questioning the patient about health complaints. It can be carried out using a standard questionnaire, this will speed up the work of doctors.
- Anamnesis collection. Lifestyle, family history, somatic diseases and other processes are subject to mandatory recording. This ensures the determination of the vector for further diagnostics.
- Listening to heart sounds. The first tone is dull, the second is split, and a sinus (systolic) noise is also observed, caused by reverse blood flow.
- Verification of the diagnosis is carried out by echocardiography. Since this imaging technique is aimed at detecting cardiac defects, there are not many alternatives.
- Electrocardiography. Allows to identify functional disorders of cardiac structures. Requires great qualifications from doctors, since errors are possible.
- Daily monitoring. Necessary for studying abnormalities in the cardiovascular system as a whole. Indicated in an outpatient setting; the hospital does not have the opportunity to create a natural environment.
- Blood pressure measurement. The cause of the acquired defect in some cases is hypertension.
- MRI. For greater detail of cardiac structures.
Laboratory techniques are not used due to ineffectiveness. Consultation with an endocrinologist will be required. This is a rare occurrence; treatment is carried out against the background of suspected diabetes mellitus.
Pathogenesis
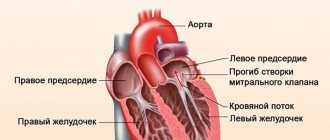
The heart is a muscular, hollow organ consisting of 4 chambers: 2 atria and 2 ventricles. The right and left parts of the heart are separated by a septum. Blood enters the ventricles from the atria, and is then pushed out through the vessels: from the right sections - into the pulmonary artery and pulmonary circulation, from the left sections - into the aorta and systemic circulation.
The structure of the heart includes 4 valves that determine the flow of blood. The tricuspid valve is located in the right half of the heart between the ventricle and the atrium the mitral is located in the left half . The pulmonary valve and are located on the vessels leaving the ventricles .
Normally, the valve flaps regulate the direction of blood flow, close and prevent reverse flow. When the shape of the valves, their structure, elasticity, and mobility change, the complete closure of the valve ring is disrupted, and some of the blood is thrown back and regurgitates.
Mitral regurgitation
Mitral regurgitation occurs as a result of functional valve insufficiency. When the ventricle contracts, part of the blood flows back into the left atrium. At the same time, blood flows there through the pulmonary veins. All this leads to overfilling of the atrium and stretching of its walls. During the subsequent contraction, the ventricle ejects a larger volume of blood and thereby overloads the remaining cavities of the heart. Initially, the muscular organ reacts to overload with hypertrophy , and then with atrophy and stretching - dilatation . To compensate for the loss of pressure, the vessels are forced to narrow, thereby increasing peripheral resistance to blood flow. But this mechanism only aggravates the situation, because regurgitation intensifies and right ventricular failure . At the initial stages, the patient may not make any complaints and not feel any changes in his body due to the compensatory mechanism, namely, a change in the configuration of the heart, its shape.
Mitral valve regurgitation can develop due to calcium and cholesterol on the coronary arteries, due to dysfunction of the valves, heart disease, autoimmune processes, changes in metabolism , and ischemia of certain areas of the body. Mitral regurgitation manifests itself differently depending on the degree. Minimal mitral regurgitation may not manifest itself clinically.
What is grade 1 mitral regurgitation? The diagnosis is established if the backflow of blood into the left atrium extends to 2 cm. Stage 2 is said if the pathological flow of blood in the opposite direction reaches almost half of the left atrium. Grade 3 is characterized by reflux beyond half of the left atrium. At grade 4, the flow of reverse blood reaches the left atrial appendage and can even enter the pulmonary vein.
Aortic regurgitation
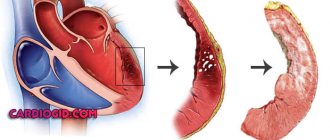
When the aortic valves fail, part of the blood returns during diastole back to the left ventricle. The large circulation suffers from this , since a smaller volume of blood enters it. The first compensatory mechanism is hypertrophy, the walls of the ventricle thicken.
Muscle mass, which has increased in volume, requires more nutrition and oxygen flow. The coronary arteries cannot cope with this task and the tissues begin to starve, hypoxia . Gradually, the muscle layer is replaced by connective tissue, which is unable to perform all the functions of the muscular organ. Cardiosclerosis develops , heart failure progresses.
As the aortic annulus expands, the valve also enlarges, which ultimately leads to the fact that the aortic valve leaflets cannot fully close and close the valve. There is a reverse flow of blood into the ventricle, when it is refilled, the walls stretch and a lot of blood begins to flow into the cavity, and little into the aorta. Compensatoryly, the heart begins to contract more often, all this leads to oxygen starvation and hypoxia , stagnation of blood in large-caliber vessels.
