Article publication date: 06/29/2018
Article updated date: 09/04/2018
Author: Yulia Dmitrieva (Sych) – practicing cardiologist
Tricuspid regurgitation is a cardiac pathology in which blood flows from the right ventricle back into the right atrium through the tricuspid, or tricuspid, valve, contrary to normal circulation.
The Latin “gurgitare” is translated as – to flood, “re” indicates a reverse or repeated action.
What kind of diagnosis is this?
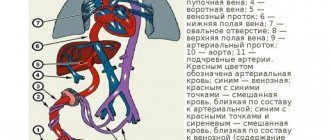
The human heart has four chambers - the left and right ventricles and atria. They are separated by partitions with valves that normally allow blood to flow in only one direction.
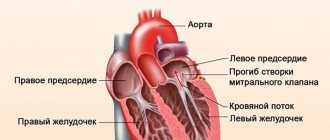
Tricuspid (tricuspid) - connects the right atrium and ventricle. Regurgitation is a situation in which, when the right ventricle contracts, blood splashes through this valve not only into the pulmonary circulation, but also back into the atrium.
This diagnosis is not an independent disease; it only signals problems with the functioning of the heart. This pathology can affect all heart valves: mitral, aortic, pulmonary artery and tricuspid.
Among all possible forms, tricuspid is less common than aortic and mitral, affecting the ascending aorta, but it is no less dangerous.
This pathology does not have its own ICD 10 code; it is included in the list of non-rheumatic pathologies of the tricuspid valve - I36.1-I36.9.
The concept of tricuspid regurgitation
The term "regurgitation" is a medical one. It comes from the Latin word gurgitare (translated as “to flood”) and the prefix re-, meaning “again, back.” In cardiology, regurgitation is the reverse flow (reflux) of blood from one chamber of the heart to another.
The heart consists of four chambers (2 atria and 2 ventricles), separated by septa and equipped with four valves. These are the mitral, aortic, pulmonary artery and tricuspid (three-leaf). The latter connects the right ventricle and the right atrium. In each of the valves, for various reasons, blood flow disturbances can occur, which means that there are four types of this disease.
Aortic and mitral regurgitation are most often diagnosed; tricuspid regurgitation is slightly less common. But the danger is that during diagnosis one can confuse different forms of this pathology. In addition, sometimes disturbances in the functioning of different heart valves occur simultaneously in a patient.
An important point: tricuspid valve regurgitation is not an independent disease and a separate diagnosis. This condition usually develops due to other serious problems (heart, lung, etc.), and therefore is usually treated in combination. And most importantly, an anomaly with a frightening Latin name should not be considered a death sentence. It is quite easy to diagnose, it is quite possible to cure or at least strictly control it.
Types of diseases and causes of their development
Tricuspid regurgitation can be:
Pathology is also classified according to the cause of its occurrence:
- Primary. Occurs as a result of various diseases: rheumatism and arthritis, infective endocarditis, myocardial infarction, deposition of connective tissue plaques on the walls of the valve, cardiac muscle and blood vessels, Marfan syndrome, hereditary connective tissue pathology, Ebstein's anomaly, displacement or prolapse of the leaflets into the ventricular cavity.
- Secondary. The cause of this form of pathology may be cardiomyopathy, increased pressure in the pulmonary vessels, causing dilatation, expansion or hypertrophic changes in the right ventricle.
Based on tricuspid valve insufficiency, the following forms are distinguished:
- Organic or absolute. It involves changing the valves, which interferes with their normal operation.
- Functional or relative. It occurs due to abnormalities of the valve itself: its stretching or damage to the heart tissue.
Congenital
This form of pathology occurs in the fetus at 11-13 weeks of pregnancy, or in an infant in the first months of life. During pregnancy, the pregnant woman is assigned to undergo screening, with the help of which it is possible to identify her.
In the prenatal period, nothing can be done about the pathology; the child is born with it. It manifests itself almost immediately after birth in the form of respiratory disorders, failure of the right ventricle of the heart, and cyanosis of the skin.
If there is a congenital abnormality, the function of the heart valve may return to normal on its own over time.
A baby with this diagnosis needs to be regularly examined by a cardiologist, and the mother needs to monitor the baby’s health. An advanced disease can lead to disability, even death.
This pathology most often appears in newborns with chromosomal abnormalities, but can also develop in a healthy embryo.
Acquired
Appears in adults against the background of cardiovascular diseases.
It never occurs in isolation, only as a consequence of another disease related to the functioning of the heart.
Possible stages
The degree of development of this pathology is determined by the intensity of the reverse blood flow.
There are four of them in total:
- Stage 1 – Slight outflow, with no symptoms observed.
- Stage 2 – The length of the jet is up to 2 cm.
- Stage 3 – The length of the stream exceeds 2 cm.
- Stage 4 – Significant regurgitation extending deep into the right atrium.
There is also a fifth or zero stage, called physiological or valvular. With it, a turbulence is formed at the valves, due to which a minimal amount of blood flows back. This stage is not a pathology and most often does not affect health in any way.
Symptoms
Symptoms vary depending on the stage of the pathology. In the first stages, symptoms are minor or virtually absent.
At stages 3 and 4, the patient exhibits a pronounced clinical picture.