Aortic regurgitation is classified by degree:
- 1st degree: reverse blood flow does not extend beyond the boundaries of the outflow tract of the left ventricle;
- 2 degrees: the blood stream reaches the anterior leaflet of the mitral valve;
- 3 degrees: the jet reaches the boundaries of the papillary muscles;
- 4 degrees: reaches the wall of the left ventricle.
Tricuspid regurgitation
Tricuspid valve insufficiency is most often secondary in nature and is associated with pathological changes in the left parts of the heart. The mechanism of development is associated with an increase in pressure in the pulmonary circulation, which creates an obstacle to sufficient release of blood into the pulmonary artery from the right ventricle. Regurgitation may develop due to primary tricuspid valve incompetence. Occurs when pressure in the pulmonary circulation increases.
Tricuspid regurgitation can lead to emptying of the right side of the heart and congestion in the venous system of the systemic circulation. Externally it manifests itself as swelling of the neck veins and bluish discoloration of the skin. Atrial fibrillation may develop , and the liver may increase in size. Also classified by degree:
- Tricuspid valve regurgitation grade 1. Tricuspid regurgitation of the 1st degree is a minor reflux of blood that does not manifest itself clinically and does not affect the general well-being of the patient.
- Tricuspid valve regurgitation of the 2nd degree is characterized by the reflux of blood at a distance of 2 cm or less from the valve itself.
- Grade 3 is characterized by throwing more than 2 cm from the tricuspid valve.
- At grade 4, the reflux of blood spreads over a long distance.
Pulmonary regurgitation
If the pulmonary valves do not close properly during diastole, the blood partially returns to the right ventricle. At first, only the ventricle is overloaded due to excessive blood flow, then the load increases on the right atrium. Signs of heart failure gradually increase, and venous congestion .
Pulmonary artery regurgitation or pulmonary regurgitation is observed with endocarditis , atherosclerosis , syphilis , and maybe congenital. Most often, diseases of the pulmonary system are simultaneously recorded. Blood reflux occurs due to incomplete closure of the valve in the artery of the pulmonary circulation.
Pulmonary regurgitation is classified by degree:
- Pulmonary regurgitation grade 1. It does not manifest itself clinically; upon examination, a slight backflow of blood is detected. Grade 1 regurgitation does not require specific treatment.
- Pulmonary regurgitation of the 2nd degree is characterized by the reflux of blood up to 2 cm from the valve.
- Grade 3 is characterized by a throw of 2 cm or more.
- At grade 4, there is a significant reflux of blood.
Degrees and forms of aortic regurgitation
This pathology is divided into 4 degrees depending on the volume of blood flow:
- at grade 1, the flow does not extend beyond the outflow tract of the left ventricle;
- with the 2nd flow extends to the anterior mitral leaflet;
- with the 3rd flow it reaches the level of the papillary muscles;
- at the 4th, the blood flow reaches the wall of the left ventricle.
The cause of aortic regurgitation is aortic valve insufficiency, which has. Pathology has two forms: chronic and acute. In the chronic form, over time, the coronary arteries are affected, the contractility of the left ventricle decreases, its dysfunction develops, and its volume increases. All this leads to the development of serious and extremely dangerous complications that can lead to death.
In the acute form, hemodynamics are very quickly disrupted, so the patient requires immediate medical attention. Otherwise, there is a high risk of developing cardiogenic shock.
Classification
Classification of regurgitation depending on location:
- mitral;
- aortic;
- tricupidal;
- pulmonary
Classification of regurgitation by degree:
- I degree. The disease may not manifest itself in any way for several years. Due to the constant reflux of blood, the cavity of the heart increases, which leads to an increase in blood pressure. During auscultation, you can hear a heart murmur, and when performing an ultrasound of the heart, divergence of the valve leaflets and impaired blood flow are diagnosed.
- II degree. The volume of returning blood flow increases, and blood stagnation in the pulmonary circulation is observed.
- III degree. A pronounced reverse jet is characteristic, the flow from which can reach the posterior wall of the atrium. The pressure in the pulmonary artery increases, the right side of the heart is overloaded.
- The changes concern the systemic circulation. Patients complain of severe shortness of breath, chest pain, swelling, rhythm disturbances, and bluish skin.
The severity of the stage is assessed by the power of the jet that returns to the heart cavity:
- the jet does not extend beyond the boundaries of the anterior valve leaflet, which connects the left ventricle and the atrium;
- the jet reaches the border of the valve leaf or crosses it;
- the stream reaches half of the ventricle;
- the stream touches the top.
How does tricuspid valve regurgitation occur?
The tricuspid or tricuspid valve is located between the right atrium and the right ventricle; during diastole, its valves open, allowing venous blood to pass from the right atrium into the ventricle. During systole (contraction), the valve leaflets close tightly, and the blood entering the right ventricle enters the pulmonary artery and then into the lungs. When the tricuspid valve regurgitates, the blood from the right ventricle does not completely enter the pulmonary artery, but partially returns to the right atrium, and a reverse reflux of blood occurs - regurgitation. This occurs due to dysfunction of the tricuspid valve - when its valves do not close tightly, the entrance to the right atrium does not completely close. With tricuspid regurgitation, due to increased load, the atrium hypertrophies, and then the muscles stretch and increase in size. In turn, this leads to the entry of a large amount of blood from the atrium into the right ventricle during diastole, its further hypertrophy and dysfunction, which provokes stagnation in the systemic circulation.
Causes
Valve dysfunction and regurgitation can develop as a result of inflammation, trauma, degenerative changes and structural abnormalities. Congenital incompetence occurs as a result of intrauterine developmental defects and may be due to heredity.
Reasons that can lead to regurgitation:
- infective endocarditis;
- systemic autoimmune disease;
- infective endocarditis;
- chest injury;
- calcification;
- valve prolapse;
- myocardial infarction with damage to the papillary muscles.
Causes of tricuspid regurgitation
Let's look at the main reasons that lead to the development of the disease. The following factors are important for the occurrence of primary forms:
- Tricuspid valve prolapse. This defect is associated with pathological protrusion of one or more leaflets.
- Endocarditis. An inflammatory disease of the heart tissue that develops against the background of an infection.
- All rheumatic diseases causing fibrosis of the valve apparatus.
- Infarction localized to the right.
- Carcinoid syndrome, in which connective tissue plaques can be deposited in the blood vessels and heart. The syndrome is caused by excess serotonin in the blood.
- Ebstein's anomaly, a rare birth defect in which the atrioventricular valve is located abnormally in the wall of the right ventricle.
- Marfan syndrome, a genetic pathology that is accompanied by aneurysm and heart failure.
- Long-term use of certain medications.
- Consequences of traumatic injuries to the chest.
The causes of the secondary type of regurgitation are the following diseases:
- Cardiomyopathy is a disease associated with structural changes in the myocardium.
- Hypertrophy (thickening, enlargement) or expansion (dilatation) of the ventricle on the right.
- Pulmonary hypertension is an increase in internal pressure in the pulmonary vessels.
- Other pulmonary artery defects (obstruction).
- Mitral stenosis.
- Combined failure of both ventricles.
- Congenital defects of the atrial septum.
Symptoms
With mitral regurgitation in the subcompensation stage, patients complain of a feeling of rapid heartbeat, shortness of breath during physical activity, cough, chest pain of a pressing nature, and excessive fatigue. As heart failure increases, acrocyanosis , swelling, rhythm disturbances, and hepatomegaly (increase in liver size) occur.
With aortic regurgitation, a characteristic clinical symptom is angina , which develops as a result of impaired coronary circulation. Patients complain of low blood pressure , excessive fatigue, and shortness of breath. As the disease progresses, syncope .
Tricuspid regurgitation can be manifested by cyanosis of the skin, rhythm disturbances such as atrial fibrillation , swelling, hepatomegaly , and swelling of the neck veins.
With pulmonary regurgitation, all clinical symptoms are associated with hemodynamic disturbances in the systemic circulation. Patients complain of swelling , shortness of breath , acrocyanosis , enlarged liver, and rhythm disturbances.
Symptoms of aortic valve regurgitation
With chronic development, symptoms are usually absent for a long time, and then appear as follows:
- shortness of breath (initially manifests itself during physical activity, later in the absence of treatment - at rest);
- bradycardia, mainly at night;
- angina pectoris also at night.
Symptoms of acute regurgitation are:
- severe shortness of breath;
- presyncope and fainting;
- decrease in pressure;
- chest pain;
- loss of strength;
- sudden weakness;
- pallor;
Important! If you experience these symptoms, you should consult a doctor immediately!
In addition, aortic regurgitation may be accompanied by pulmonary edema, in which the following symptoms are observed:
- hoarse breathing;
- moist rales in the lungs;
- feeling of lack of air;
- bluish skin;
- when coughing, sputum with foam and blood comes out;
- heart sounds are muffled.
Tests and diagnostics
Diagnosis of regurgitation includes collecting anamnesis, objective and instrumental examination data, which allow you to visually assess the structure of the heart, the movement of blood through the cavities and vessels.
Inspection and auscultation make it possible to assess the location and nature of the heart murmur. Aortic regurgitation is characterized by a diastolic murmur on the right in the second hypochondrium; with pulmonary valve incompetence, a similar murmur is heard to the left of the sternum. With tricuspid valve insufficiency, a characteristic murmur is heard at the base of the xiphoid process. With mitral regurgitation, there is a systolic murmur at the apex of the heart.
Basic examination methods:
- ECG;
- Heart ultrasound with Doppler;
- blood chemistry;
- general blood analysis;
- functional stress tests;
- R-graphy of the chest organs;
- Holter monitoring ECG.