Table of characteristic symptoms at different stages of pathology:
| Stage of tricuspid regurgitation | Symptoms of the disease |
| First | Absent or may appear as excessively intense pulsation of the veins in the neck. |
| Second | The neck veins are noticeably pulsating and trembling. |
| Third and fourth | Swelling of the jugular vein. |
Blueness of the skin on the lips, nose, under the nails.
Swelling of the lower extremities.
Shortness of breath, fatigue during physical activity (as it progresses, it is also diagnosed at rest).
Pain in the right hypochondrium.
Enlarged liver.
Most of the signs are similar to other cardiovascular diseases, but the most clear indication of tricuspid valve regurgitation is swollen jugular veins and the development of atrial fibrillation.
How is it diagnosed?
The main method for diagnosing regurgitation is ultrasound examination of the heart.
Other diagnostic procedures to clarify the diagnosis:
- Taking an anamnesis, external examination, listening to the heart using a phonendoscope.
- Electrocardiography.
- Echocardiographic study with Doppler analysis.
- Chest X-ray.
- Cardiac catheterization: A diagnostic procedure in which a catheter and x-ray are used to examine the condition of the arteries and blood supply to the heart.
Treatment methods at different stages
In mild cases of pathology, treatment is mainly supportive and aimed at stabilizing blood pressure. The patient is under the supervision of the attending cardiologist.
In case of progressive pathology, conservative therapy is prescribed, which is aimed not only at eliminating the dysfunction of the heart valve, but also at treating the root cause, i.e., the disease that caused it.
In later stages, tricuspid regurgitation is treated with the following surgical methods:
Drug therapy
Drug treatment of tricuspid valve regurgitation consists of:
- Diuretics. Diuretics that remove salts and water from the kidneys.
- Vasodilators. Vasodilator drugs widely used to treat cardiovascular diseases.
- Cardiac glycosides. Herbal medicines used to treat heart failure and have an antiarrhythmic effect.
- Metabolic drugs to improve oxygen supply to tissues.
- Potassium and magnesium preparations as universal cardioprotectors.
Drug therapy is prescribed if the pathology is hemodynamically insignificant, i.e. the vessels are not affected.
Valve plastics
Tricuspid valve repair is performed to correct insufficiency in hemodynamically significant heart defects and significant deformation of the leaflets.
This intervention is also called Boyd bicuspidalization. It involves placing sutures on the valve flaps to reduce its lumen.
Annuloplasty
This type of surgery is a type of plastic surgery.
It can be done in several ways:
- Annuloplasty with a support ring according to Carpentier. With this type of plastic surgery, corrective rings are used.
- Suture annuloplasty according to De Vega. In this case, a semi-purse string suture is placed on the valve gaskets.
- Annuloplasty according to Amosov. Similar to the De Vega method, differs only in the type of seam used.
Prosthetics
When tricuspid valve repair is impossible due to organic destruction or hemodynamically significant defects, prosthetics is performed, i.e. complete replacement.
Prostheses can be mechanical or biological; the latter are most often installed.
The choice in favor of such an operation should be made taking into account the patient’s age, contraindications to major surgery and anticoagulant therapy, and an assessment of the patient’s general condition.
Given that the hemodynamic conditions in the area of the tricuspid valve are less stressful, the degeneration of biological tissue occurs more slowly, so the prosthesis lasts longer than in the case of implantation of other heart valves.
Tricuspid regurgitation: what it is, degrees, symptoms, diagnosis
Tricuspid regurgitation is a cardiac pathology in which blood flows from the right ventricle back into the right atrium through the tricuspid, or tricuspid, valve, contrary to normal circulation.
The Latin “gurgitare” is translated as - to flood, “re” indicates a reverse or repeated action.
What kind of diagnosis is this?
The human heart has four chambers - the left and right ventricles and atria. They are separated by partitions with valves that normally allow blood to flow in only one direction.
Tricuspid (tricuspid) - connects the right atrium and ventricle. Regurgitation is a situation in which, when the right ventricle contracts, blood splashes through this valve not only into the pulmonary circulation, but also back into the atrium.
This diagnosis is not an independent disease; it only signals problems with the functioning of the heart. This pathology can affect all heart valves: mitral, aortic, pulmonary artery and tricuspid.
Among all possible forms, tricuspid is less common than aortic and mitral, affecting the ascending aorta, but it is no less dangerous.
This pathology does not have its own ICD 10 code; it is included in the list of non-rheumatic pathologies of the tricuspid valve - I36.1-I36.9.
Types of diseases and causes of their development
Tricuspid regurgitation can be:
- Congenital.
- Acquired.
Pathology is also classified according to the cause of its occurrence:
- Primary. Occurs as a result of various diseases: rheumatism and arthritis, infective endocarditis, myocardial infarction, deposition of connective tissue plaques on the walls of the valve, cardiac muscle and blood vessels, Marfan syndrome, hereditary connective tissue pathology, Ebstein's anomaly, displacement or prolapse of the leaflets into the ventricular cavity.
- Secondary. The cause of this form of pathology may be cardiomyopathy, increased pressure in the pulmonary vessels, causing dilatation, expansion or hypertrophic changes in the right ventricle.
Based on tricuspid valve insufficiency, the following forms are distinguished:
- Organic or absolute. It involves changing the valves, which interferes with their normal operation.
- Functional or relative. It occurs due to abnormalities of the valve itself: its stretching or damage to the heart tissue.
Congenital
This form of pathology occurs in the fetus at 11-13 weeks of pregnancy, or in an infant in the first months of life. During pregnancy, the pregnant woman is assigned to undergo screening, with the help of which it is possible to identify her.