Prevention and prognosis
A healthy lifestyle is recommended to prevent any disease. A normal work and rest schedule, reasonable physical activity, lack of stress and harmful addictions makes the likelihood of getting sick minimal. A very important aspect is the timely and correct treatment of colds, the obligatory clarification of the causes of systematic ailments. If the patient has undergone surgery for a heart defect or other pathology, it is very important to follow all clinical recommendations of cardiologists and carry out rehabilitation measures.
The prognosis for tricuspid regurgitation is positive; in childhood it can level out with age. For an adult, grade 1 pathology detected by chance is considered a functional norm that does not require treatment. If tricuspid insufficiency occurs in combination with other complications, the patient is assigned a disability group.
Be attentive to yourself and your children, do not ignore periodic ailments. Dangerous conditions may be masked behind them.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner
Procedures and operations
In cases of acute regurgitation, patients undergo emergency valve replacement. The modified valve is removed and an artificial one is installed in its place. In some cases, valve repair is sufficient. During the rehabilitation period, patients are prescribed medications that support normal cardiac activity: vasodilators and nootropics. In case of a chronic process, surgical interventions to replace the valve are also performed routinely as negative dynamics progress. In the absence of negative symptoms and stable EchoCG indicators, symptomatic therapy is prescribed.
Prognosis of aortic valve regurgitation
The prognosis depends on the development and stage of the underlying disease, and on the degree of regurgitation. Timely treatment, in particular surgical treatment, is also important. In its absence, heart failure can develop within two years from the onset of the first symptoms.
All of the following forecasts are given taking into account timely replacement of the valve. With minimal and moderate regurgitation (grades 1 and 2), the prognosis for the next 10 years is quite high - 80 - 95%. This indicator reflects how important it is to diagnose pathology on time. The higher the degree of regurgitation, the more noticeably the prognosis decreases. At grade 3 it is approximately 50%, and at grade 4 cardiac death may be sudden. This is also typical during the acute development of pathology.
To improve the prognosis, all patients with any stage of the disease should follow a healthy lifestyle, which includes:
- giving up bad habits (alcohol, especially in excess, and smoking);
- adherence to a diet (regular balanced meals without overeating);
- normalization of body weight;
- normalization of physical activity (strenuous training should be switched from walking in the fresh air and moderate exercise);
- avoidance of stressful situations.
Regularly undergo preventive examinations, consult a doctor at the first signs of illness and lead a healthy lifestyle, this will help you avoid many dangerous diseases. Be healthy!
Consequences and complications
In acute mitral regurgitation, the prognosis is extremely unfavorable in the absence of timely surgical care. The prognosis worsens with the addition of heart failure. In the second degree of the disease, the 5-year survival rate without surgery is 38% for men and 45% for women. Regurgitation can be complicated by endocarditis (non-infectious and infectious origin), rhythm disturbances, myocardial infarction , heart failure .
Diagnostic methods
When examining the patient, typical signs of aortic regurgitation are revealed:
- pale skin;
- cyanosis of the fingers, tip of the nose and lips;
- “dancing carotid” – noticeable pulsation of the carotid arteries;
- nodding your head to the beat of your pulse;
- rhythmic dilation and constriction of the pupils;
- trembling of the soft palate and uvula;
- when measuring pressure - low diastolic, high systolic and pulse;
- visible apical push;
- when palpating the xiphoid process, pulsation of the aorta is felt;
- decreasing murmur during diastole, weak double tones, double murmurs.
To instrumentally confirm the diagnosis, the following methods are used:
- electrocardiography – hypertrophied LV myocardium, in the later stages and right sections;
- phonocardiography – heart murmurs in accordance with the stage of the process;
- Ultrasound of the heart - a defect in the closure of the valves, an increase in the size of the heart chambers, the amount of blood returning to the left ventricle;
- radiography - the LV cavity is expanded, the aortic shadow is, the apex is moved downward and to the left, venous stagnation is noticeable in the lung tissue;
- aortography – regurgitation through an open valve in the diastole phase;
- cardiac probing helps determine the volume of blood ejection and return, pressure in the cavities;
- MRI, MSCT are prescribed for preoperative diagnosis and dynamic monitoring after surgery or in the compensation stage.
List of sources
- L.A. Boqueria, O.L. Bockeria, E.R. Jobava review article “Functional mitral regurgitation in atrial fibrillation”, 2015
- Mashina T.V., Golukhova E.Z. Left ventricular diastolic dysfunction in patients with atrial fibrillation: pathogenetic mechanisms and modern ultrasound assessment methods (analytical review). Creative cardiology. 2014
- Karpova N.Yu., Rashid M.A., Kazakova T.V. , Shostak N.A. Aortic regurgitation, Regular issues of “RMZh” No. 12 from 06/02/2014
Symptoms experienced by the patient
Damage to the tricuspid valve is accompanied by nonspecific symptoms, the severity of which depends on the stage of the pathology and the level of decompensation of functions. In clinical practice, there are 3 degrees of acquired valvular disease:
- 1st degree regurgitation on the tricuspid valve (“soft”) is characterized by minor manifestations of blood stagnation in the systemic circle (moderate swelling in the legs by the end of the day);
- with regurgitation of the tricuspid valve of the 2nd degree, an expansion of the lumen of the right atrioventricular orifice to 10 cm2 is observed, with a moderate disturbance of blood flow in the portal vein of the liver, swelling of the neck veins, and pronounced edema in the lower extremities;
- regurgitation of the 3rd degree (“acute”) with expansion of the cavities of the right chambers, increased pressure in the cavitary veins, enlargement of the liver and spleen, severe edema in the extremities, accumulation of fluid in the chest and abdominal cavity.
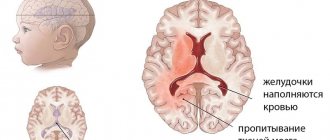
Functional failure develops during a growth spurt in a child (7-9 and 14-17 years old) and is associated with prolapse of the valve leaflets during ventricular systole into the atrium. The pathology does not require special treatment, only dynamic observation.
The patient's main complaints are related to blood stasis and are presented:
- pain in the right hypochondrium (impaired blood flow from the liver stretches the organ capsule and causes pain);
- shortness of breath, heaviness in the chest due to fluid accumulation;
- swelling of the neck veins (pulsation of the latter is visible upon examination);
- swelling in the legs, developing in the evening, cyanotic, cold, dense;
- increase in abdominal volume (due to free fluid).
Secondary symptoms include a feeling of tightness in the chest, interruptions in heart function, and freezing.
Diagnosis of deviation
Mitral-papillary dysfunction and any other abnormality can begin to be treated only after the main diagnosis has been established. Diagnostics include:
- Ultrasound;
- electrocardiogram;
- laboratory research.
Moderate tricuspid or any other regurgitation may not appear for a long time. Pathology can only be detected using ultrasound. The degree of severity is clarified using an electrocardiogram.
During the initial examination, the doctor examines the sick person. He clarifies what health complaints are present. The doctor then provides a referral for laboratory tests. Only based on their results, ultrasound and ECG are performed.
ECG allows you to reliably determine the severity of the disease
It is impossible to make a diagnosis on your own. Symptoms do not allow us to determine which valve pathology is present.
Features of mitral valve prolapse 2nd degree
When the ventricle is in systole, the valves of the MV close tightly, which prevents blood flow from returning in the opposite direction.
MVP is that the mitral valve leaflets (or one of them) sag into the cavity of the left atrium.
As a result, a small hole is formed through which some of the blood is directed back into the left atrium. This process is known as regurgitation.
According to the degree of regurgitation, experts distinguish several types of mitral valve prolapse:
- 1st degree: 1st degree mitral valve prolapse is characterized by the fact that the valve flaps bend from 3 to 6 mm. At the same time, the level of reverse blood flow is insignificant, which does not provoke the occurrence of severe pathology. Symptoms are mild or do not appear at all. The first degree of MVP does not harm human health. With this diagnosis, people can play sports;
- 2 degrees: second degree prolapse manifests itself when the mitral valve leaflets bend from 6 to 9 mm. Patients diagnosed with grade 2 MVP should be under the supervision of specialists and also periodically undergo preventive drug treatment;
- 3 degrees: in this case, the deflection of the valve halves is more than 9 mm. In a patient with regurgitation of this size, there is a high probability of disruption of the functioning of the cardiovascular system or the structure of the heart. Treatment of third-degree MVP is carried out surgically (suturing the halves of the mitral valve or installing a mitral valve prosthesis).
When classifying prolapse, factors such as the manifestation of symptoms and their intensity are taken into account. The classification of MVP is a determining indicator when choosing a treatment method.
Causes
Pathology can develop as a result of exposure to several factors. Experts divide all the reasons into two large groups:
- Congenital. This may be a hereditary predisposition. If any of the relatives of the unborn child is diagnosed with MVP or has diseases of the cardiovascular system, there is a high probability that the newborn will have prolapse.
- Purchased. There are several reasons whose impact on the human body can lead to the development of pathology. Among the most common are the following:
- mechanical damage to the integrity of the chest, which is accompanied by injury to the heart or internal organs;
- chronic form of coronary heart disease;
- disruption of the functioning of the coronary blood supply system;
- hyperthyroidism (the thyroid gland secretes an increased amount of hormones such as triiodothyronine or thyroxine);
- the patient has had rheumatic fever;
- myocarditis (inflammatory process of the heart muscle - myocardium).
If the above factors affect the human body, you should consult a specialist to determine the state of the cardiovascular system.
If a pregnant woman’s closest relatives have those who suffer from cardiovascular diseases, she must inform the obstetrician-gynecologist who is caring for her pregnancy about this.
Such women are under special control of doctors.
Symptoms
- severe headaches;
- weakness;
- fast fatiguability;
- dizziness;
- lack of air;
- frequent fainting conditions.