In the prenatal period, nothing can be done about the pathology; the child is born with it. It manifests itself almost immediately after birth in the form of respiratory disorders, failure of the right ventricle of the heart, and cyanosis of the skin.
If there is a congenital abnormality, the function of the heart valve may return to normal on its own over time.
A baby with this diagnosis needs to be regularly examined by a cardiologist, and the mother needs to monitor the baby’s health. An advanced disease can lead to disability, even death.
This pathology most often appears in newborns with chromosomal abnormalities, but can also develop in a healthy embryo.
Acquired
Appears in adults against the background of cardiovascular diseases.
It never occurs in isolation, only as a consequence of another disease related to the functioning of the heart.
Possible stages
The degree of development of this pathology is determined by the intensity of the reverse blood flow.
There are four of them in total:
- Stage 1 - Slight outflow, with no symptoms observed.
- Stage 2 - The length of the jet is up to 2 cm.
- Stage 3 - The length of the stream exceeds 2 cm.
- Stage 4 - Significant regurgitation extending deep into the right atrium.
There is also a fifth or zero stage, called physiological or valvular. With it, a turbulence is formed at the valves, due to which a minimal amount of blood flows back. This stage is not a pathology and most often does not affect health in any way.
Symptoms
Symptoms vary depending on the stage of the pathology. In the first stages, symptoms are minor or virtually absent.
At stages 3 and 4, the patient exhibits a pronounced clinical picture.
Table of characteristic symptoms at different stages of pathology:
| Stage of tricuspid regurgitation | Symptoms of the disease |
| First | Absent or may appear as excessively intense pulsation of the veins in the neck. |
| Second | The neck veins are noticeably pulsating and trembling. |
| Third and fourth | Swelling of the jugular vein. Blueness of the skin on the lips, nose, under the nails. Swelling of the lower extremities. Atrial fibrillation. Shortness of breath, fatigue during physical activity (as it progresses, it is also diagnosed at rest). Pain in the right hypochondrium. Enlarged liver. |
Most of the signs are similar to other cardiovascular diseases, but the most clear indication of tricuspid valve regurgitation is swollen jugular veins and the development of atrial fibrillation.
How is it diagnosed?
The main method for diagnosing regurgitation is ultrasound examination of the heart.
Other diagnostic procedures to clarify the diagnosis:
- Taking an anamnesis, external examination, listening to the heart using a phonendoscope.
- Electrocardiography.
- Echocardiographic study with Doppler analysis.
- Chest X-ray.
- Cardiac catheterization: A diagnostic procedure in which a catheter and x-ray are used to examine the condition of the arteries and blood supply to the heart.
Treatment methods at different stages
In mild cases of pathology, treatment is mainly supportive and aimed at stabilizing blood pressure. The patient is under the supervision of the attending cardiologist.
In case of progressive pathology, conservative therapy is prescribed, which is aimed not only at eliminating the dysfunction of the heart valve, but also at treating the root cause, i.e., the disease that caused it.
In later stages, tricuspid regurgitation is treated with the following surgical methods:
- plastic;
- prosthetics;
- Annuloplasty.
Drug therapy
Drug treatment of tricuspid valve regurgitation consists of:
- Diuretics. Diuretics that remove salts and water from the kidneys.
- Vasodilators. Vasodilator drugs widely used to treat cardiovascular diseases.
- Cardiac glycosides. Herbal medicines used to treat heart failure and have an antiarrhythmic effect.
- Metabolic drugs to improve oxygen supply to tissues.
- Potassium and magnesium preparations as universal cardioprotectors.
Drug therapy is prescribed if the pathology is hemodynamically insignificant, i.e. the vessels are not affected.
Valve plastics
Tricuspid valve repair is performed to correct insufficiency in hemodynamically significant heart defects and significant deformation of the leaflets.
This intervention is also called Boyd bicuspidalization. It involves placing sutures on the valve flaps to reduce its lumen.
Annuloplasty
This type of surgery is a type of plastic surgery.
It can be done in several ways:
- Annuloplasty with a support ring according to Carpentier. With this type of plastic surgery, corrective rings are used.
- Suture annuloplasty according to De Vega. In this case, a semi-purse string suture is placed on the valve gaskets.
- Annuloplasty according to Amosov. Similar to the De Vega method, differs only in the type of seam used.
Prosthetics
When tricuspid valve repair is impossible due to organic destruction or hemodynamically significant defects, prosthetics is performed, i.e. complete replacement.
Prostheses can be mechanical or biological; the latter are most often installed.
The choice in favor of such an operation should be made taking into account the patient’s age, contraindications to major surgery and anticoagulant therapy, and an assessment of the patient’s general condition.
Given that the hemodynamic conditions in the area of the tricuspid valve are less stressful, the degeneration of biological tissue occurs more slowly, so the prosthesis lasts longer than in the case of implantation of other heart valves.
The operation is performed under anesthesia both with the beating heart and with a cardiopulmonary bypass machine connected.
Forecast
The prognosis of the pathology is favorable in the initial stages. Tricuspid regurgitation of the 1st degree is not very scary, does not require treatment, and allows the patient to lead a normal lifestyle. He just needs to be seen by a cardiologist.