Experts consider pain in the chest area to be the most striking sign. As a rule, the pain is stabbing or squeezing in nature. The duration of pain attacks ranges from 10 seconds to 5 minutes.
The frequency of pain also varies: in some patients it may occur once over several days, while some complain of attacks of pain two or more times a day.
The intensity and frequency of pain attacks is directly dependent on the psycho-emotional state of the patient, as well as the amount of physical stress on the body.
- a violation of the structure of the child’s jaw and nasopharynx, known as the “Gothic” palate;
- articular hypermobility - a disorder in the structure of the connective tissue that makes up cartilage and joint capsules, which leads to the fact that the tissue is greatly stretched and the joints become very mobile;
- flat feet;
- osteochondrosis, which develops in early childhood;
- Schmorl's hernia;
- myopathy, etc.
The manifestation of these symptoms in both children and adults is a signal for immediate contact with specialized specialists for a medical examination.
Treatment
Children diagnosed with mitral valve prolapse with mild regurgitation are under the supervision of specialists. And with a diagnosis of grade 2 MVP, they are exempt from physical education on a general basis, and can only engage in specialized groups.
Patients with grade 1 regurgitation usually do not require treatment. It is enough to undergo a comprehensive examination once a year.
In the case when a patient experiences rapid heartbeat, arrhythmia, autonomic disorders, or mitral valve insufficiency, he needs the use of therapeutic therapy.
- beta blockers - help reduce the frequency of heart contraction, as well as its strength, reduce blood pressure;
- disaggregating agents - this group of drugs is based on aspirin. They are prescribed to prevent the formation of blood clots after a patient has suffered a stroke;
- anticoagulants - used to prevent blood thickening as a prophylaxis against blood clots. It should be noted that taking anticoagulants must be carried out under the supervision of specialists in order to avoid the possibility of complications.
Mitral valve prolapse is a pathology in which its leaflets sag toward the left atrium during contraction of the left ventricle. This leads to a certain amount of blood being thrown into it. The disease often has no symptoms, making it difficult to diagnose. But if too much blood enters the atrium, then surgical intervention is necessary.
Protrusion of the valve leaflets is more often detected in childhood. But cases of the disease developing in adults are not uncommon. Usually representatives of the fair sex suffer from this after 35 years.
The reasons for the development of the problem have not been precisely established. Scientists were able to reveal that connective tissue pathologies contribute to the occurrence of the disorder.
Depending on the type, the disease can occur as a result of the influence of various factors:
- Congenital forms occur when a child has myxomatous degeneration, which is a pathological process affecting connective tissue. The disorder is also associated with the effects of toxic substances on the fetal heart during intrauterine development.
- Acquired forms occur as a result of rheumatism, ischemic disorders, endocarditis, and injuries in the chest area.
Varieties
Depending on the severity of prolapse symptoms, there are:
- First degree. Mitral valve prolapse of the 1st degree in the mildest form. In this case, prolapse of no more than six millimeters is observed.
- Second degree. With it, prolapse increases to nine millimeters.
- Third degree. In this situation, the sashes sag by a centimeter or more.
Regurgitation is also taken into account. It comes in different types depending on how far the blood returns to the atrium. The doctor needs to know this subtlety. It is enough for the patient to find out whether it matters or not.
Symptoms
A certain proportion of patients do not experience any signs of the disease. In this case, it is accidentally detected on ultrasound.
With congenital prolapse, patients suffer from discomfort in the heart, which is observed during periods of emotional stress. At the same time, there is tingling and aching in the chest, shortness of breath, and dizziness. A person can remain in this state for several days or hours.
Patients also develop vegetative-vascular dystonia, due to which:
often stomach and headache;- the temperature periodically rises to 37 degrees;
- there is a feeling of a lump in the throat;
- urination becomes more frequent;
- fatigue is felt, physical activity is difficult to tolerate;
- health deteriorates depending on weather conditions.
If the psycho-emotional state is not corrected, the patient will suffer from panic attacks and depression, which can cause hysteria and psychopathy.
Symptoms of mitral valve prolapse resulting from various diseases depend on the underlying cause:
- If the pathology is associated with infectious processes, then the patient suffers from inflammation of the endocardium, which is accompanied by poor exercise tolerance, weakness, shortness of breath, and interruptions in heart function.
- With prolapse after a heart attack, patients suffer from severe chest pain, shortness of breath, cough, and rapid heartbeat.
- As a result of injury, the chords that regulate the valve leaflets can be torn. In this case, the patient suffers from shortness of breath and cough, and may produce pink sputum.
Diagnostic methods
In most cases, the presence of prolapse is discovered accidentally. The problem is identified during auscultation, electrocardiogram, and ultrasound examination. To confirm your suspicions:
An ultrasound with Doppler ultrasound is performed to determine the degree and volume of regurgitation.- Daily Holter monitoring is prescribed to detect rhythm disturbances, extrasystoles, weakness of the sinus node and other abnormalities.
After this, a treatment option is selected.
Therapy
Most often, with prolapse there is no need for special treatment, since there are no significant deviations in the functioning of the heart. In this case, the patient should regularly visit a cardiologist, and also:
- do an ultrasound once or twice a year;
- monitor oral hygiene and prevent dental diseases;
- do not smoke and avoid caffeine and alcohol-containing drinks;
- establish a normal regime of physical activity.
It is determined individually whether there is a need for medications. It is usually practiced to prescribe vitamins, magnesium preparations, cardioprotectors and adrenergic blockers.
In case of severe disturbances in the psycho-emotional state, they resort to the help of a psychotherapist. In severe cases, you cannot do without antipsychotics and tranquilizers.
If grade 2 or first mitral valve prolapse develops, then there are no significant hemodynamic disturbances. But the third requires serious treatment. In some cases, it is necessary to replace the mitral valve with an artificial one.
Forecast
Degrees
Regurgitation can have varying degrees of deviation from the normal state:
- 1st degree. Weakly expressed. It's not clear exactly how much blood is returning. The diameter of the jet is up to 1 cm. The pathology manifests itself weakly, or there are no symptoms at all. At this stage, the pathology is difficult to diagnose. More often it is determined by chance. However, it is at this stage that it is best to begin surgical treatment.
- 2nd degree. Moderate. The normal flow is disrupted by 2 cm of volume or more. The patient can only be restored quickly. Clinical manifestations are mild. The patient complains of chest pain, shortness of breath with heavy exertion. There is still a chance for a cure. Extracardiac and cardiac defects may occur, but the chances of this happening are low. The patient has a high probability of living a full, long life, even if minor defects appear.
- 3rd degree. Expressed. The blood stream exceeds 2 cm. Congestive chronic heart failure develops. Recovery is possible, but it will not be complete. Lifelong maintenance treatment will be required.
- 4th degree. Terminal. All organs and systems change significantly: liver, kidneys, heart, brain. Surgical treatment at this stage does not make sense. Such a patient will no longer be able to recover. There is a short period of life left. The task of doctors is to ensure decent quality. Ultimately, acute heart failure and death occur.
- Sometimes grade 5, physiological, is distinguished. With it, the valve leaflets are absolutely healthy, without changes, but you can notice a disturbance in the blood flow in the area of the leaflets themselves. The blood creates small areas of swirls. More often the functional type is designated as 0-1 degree. It is often diagnosed in tall and extremely thin people. A number of medical sources express the opinion that the functional type occurs in 2/3 of the total number of healthy people. A person can live a long active life and not even suspect that he has a “surprise” valve. If this pathology does not progress, it is absolutely safe.
It is very important to determine exactly the stage of the disease. The method of diagnosis, tactics and success of treatment depend on this.
Treatment
Therapy for aortic regurgitation has two main goals:
- Prevent the development of complications - heart failure and death of the patient.
- Improve his quality of life.
Conservative treatment
Treatment with medications is aimed at reducing the level of SBP (systolic blood pressure) and reducing the amount of blood flowing back.
Drugs that are effective in this case are vasodilators of different groups:
- calcium channel blockers (nifecard);
- ACE inhibitors.
Medicines are indicated in the following cases:
- There are contraindications for surgical treatment or the patient is unwilling to resort to surgical treatment - drugs are prescribed for a long time.
- Severe manifestations of heart failure or severe regurgitation before surgical treatment are prescribed in a short course.
- Severe clinical manifestations, LV dilatation, but EF is normal - prescribed to slow progression.
Indications for surgery:
- Patients with EF less than 55%, LV ESD more than 55 mm, LV ESD more than 75 mm, even without visible manifestations.
- Severe symptoms (signs appear daily with exercise or a special stress test).
- Marked expansion of the LV cavity even with normal ejection fraction.
- Planning of other operations on the heart and blood vessels.
Mitral regurgitation: degrees, causes and treatment
Mitral regurgitation is dysfunction of the mitral valve leaflets. The mitral valve is located between the left ventricle and the left atrium. When the left atrium contracts, blood enters the ventricle. After this, the left atrium is blocked by the mitral valve, and blood from the left ventricle enters the aorta.
If the mitral valve does not provide complete blocking, its walls do not contract sufficiently and begin to sag, then this leads to the opposite process - the flow of blood from the left ventricle into the left atrium. This process leads to poor circulation. The cardiovascular system slows down the process of pumping blood. The pressure begins to drop, which causes a shortage of oxygen supplied to organs and tissues.
Causes
Mitral regurgitation can develop against the background of congenital or acquired pathologies.
Causes of birth defects:
- hereditary pathology;
- failure of heart formation during intrauterine development;
- mitral valve deformation.
Causes of acquired pathology:
- rheumatism;
- systemic lupus erythematosus;
- infective endocarditis;
- myocardial infarction;
- chest injury.