Tricuspid regurgitation of the 2nd degree also does not require treatment if it does not cause health problems: heart failure, shortness of breath, swelling of the neck veins, etc. If you consult a doctor in a timely manner, if alarming symptoms appear, drug therapy is prescribed.
Tricuspid valve regurgitation grades 3 and 4 requires surgical intervention. The prognosis for surgery is generally positive: heart valve repair or replacement increases life expectancy. Implantation of a biological prosthesis has extremely positive reviews.
Mortality due to tricuspid valve regurgitation is caused by cardiovascular diseases that cause its malfunction. If left untreated, the disease can lead to serious consequences, even death. It is important to undergo regular medical checkups and monitor your health.
Additional questions
Are they allowed into the army with this diagnosis? With grade 1 tricuspid valve regurgitation, there are no contraindications to military service, but with a more severe degree of this pathology, exemption from military service is expected.
The same goes for playing sports. The initial stages of the pathology allow physical activity, but at stages 3 and 4 of regurgitation it is not recommended to engage in sports, since excessive physical activity can aggravate the disease and cause a deterioration in the person’s condition.
Dmitrieva Yulia (Sych) – In 2014, she graduated with honors from Saratov State Medical University named after V. I. Razumovsky. Currently working as a cardiologist at the 8th City Clinical Hospital in the 1st clinic.
Source: https://infoserdce.com/serdce/trikuspidalnaya-regurgitatsiya/
Forecast
The prognosis of the pathology is favorable in the initial stages. Tricuspid regurgitation of the 1st degree is not very scary, does not require treatment, and allows the patient to lead a normal lifestyle. He just needs to be seen by a cardiologist.
Tricuspid regurgitation of the 2nd degree also does not require treatment if it does not cause health problems: heart failure, shortness of breath, swelling of the neck veins, etc. If you consult a doctor in a timely manner, if alarming symptoms appear, drug therapy is prescribed.
Tricuspid valve regurgitation grades 3 and 4 requires surgical intervention. The prognosis for surgery is generally positive: heart valve repair or replacement increases life expectancy. Implantation of a biological prosthesis has extremely positive reviews.
Mortality due to tricuspid valve regurgitation is caused by cardiovascular diseases that cause its malfunction. If left untreated, the disease can lead to serious consequences, even death. It is important to undergo regular medical checkups and monitor your health.
Treatment methods
Therapy is carried out under the full supervision of a cardiac surgeon. Methods of exposure depend on the stage of the pathological process.
Grade 1 tricuspid regurgitation is the best time to start therapy. But there are no symptoms yet, identification is incidental (random), and does not pose any difficulties during a targeted search.
At this stage, dynamic observation for 3-5 years is indicated. In the absence of progression, with stagnation of the process, there is no need for treatment. Sometimes patients can live a quality life without knowing about their condition, without major restrictions.
Tricuspid regurgitation of grade 2 and higher is corrected strictly surgically. There are several intervention options.
But before the treatment stage, it is necessary to stabilize the patient’s condition, if there is time for that (planned operations).
Drugs used:
- Antiarrhythmics in the minimum dosage to restore an acceptable heart rate (Amiodarone, Hindin).
- Beta blockers (Metoprolol).
- Glycosides. In order to normalize myocardial contractility.
- Cardioprotectors.
- Anticoagulants. To prevent the formation of blood clots, which cause frequent premature death of patients.
- Diuretics in the treatment of early manifestations of renal conditions.
The duration of the preparatory period varies from 2 to 4 months, possibly more.
By the time of surgery, the rhythm should be stable, correct, blood pressure within the reference value or close to it.
Depending on the stage of the pathological process and the nature of the changes, plasty or prosthetics of the tricuspid valve is indicated. Both methods are generally equivalent.
Correction of pathologies and defects of distant organs is carried out under the supervision of specialized specialists. The list of techniques is wide and is determined based on the severity of the process.
Attention:
The use of folk remedies is impossible. Since the effect of them in case of organic deviation on the part of the cardiac structures is zero.
Changing your lifestyle will also not play a key role. It makes sense to give up smoking, alcohol and drugs. When carrying out severe therapy for third-party pathologies, correction by a treating specialist is recommended.
Additional questions
Are they allowed into the army with this diagnosis? With grade 1 tricuspid valve regurgitation, there are no contraindications to military service, but with a more severe degree of this pathology, exemption from military service is expected.
The same goes for playing sports. The initial stages of the pathology allow physical activity, but at stages 3 and 4 of regurgitation it is not recommended to engage in sports, since excessive physical activity can aggravate the disease and cause a deterioration in the person’s condition.
Specialized Academic Clinical Center
Preventive measures
Regurgitation of the tricuspid heart valve does not recur if all medical instructions are followed after treatment. The patient needs to lead a healthy lifestyle and refrain from bad habits. Drinking alcoholic beverages and smoking is excluded. This applies to those people who have undergone valve surgery and who have been diagnosed with the initial stage of the disease. Compliance with preventive measures will prevent further development.
Moderate exercise, proper diet and nutrition are required. Food should not be too fatty or peppery; it is not recommended to overuse pickles and sweets. It is necessary to carefully monitor your weight and avoid weight fluctuations. Rapid weight gain is especially dangerous.
Preventive measures include proper rest and sleep, and, if possible, avoiding stressful and nervous situations. Mandatory regular examination by a cardiologist to identify further development of tricuspid heart valve regurgitation.
Screening 1st (first) trimester. Screening timing. Screening results. Ultrasound screening.
Your baby has overcome all the difficulties and dangers associated with the embryonic period. It safely reached the uterine cavity through the fallopian tubes, trophoblast invasion into the endometrium occurred, and chorion formation occurred. The embryo grew and changed in an incredible way every week, the rudiments of all the most important organs and systems were formed, the torso, head, and limbs were formed. Finally, it grew to 10 weeks, acquiring all those necessary features, a child-like configuration, which made it possible to call it a fetus from that moment on. The time has come for screening of the 1st (first) trimester. Today we will talk about the timing of first trimester screening and the results of ultrasound screening.
This topic is vast and of course you can’t get rid of it with just one article. We have to look at many anomalies and malformations that may already be suspected or even diagnosed at this time. But let's start from the beginning.
What is screening?
Screening is a set of necessary activities and medical studies, tests and other procedures aimed at the preliminary identification of individuals among whom the likelihood of having a certain disease is higher than that of the rest of the population being examined. Screening is only the initial, preliminary stage of population examination, and individuals with positive screening results require subsequent diagnostic examination to establish or exclude the presence of a pathological process. The inability to carry out diagnostic tests that allow one to establish or exclude the presence of a pathological process with a positive screening result makes the screening itself pointless. For example, biochemical screening for fetal chromosomal diseases is not justified if subsequent prenatal karyotyping is not possible in a given region.
Any screening program must be accompanied by clear planning and assessment of the quality of screening, since any screening test conducted in the general population may cause more harm than good for the individuals being examined. The concept of “screening” has fundamental ethical differences from the concept of “diagnosis”, since screening tests are carried out among potentially healthy people, so it is very important that they have realistic ideas about the information that this screening program provides. For example, when conducting ultrasound screening for chromosomal pathology of the fetus in the first trimester of pregnancy, women should not have the idea that detecting an increase in the thickness of the nuchal space (NT) in the fetus necessarily indicates the presence of Down syndrome and requires termination of pregnancy. Any screening has certain limitations, in particular, a negative result of a screening test does not guarantee the absence of the disease, just as a positive test result does not indicate its presence.
When and why was first trimester screening invented?
Every woman has a certain risk that her child may have a chromosomal abnormality. It is for everyone, and no matter what lifestyle she leads and social status she occupies. In systematic (non-selective) screening, a specific screening test is offered to all individuals in a specific population. An example of such screening is ultrasound screening for fetal chromosomal abnormalities in the first trimester of pregnancy, which is offered to all pregnant women without exception at 11-13(+6) weeks.
And so, screening of the first trimester is a set of medical studies carried out at a period of 11-13 (+6) weeks, and aimed at the preliminary identification of pregnant women, among whom the likelihood of having a child with chromosomal abnormalities (CA) is higher than in other pregnant women.
The main place among detected CAs is occupied by Down syndrome (trisomy of 21 pairs of chromosomes). The English physician John Langdon Down was the first to describe and characterize the syndrome, later named after him, in 1862, as a form of mental disorder. Down syndrome is not a rare pathology - on average there is one case in 700 births. Until the mid-20th century, the causes of Down syndrome remained unknown, but the relationship between the likelihood of having a child with Down syndrome and the age of the mother was known, and it was also known that all races were susceptible to the syndrome. In 1959, Jerome Lejeune discovered that Down syndrome occurs due to trisomy of the 21st pair of chromosomes, i.e. the karyotype is represented by 47 chromosomes instead of the normal 46, since the chromosomes of the 21st pair, instead of the normal two, are represented by three copies.
In 1970, the first method of screening for trisomy 21 in the fetus was proposed, based on the increasing likelihood of this pathology with increasing age of the pregnant woman. When screening based on maternal age, only 5% of women would be classified as “high risk,” and this group would include only 30% of fetuses with trisomy 21 in the population. In the late 1980s, screening methods appeared that took into account not only age, but also the results of studying the concentration of such biochemical products of fetal and placental origin in the blood of a pregnant woman, such as alpha-fetoprotein (AFP), unconjugated estriol (uE3), human chorionic gonadotropin (hCG ) and inhibin A. This screening method is more effective than screening based only on the age of the pregnant woman, and with the same frequency of invasive interventions (about 5%) it can identify 50–70% of fetuses with trisomy 21. In the 1990s a screening method was proposed based on the age of the mother and the size of the fetal nuchal translucency thickness (nuchal translucency thickness) at 11–13 (+6) weeks of pregnancy. This screening method can identify up to 75% of fetuses with chromosomal abnormalities with a false-positive rate of 5%. Subsequently, the screening method, based on the age of the mother and the value of fetal TVL at 11–13 (+6) weeks of pregnancy, was supplemented by determining the concentrations of biochemical markers (free fraction of β-hCG and PAPP-A) in the mother’s blood serum in the first trimester of pregnancy, which made it possible to identify 85–90% of fetuses with trisomy 21. In 2001, it was found that during ultrasound examination at 11–13 weeks, in 60–70% of fetuses with trisomy 21 and in 2% of fetuses with a normal karyotype, the nasal bones are not visualized . The inclusion of this marker in a screening method based on ultrasound and determination of biochemical markers in the first trimester of pregnancy can increase the detection rate of trisomy 21 to 95%.
tricuspid regurgitation during pregnancy
I haven't written anything in my diary for a long time. During this time, I managed to pass 2 state exams, defend my diploma with excellent marks, and receive it (today, by the way, there was a ceremonial presentation). Go through an ultrasound screening, and I want to tell you more about this:
The ultrasound was scheduled for June 17 (Sunday) at 15:00. I had it all at the same paid clinic. My husband and I decided in advance that we would go together. In the morning I woke up and realized that my stomach was hurting. When it was time to go to the clinic, the pain was almost unbearable. But we shouldn’t cancel such a long-awaited trip because of this, in fact, especially since who knows what kind of queues they have there if we correspond... On the way we went to the pharmacy, bought Festal, I swallowed one of them in the hope that will take effect soon.
I had it all at the same paid clinic. My husband and I decided in advance that we would go together. In the morning I woke up and realized that my stomach was hurting. When it was time to go to the clinic, the pain was almost unbearable. But we shouldn’t cancel such a long-awaited trip because of this, in fact, especially since who knows what kind of queues they have there if we correspond... On the way we went to the pharmacy, bought Festal, I swallowed one of them in the hope that will take effect soon.
In short, the walk from our house to the clinic takes a maximum of 7 minutes. We arrived 10 minutes early, I also told the girl at the reception that it’s no big deal that we’re a little earlier, she somehow vaguely answered me that “I don’t care, there’s still a long line ”!!!!!! We approach the office, and there, as it turns out, there are 3 more women in front of us!!! Paid clinic! One of the best, if not the best! Admission 1200 rub. They called me 2 times to clarify and remind me about the time. "RECORD" yo-mayo! It's okay that we came for 10 minutes. earlier, otherwise there wouldn’t have been 3 people in line in front of us, but 4! (following me, another woman came up “Who’s last?”) We could have gone to find out, but the fact that I was getting sicker and worse every minute worse... The air conditioner in the corridor didn’t work (Was it there at all?) I was constantly feeling hot, there were three streams of sweat from my forehead... Okay, at least we bought some cool water on the way to wash down the pills, and I took a fan with me from home, So in general, I apologize, I threw off my hooves in this line. It’s not that it’s difficult for me to wait an extra 40 minutes, it’s just that when you have terrible cramps in your stomach and can’t breathe, you start to think about it.
Our turn has come (Hurrrra!). A pleasant female doctor was waiting for us in the office. My dear one modestly sat down on a chair waiting for the movie. I lay down on the couch, the doctor began to move this very thing over my stomach (due to the colic it was very unpleasant, because the stomach pain radiated to all parts of the abdomen)
Result:
The heartbeat is visualized, heart rate is 155 beats per minute (I think that if I didn’t feel so bad, it would be less)
Fetal CTE 57 mm (12-12 weeks)
Collar space 1.28 mm
The nasal bone is visualized
Ductus venosus is normal
There is no tricuspid regurgitation (I tried to find an explanation on the Internet what it is, but everything is so complicated... I didn’t even bother to delve into it, I realized that it’s not and that’s good)
Fetal anatomy is not changed
The bones of the cranial vault are satisfactory (the question arises: is it good or excellent in this case?)
«Butterfly" is not changed
The spine is not changed
The stomach is not changed
The anterior abdominal wall is unchanged
Urinary fluid is not changed
Limbs are not changed
The chorion is located on the back wall (here, as I understand it, I should be happy, because if I understood everything correctly, this means that the stomach will be neater than if it were located on the front wall, and I should supposedly feel the baby’s movements earlier)
The structure of the chorion is not changed
The internal pharynx is closed (here, if I understood correctly again, at this stage this is gud)
The walls of the uterus are without features
Ovaries without features
Visualization not changed
While the ultrasound was being done, the child seemed to be lying calmly, then he arched over and then jumped up. Mine asks the doctor: “Is it that he’s already moving like that????” (Oh, man! :)) I asked her if anyone would be visible (the age-old question :)) She said that it wouldn’t be visible, but she could guess. In short, she said that there is a very high probability that it is a boy, because... the genitals are curved to the top (in girls usually to the bottom at this stage) and even showed what’s what. She let me listen to the heart and displayed the cardiogram on the monitor.
As soon as I got off the couch, it immediately got worse. I started to feel sick (from the very first day of pregnancy I was deprived of such “happiness” as toxicosis). I tell her that I feel bad, I went to the air, my husband will take all the papers and photos. And I run to the toilet. Vomited. They ran home at the speed of light. The husband kept saying: “Just a little more, be patient with the little one, we’ll be home soon!” Eh, I thought we’d go to the bookstore and buy something for you in honor of such an event...” Then I didn’t understand anything at all, what does the bookstore have to do with it? I didn’t have the strength to ask, I run and understand that his emotions are bursting, he wants to discuss, but here I am and I feel so bad. In short, an acute attack of gastritis, as it turned out later, 3 days of a special diet, gastro-herbal collection and I was back to normal.
It’s a shame that such a wonderful day was ruined by my poor health! Words simply cannot express how pathetic it is!
And here is the photo
How does tricuspid valve regurgitation occur?
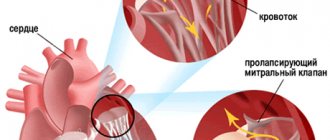
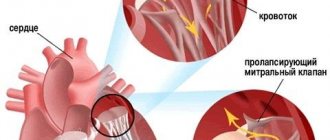
The tricuspid or tricuspid valve is located between the right atrium and the right ventricle; during diastole, its valves open, allowing venous blood to pass from the right atrium into the ventricle. During systole (contraction), the valve leaflets close tightly, and the blood entering the right ventricle enters the pulmonary artery and then into the lungs. When the tricuspid valve regurgitates, the blood from the right ventricle does not completely enter the pulmonary artery, but partially returns to the right atrium, and a reverse reflux of blood occurs - regurgitation. This occurs due to dysfunction of the tricuspid valve - when its valves do not close tightly, the entrance to the right atrium does not completely close. With tricuspid regurgitation, due to increased load, the atrium hypertrophies, and then the muscles stretch and increase in size. In turn, this leads to the entry of a large amount of blood from the atrium into the right ventricle during diastole, its further hypertrophy and dysfunction, which provokes stagnation in the systemic circulation.
What causes regurgitation of blood through the tricuspid valve?
The normal movement of blood through the right parts of the heart is ensured by the ability of the tricuspid valve leaflets to move synchronously with the phases of systole and diastole of the myocardium.
Valve defects, depending on the morphological substrate and functional disorder, are divided into:
- stenosis, which develops due to calcification, an inflammatory lesion. The pathology is characterized by a narrowing of the lumen of the orifice, which reduces the volumetric velocity of blood flow from the atrium to the ventricle;
- regurgitation (in the old terminology - insufficiency) - elongation of the chords, damage to valve structures by infectious processes contributes to the expansion of the lumen and pathological movement of blood during ventricular systole not only into the pulmonary artery, but also into the atrium;
- combined defect.
Pathologies of the tricuspid valve are rare acquired defects and most often develop as secondary changes against the background of decompensation of the condition.
The most common causes of tricuspid regurgitation:
- infective endocarditis is a bacterial pathology characterized by the entry of the pathogen into the blood and selective damage to the endocardial tissue. Involvement of the valves of the right half of the heart most often develops in injection drug users;
- chronic rheumatic heart disease is a consequence of an infection with beta-hemolytic streptococcus, which has cross-antigens with valve structures;
- systemic connective tissue pathologies: Ellesre-Danlos syndrome, Marfan syndrome, undifferentiated dysplasia syndrome;
- Ebstein's anomaly is a congenital valve malformation in which the leaflets develop not from the connective tissue of the fibrous ring, but from the myocardium of the right ventricle. The first signs of disorders are diagnosed during examination of the newborn in the maternity hospital;
- dilated cardiomyopathy. The resulting regurgitation is considered relative, since an increase in the size of the right atrioventricular orifice is associated with a pathological expansion of the cavities of the heart;
- carcinoid syndrome is a specific reaction of the body to malignant tumors of various locations. It is formed in response to the release of the metabolic product of cancer cells into the bloodstream: diarrhea, nausea, hot flashes (as during menopause), abdominal pain.
Most often, grade 1 tricuspid valve regurgitation is diagnosed in patients with decompensated mitral valve disease. Impaired blood outflow from the left atrium increases pressure in the pulmonary circle (pulmonary vessels), and secondarily in the right ventricle.
Causes and types of tricuspid regurgitation
There are several types of tricuspid valve insufficiency:
- Absolute or organic failure. The pathology is caused by damage to the valve leaflets, such as valve prolapse (sagging leaflets), due to a congenital disease - connective tissue dysplasia, also causes include rheumatism, infective endocarditis, carcinoid syndrome and others;
- Relative or functional deficiency. Occurs when the valve is stretched due to resistance to the outflow of blood from the right ventricle, with pronounced dilatation of the ventricular cavity caused by high pulmonary hypertension or diffuse myocardial damage.
Based on the severity of reverse blood flow, tricuspid regurgitation is divided into four degrees:
- 1st degree. Barely detectable backflow of blood;
- 2nd degree. Regurgitation is determined at a distance of 2 cm from the tricuspid valve;
- 3rd degree. Reverse flow of blood from the right ventricle is detected at a distance of more than 2 cm from the valve;
- 4th degree. Regurgitation is characterized by a large extent in the cavity of the right atrium.
The severity of blood return is determined using echocardiographic examination.
Symptoms
Patients with tricuspid regurgitation present with signs and symptoms of right-sided heart failure. The spectrum of symptoms depends on whether the condition is secondary to left ventricular (LV) dysfunction.
Common complaints in patients with LV dysfunction include the following:
- Shortness of breath on exertion
- Orthopnea
- Paroxysmal nocturnal dyspnea
- Ascites
- Peripheral edema
Exercise intolerance may also occur. Rarely, patients report angina, which can result from right ventricular overload and strain, even in the absence of coronary artery disease.
These patients, especially those who experience febrile episodes, should be questioned regarding risk factors for infective endocarditis, which is a common cause of tricuspid valvular disease. Risk factors include intravenous drug use, alcoholism, and a history of rheumatic fever.
Cardiovascular findings in patients with tricuspid regurgitation include the following:
- S 3 galloping rhythm
- Jugular venous expansion with prominent V-wave
- Some patients have a pansystolic murmur
- Reduced peripheral impulse volume secondary to disruption of forward flow; Patients with this sign may have relative hypotension secondary to therapeutic interventions used to reduce volume overload
- Pulmonary rales if tricuspid regurgitation is associated with left ventricular dysfunction or mitral stenosis
- Right ventricular pain and S4 surge, increasing with inspiration
- ascites
- Peripheral edema
- Cachexia and jaundice
- Atrial fibrillation
The pansystolic murmur associated with tricuspid regurgitation is high-pitched and loudest in the fourth intercostal space in the parasternal region. The murmur usually increases during inspiration and decreases in intensity and duration during standing and during the Valsalva maneuver. A short, early hum of diastolic flow may be present due to increased flow across the tricuspid valve.
Description of grade 1 tricuspid regurgitation
With regurgitation of the 1st degree, as a rule, the symptoms of the disease do not manifest themselves, and it can only be detected accidentally during electrocardiography. In most cases, grade 1 tricuspid regurgitation does not require treatment and can be considered normal. If the development of the disease is provoked by rheumatic defects, pulmonary hypertension or other diseases, it is necessary to treat the underlying disease that caused a minor defect in the tricuspid valve leaflets.
In children, this degree of regurgitation is considered an anatomical feature that may even disappear over time - without the presence of other cardiac pathologies, it usually does not affect the development and general condition of the child.
Tricuspid regurgitation in children
Reverse reflux of blood into the right ventricle is now increasingly being recorded in children, even before birth. Tricuspid regurgitation in the fetus can appear in the first trimester of pregnancy, at 11–13 weeks.
This feature often occurs in babies with chromosomal abnormalities (for example, Down syndrome). But a certain percentage of regurgitation is also observed in an absolutely healthy fetus.
Pediatric cardiologists report a rapidly growing number of cases of tricuspid anomaly in children of different ages. In most of them, regurgitation of the first degree is diagnosed, and today it is already considered a normal variant.
If the child does not have other heart pathologies, in the future there is a high chance that the valve will work on its own.
But if the congenital disease reaches the second or third stage, there is a risk of developing heart failure and right ventricular dysfunction in the future. Therefore, it is important for your child to regularly visit a cardiologist and follow all necessary measures to prevent heart disease.
Symptoms of tricuspid regurgitation
With grade 2 tricuspid regurgitation, as with other degrees, the disease often occurs without obvious symptoms. In severe cases of the disease, the following manifestations are possible:
- Weakness, fatigue;
- Increased venous pressure, leading to swelling of the veins of the neck and their pulsation;
- Enlarged liver with characteristic pain in the right hypochondrium;
- Heart rhythm disturbances;
- Edema of the lower extremities.
Auscultation (listening) reveals a characteristic systolic murmur, best heard in the 5th–7th intercostal space from the left edge of the sternum, intensifying with inspiration, quiet and inconsistent. With enlargement of the right ventricle and a large volume of blood entering it during diastole, a systolic murmur is also heard over the right jugular vein.
Passing a medical examination
After clarifying the essence of the pathology and the differences in severity, it is necessary to undergo a medical examination, since you will not be able to diagnose this disease yourself. The examination is carried out repeatedly to eliminate the risk of misdiagnosis.
The VVC raises the most questions about grade 2 prolapse. Young people need to adjust their regime: they should refrain from stress and overwork, heavy physical activity, which is not possible in the army. Therefore, intense military exercises are detrimental to the health of sick conscripts.
When determining the fitness category, members of the military commission rely on the following criteria:
- clear manifestations of heart rhythm disturbances;
- improper conductivity;
- heart failure.
If there are no characteristic symptoms of heart failure (shortness of breath, lethargy, accelerated heart rate), they will be accepted into the army with category “B-4”. The young man will be assigned to communications, radio engineering and other similar troops. If the listed symptoms appear after physical activity, even if they disappear after it, the conscript can count on release.
Diagnosis of tricuspid regurgitation
To diagnose tricuspid regurgitation, in addition to the history, physical examination and auscultation, the following studies are performed:
- ECG. The dimensions of the right ventricle and atrium, heart rhythm disturbances are determined;
- Phonocardiogram. The presence of systolic murmur is detected;
- Ultrasound of the heart. Signs of compaction of the valve walls, the area of the atrioventricular orifice, and the degree of regurgitation are determined;
- Chest X-ray. The location of the heart and its size, signs of pulmonary hypertension are revealed;
- Catheterization of the heart cavities. The method is based on the introduction of catheters to determine the pressure in the cavities of the heart.
In addition, coronary angiocardiography can be used before surgery. It is based on the introduction of a contrast agent into the vessels and cavities of the heart to assess the movement of blood flow.
Treatment of tricuspid regurgitation
Treatment of the defect can be carried out conservatively or surgically. The surgical method may be indicated already for grade 2 tricuspid regurgitation, if it is accompanied by heart failure or other pathologies. With functional tricuspid regurgitation, the disease that caused the lesion is treated first.
During drug therapy, the following are prescribed: diuretics, vasodilators (drugs that relax the smooth muscles of the walls of blood vessels), potassium preparations, cardiac glycosides. If conservative treatment is ineffective, surgical intervention is prescribed, including plastic surgery or annuloplasty and prosthetics. Plastic surgeries, suture and semicircular annuloplasty are performed in the absence of changes in the valve leaflets and expansion of the fibrous ring to which they are attached. Prosthetics are indicated for tricuspid valve insufficiency and extremely severe changes in its valves; prostheses can be biological or mechanical. Biological prostheses created from animal aortas can function for more than 10 years, then the old valve is replaced with a new one.
With timely treatment of tricuspid regurgitation, the prognosis is favorable. After it is performed, patients must be regularly monitored by a cardiologist and undergo examinations to prevent complications.