Classification
Depending on the volume of counterflow of blood in case of malfunction of the mitral valve, several degrees of pathology are distinguished:
- Mitral regurgitation of the 1st degree is accompanied by a backflow of no more than 25%. A pathological deviation in the initial stage may not manifest itself in any way, since the patient does not experience any complaints. The ECG does not reveal any abnormalities in the functioning of the valve. Stage 1 pathology can only be detected using Doppler ultrasound.
- Mitral regurgitation of the 2nd degree is a more serious pathology. The counterflow volume reaches 50%, which is the cause of pulmonary hypertension. This condition can lead to secondary changes in the heart muscle. An ECG reveals abnormalities due to the expansion of the boundaries of the heart. Drug treatment is required.
- In grade 3 pathology, the reverse flow of blood from one chamber to another reaches 90%. Secondary changes in the myocardium occur in the form of left ventricular hypertrophy. There is a shift in the borders of the heart to the left side. The changes are clearly visible on the ECG.
- Grade 4 mitral regurgitation is a severe form that can lead to complete loss of performance. Treatment with medications is not effective and surgery is required.
According to the clinical course, mitral valve regurgitation is divided into acute and chronic. In the first case, the changes are sudden. The chronic form is accompanied by a gradual increase in valve regurgitation.
Symptoms
With grade 1 regurgitation, the pathology has no obvious signs. This condition can last up to several years.
Stage 2 is characterized by the following symptoms:
At grade 3 there is:
Stage 4 is characterized by the occurrence of atrial fibrillation and heart failure.
Diagnostics
Mitral regurgitation is diagnosed using cardiac ultrasound. In some cases, Doppler ultrasound is used, which determines the degree of pathology.
ECHO-CG is also performed to determine the cause of regurgitation.
The following are carried out as auxiliary studies:
During preoperative preparation, coronary angiography is prescribed. This examination is also carried out in case of suspicion of the ischemic nature of the emerging pathology. Treatment is prescribed by a doctor after appropriate diagnosis.
Treatment measures
Drug treatment of mild forms of pathology that are asymptomatic is not required.
For stage 2 defects, the following is prescribed:
Treatment with indirect anticoagulants is appropriate for the development of atrial fibrillation.
In grades 3-4, medication treatment is not advisable and surgical intervention is required.
Forecast
Pathology progression occurs in only 5–10 patients out of 100. The minimum risk group has a prognosis of 80% five-year survival and 60% ten-year survival.
With an ischemic nature, the clinical picture is less favorable: severe circulatory impairment occurs, which reduces survival and worsens the prognosis.
Patients with mitral regurgitation of any degree should be regularly examined by a cardiologist, cardiac surgeon and rheumatologist to assess the stage of development of the pathology.
The mechanism of regurgitation in normal and pathological conditions
Cardiologists identify minor physiological regurgitation, which is possible under normal conditions. For example, 70% of tall adults have incomplete closure of the tricuspid valve, which the person is not aware of. Ultrasound reveals slight swirling flows when the valves are completely closed. This does not affect general blood circulation.
Pathology occurs during inflammatory processes:
- rheumatism,
- infective endocarditis.
Most typical for mitral localization, the formation of heart disease. It should not be confused with prolapse (stretching and bending of the valves into the atrium). It is with prolapse that physiological regurgitation often occurs and is found in growing children and adolescents. It is taken into account as a possible cause of extrasystole. The child must be observed by a cardiologist and re-examined. No special treatment is required.
The formation of scars after an acute heart attack, against the background of cardiosclerosis, in the area approaching the valve leaflets and threads, leads to breakdown of the necessary tension mechanism and changes the shape of the leaflets. Therefore, they do not completely close.
In a pathological process, an equally significant role is played by the diameter of the outlet, which must be blocked. Significant enlargement due to left ventricular dilatation or hypertrophy prevents the tight junction of the aortic valve leaflets.
Causes of pathologies
In medicine there is the concept of physiological regurgitation, in which there are no valve pathologies. Such phenomena concern valvular blood turbulence at the tricuspid and mitral valves and occur in thin, tall people.
Disorders begin when the valve flaps do not close completely and their insufficiency occurs. The cause is congenital heart defects (including the valves themselves), inflammatory changes in the endocardium that covers the valves, and serious cardiac and pulmonary pathologies. A common cause of valve problems is rheumatism.
Features of treatment
Treatment of mitral or any other regurgitation of the 1st degree is not carried out. The patient is registered with a cardiologist. He must undergo regular diagnostics to prevent the development of complications. In addition, you need to give up all bad habits.
With 3-4 degrees of pathology, the patient may be referred for prosthetics. The operation is considered difficult and often provokes the development of complications.
There is no specific set of medications for the treatment of regurgitation. Medicines are selected based on the main diagnosis.
If the patient has no complaints, it is enough to follow the doctor’s general recommendations. They consist of moderate physical activity and maintaining a healthy lifestyle.
You can learn in detail about the causes and mechanisms of development of mitral regurgitation by watching the video below: