The length and quality of a person’s life depends on the health of the heart. The occurrence of malfunctions in the functioning of this organ causes anxiety for most people. Modern medicine has many methods for diagnosing the functioning of the cardiovascular system. They all differ in how they are conducted and how informative they are.
The Holter study is considered one of the most modern diagnostics of cardiac activity and health. Therefore, it is important to find out what cardiac Holter is , when and why monitoring with this device is prescribed.
Holter heart monitoring – what is it?
Holter monitoring is a modern technique for studying the work and condition of the human heart . It received its name in honor of Norman Holter, the founder of this diagnostic method.
What is heart holter? Read more in our article!
The principle of the examination is to conduct an electrocardiogram. Unlike the classical method of carrying out the procedure, data is taken not over a short period, but throughout the whole day. This allows you to see the slightest changes in the functioning of the heart when a person is engaged in normal daily activities.
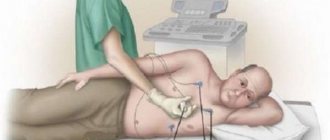
To undergo a Holter study, the patient does not need to stay in the hospital department for a long time . A person is put on a special device, which he wears on his belt - this is what is called a “halter”.
Heart Holter
The total weight of the device reaches about 500 g, so wearing it does not cause much inconvenience.
Recording can be carried out through several channels, up to 12. Most often, 2 or 3 channel research is used.
With the help of a heart holter, you can see how the heart works normally and what changes when performing some loads. Such a study makes it possible to detect changes in rhythm and abnormalities in the functioning of the heart at the initial stages.
In order for the information received to help the attending physician when making a diagnosis, the patient must keep a diary of his affairs. This way you can find out what loads the heart reacted to and to what extent.
How the research is carried out
To carry out daily ECG monitoring, small devices called recorders are used. Using wires, they are attached to 5 - 7 (sometimes more) disposable electrodes, which are glued to certain points on the chest wall. After equipment and instruction, the patient goes home and returns to the functional diagnostic room only the next morning. Information from the device is downloaded to a computer and analyzed by a doctor.
Analysis of a daily record can last up to 2 hours, and sometimes longer. Therefore, you should not expect the doctor to give the result immediately. Typically, patients either wait for several hours or come to the cardiologist the very next day. You should never rush a doctor analyzing a record. Such work requires care, attention and thoughtfulness, and haste here will only harm the patient himself.
Research stages:
Preparation
Depending on the goals of the study, the cardiologist either discontinues some medications or leaves the treatment unchanged for the duration of the study. When canceling, the doctor informs the patient about this, but if desired, you can further clarify which medications can be taken.
It is better to wear loose clothes, take a shower in the morning; for women, a fairly loose bra will be comfortable. Many institutions recommend leaving it on at night to avoid dislodging the electrodes and interfering with the recording. Men need to shave the entire front of their chest. This will not only save them from the painful removal of disposable electrodes, but will primarily eliminate recording noise caused by electrodes rubbing against hair. This will improve the quality of the study.
The recorder runs on batteries or rechargeable batteries. The patient is warned in advance if he needs to bring a battery with him. Often in the test coupon you can see the following designations:
- AA LR 06 – alkaline (alkaline) finger-type battery;
- AA LR 03 – alkaline “pinky” battery.
There is no need to buy salt batteries; their capacity is not enough for a day. It is usually recommended to purchase Duracell or Energizer. They must be new and cannot be taken from a watch or TV remote control.
Patient equipment
The subject undresses from top to waist. Disposable electrodes are glued to the skin of his chest. Many types of electrodes have a glue-free edge for easy removal. This does not mean that the electrode is installed poorly and is about to come off. The electrodes are white synthetic circles with a diameter of 5 cm.
Wires are attached to the electrodes and connected to the recorder. The nurse installs a battery or accumulator in the recorder, and then starts the device. From this moment until the battery is removed, recording continues continuously.
The recorder is placed in a small bag or case, which is hung around the patient’s neck. Do not put the device in your pocket or attach it to your belt. Firstly, it is uncomfortable to sleep, and you can crush an expensive device. Secondly, it may accidentally fall out, for example, when visiting the toilet. It is not recommended to change anything in the equipment yourself. The exception is the case when the electrode accidentally came off. In this case, you need to carefully place it in its original place, additionally securing it with adhesive tape if necessary.
Lifestyle
Once equipped, the nurse will give the patient a diary in which to record events throughout the day. It is imperative to indicate the time when the patient went to bed in the evening (even if he did not fall asleep immediately) and got up in the morning.
Also, depending on the diagnosis and condition of the patient, it is recommended to do 2–3 physical activities. Usually this is climbing stairs at a pace comfortable for the patient until fatigue, or walking quickly in a straight line. There is no need to exercise to the point of exhaustion; the essence of the procedure is to evaluate the work of the heart during the patient’s normal life.
It is not recommended to jump, run, do push-ups, wash the floor, do laundry, remove snow, that is, make any sudden movements, especially with tense hands. This will create noise in the recording. Most likely, the doctor will not be able to analyze this area, and all such work will be done in vain.
Also, you should not sleep on your stomach, as there is a high probability of the electrode coming off. You cannot take a shower, go to the bathhouse, wash your hair, etc., that is, moisturize the device. If the handle of a bag or case rubs your neck, especially in obese people, you can place a small soft towel under it.
During the morning toilet, you can wipe your body with a damp towel without touching the electrodes and the recorder.
The diary should indicate the time at which the patient climbed the stairs or walked on the street, as well as his sensations at this time - palpitations, shortness of breath, interruptions in heart function, and so on. If unpleasant symptoms arose outside of exercise, you must also indicate what exactly happened and at what time. Additionally, you can record the time you took medications and other unusual events related to the work of the heart, but you should not write down a typical day minute by minute.
If the nurse recommended counting the number of steps the patient climbed, this can be done. But in fact, this will not provide reliable information, since it is impossible to take into account the height of the steps, the speed with which the person being studied climbed and other factors.
Possible problems
Daily production monitors are very common in Russia. The manufacturer's name is indicated on the device. Do not be surprised or alarmed if the patient notices the blue light on the device blinking; this is completely normal.
Sometimes Valenta monitors begin to beep loudly, and the message “No CD card” appears on the screen. What to do in this case: take the device out of the bag, open the back cover, remove and insert the battery back, observing the polarity, close the cover. Recording will continue automatically.
Sometimes other recorders also start beeping continuously. This indicates a recording failure. In this case, the easiest way is to remove the battery from the device. It will stop beeping, but the recording will also stop. This study will need to be redone.
If the electrode accidentally comes off, you need to place it in the same place or at least on the chest (not on the stomach or arms, as sometimes happens).
The 24-hour ECG recorder does not give any signals to the patient’s body, does not cause pain, tingling, cannot “electric shock” or otherwise affect the body. With this device you can work at a computer, talk on a mobile phone, walk through frames in stores, and do an ultrasound of internal organs.
Types of Holter monitoring methods
Study of the heart for one day using the Holter technique - monitoring, which can be carried out using several methods:
- full-scale method;
- fragmentary.
To correctly understand what a heart holter is, why it is needed and what it shows, it is worth considering both diagnostic methods in more detail.
Full-Scale Monitoring
The full-scale research technique is used most often. The duration of the procedure ranges from 1-3 days. Thanks to such long-term recording of information, it is possible to obtain reliable information about the functioning of the heart and the causes of failures.
A full-scale Holter study cannot be compared with a classical ECG. With a cardiogram, only 50-60 heartbeats come to the attention of the doctor.
Heart Holter records the dynamics of more than 100,000 beats, which gives a complete picture of the work of the heart. Such information cannot be obtained in any other way.
Fragmented monitoring
The fragmentary diagnostic method is used only during noticeable problems in the heart. The device is worn constantly, however, recording is carried out only when a person experiences pain or feels signs of arrhythmia.
Holter heart study
To start the device you need to press the button. When the discomfort ends, the device turns off.
Sometimes another, more compact device is used for fragmentary research. It also records the time between recordings. It can be worn on the arm, or attached to the chest at the time of pain for the period of recording information.
Carrying out the procedure
In order to obtain valuable and reliable information, it is necessary to correctly attach the electrodes to the chest. The wires coming from them are connected to a small recording device. The recorder itself is small in size and can be attached to a belt. Daily cardiac monitoring should be carried out even during sleep, so the patient must ensure that the device is connected.
Throughout the diagnosis, the patient leads a normal lifestyle, goes to work, and rests. You will also need to keep a diary where the following events that affect the functioning of the heart are recorded:
- Morning awakening time.
- Eating foods that can change your heart rate (coffee, strong tea, chocolate).
- Any physical activity (jogging, climbing stairs).
- Emotional stress.
- Taking medications.
- Bedtime time.
Sometimes doctors specifically prescribe certain actions for the patient, which he must perform and record the time in a diary.
What does Holter heart monitoring show?
A one-time visit to a cardiologist does not always give a complete picture of the functioning of the heart. The behavior of the electrocardiogram may also not show any failures. At the same time, the person continues to experience negative symptoms and pain. The thing is that malfunctions in the heart occur at other moments, when a person is in everyday life and does not have the opportunity to see a doctor.
A Holter cardiac study allows you to evaluate the frequency and pattern of heart contractions throughout the day, including during sleep.
This diagnosis shows whether the heart is well supplied with blood and oxygen, how regular the pulse is and how often contractions occur.
Timely examination makes it possible to detect such diseases in the early stages.:
- arrhythmia;
- IHD;
- angina pectoris;
- hypertension.
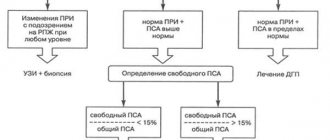
Unlike a classic cardiogram, daily Holter heart monitoring helps the doctor determine the asymptomatic course of coronary artery disease and the exact localization of such an affected area. To correctly interpret the data obtained, the attending physician will analyze the location and displacement of the ST-T segment.
Holter (24-hour) ECG monitoring – complete instructions for the patient
Pulling behind the sternum? Rapid heartbeat or slow pulse? Do you experience a fluttering feeling in your chest? How can a modern method of heart research, Holter ECG monitoring, also known in common parlance as Holter, help in such cases?
To find out this, we visited an appointment with a general practitioner, cardiologist at the Expert Voronezh Clinic, Angelina Anatolyevna Kalinina.
— Angelina Anatolyevna, what is Holter monitoring and why is it prescribed?
Holter ECG monitoring or, in other words, daily monitoring of heart function is a method of electrophysiological instrumental diagnostics that allows continuous recording of an electrocardiogram using a special device.
This method is used in clinical practice in the field of cardiology, therapy to identify disturbances in the rhythm and conductivity of the heart, ischemic changes (especially with contraindications to the so-called “stress tests” - for example, bicycle ergometry), as well as for monitoring and control in the treatment of rhythm disturbances and coronary heart disease.
You can sign up for Holter monitoring here
— What symptoms of the cardiovascular system are an indication for Holter monitoring?
These are spontaneous, inexplicable episodes of loss of consciousness, dizziness, especially without any obvious reason (staying in a stuffy room, excitement, etc.); any sensations of heart rhythm disturbances (rapid or rare pulse; interruptions, “freezing”, “tumbling” in the heart area; shortness of breath, chest pain; night awakenings, especially accompanied by shortness of breath, breathing problems).
A leading neurologist talks about the possible causes and diagnosis of dizziness
"Clinic Expert Kursk" Umerenkova Natalya Vladimirovna
The study is also advisable if the patient or his relatives have a certain heart pathology (including hereditary pathology), and it can be carried out even in the complete absence of complaints. These are diseases such as hypertrophic cardiomyopathy, long QT syndrome, short QT syndrome, and ventricular preexcitation syndromes. Additionally, Holter ECG monitoring can be prescribed to evaluate the performance of an artificial pacemaker after a myocardial infarction.
— Is this diagnosis carried out only for adults? Or do children also undergo a daily ECG?
Of course, Holter monitoring is also used to examine children. Of course, the child’s adequate and conscious behavior is important (following any doctor’s instructions during the study, avoiding unintentional breakdown of the electrodes or damage to the device, etc.). Those. These are organizational and technical aspects. In principle, there are no obstacles to researching children.
— How does Holter monitoring differ from a simple ECG? Why is a regular ECG not enough?
The fundamental difference is the likelihood of detecting some pathological abnormalities. It is incomparably higher during Holter monitoring. It often happens that a doctor, during an objective examination of a patient, clearly records rhythm disturbances, but there is nothing on the ECG. The problem with an ECG in such cases is the short duration of the study and the absence of a person’s usual load (for example, walking). Rhythm disturbances, especially if they are unstable, may not “get” on a regular ECG purely statistically.
Heart, why don't you want peace? What causes tachycardia? Cardiologist says
"Clinic Expert Kursk" Novikova Elena Viktorovna
— Patients often ask questions: what is better: Holter monitoring or cardiac echo, Holter or cardiac ultrasound? Tell us, is there an alternative to the method of daily ECG monitoring?
Holter does not have an alternative that is identical in terms of capabilities. The fact is that echocardiography and Holter monitoring evaluate different aspects related to the structure and function of the heart.
Ultrasound allows you to “see” the structure of the organ, its parts (chambers, valve apparatus), their sizes, the presence of some structural features, functional characteristics associated with the operation of the valves, the movement of blood and the walls of the heart. However, it will not say anything about the type of heart rhythm disturbances, possible myocardial ischemia, which is especially important - outside of a state of rest.
Holter monitoring answers these questions. On the other hand, Holter will not help in any way to evaluate, for example, the valve apparatus, or to determine the presence of defects or blood clots in the cavities of the heart.
When is it prescribed and what will a heart ultrasound show? Read more
Therefore, these studies are not mutually exclusive, but complementary, and to complete the picture, it is recommended to perform both diagnostics.
— Are there any contraindications to Holter monitoring?
There are no such restrictions, rather restrictions. There may be, for example, some difficulties when applying electrodes (severe deformation of the chest, acute inflammatory processes on the skin in this area); mental disorders and corresponding behavior, which may create a risk of incorrect data collection or damage to the device, leading to inaccurate keeping of the research diary; You may be allergic to the adhesive plaster used to secure the electrodes.
— Angelina Anatolyevna, how to properly prepare for a daily ECG?
No special preparation of the patient for daily ECG monitoring is required. If a man has thick hair on his chest, it is recommended to shave it off where the electrodes are applied for optimal contact of the electrodes with the skin.
— How is the Holter monitoring procedure performed?
The person arrives at the appointed time. Several electrodes are placed on his chest, fixed and connected with wires to a portable recording device.
For additional support of the electrodes, a cotton T-shirt or T-shirt is put on top, tightly fitting to the body.
The person is given instructions, including how to keep a diary, and is released for a day. A day later he returns, the device is removed and the data is decrypted.
— Please give an example of how to correctly fill out a Holter monitoring diary?
First of all, it describes what the patient did during the entire study period and his physiological state. The time of sleep, wakefulness, physical exercise, walking, running, eating and taking medications (as agreed with the attending physician, with the name of the drug), driving, emotional stress (even quarrels, etc.) are noted. The exact time of occurrence of complaints is recorded: pain of any localization with its nature (dull, squeezing, stabbing, burning, etc.) and duration; feelings of tightness in the chest; palpitations or rare pulse, “fading” of the heart; episodes of weakness; dizziness, etc. It is very advisable to indicate under what circumstances the complaints appeared (during exercise or at rest, after emotional stress, etc.), how they went away (after stopping the exercise, taking medication, calming down, etc.).
In other words, the more detailed the diary, the more valuable information the doctor will receive.
— Does the patient need to take sick leave during 24-hour monitoring?
No, it is not issued.
— What can and cannot be done under any circumstances while wearing a Holter monitoring device?
The rules for wearing a halter are relatively simple, but at the same time important.
It is possible and advisable to wear a tight-fitting cotton tank top or T-shirt to ensure that the electrodes adhere more closely to the skin.
At night, do not remove the device, choosing a comfortable position in bed.
If the electrode comes off, call your doctor or nurse immediately and wait for further instructions.
Do not wet the electrodes (showering, swimming). It is undesirable to be in an area with electromagnetic radiation (microwave oven, etc.). You should not carry your mobile phone in your pocket or talk on it for a long time.
Otherwise, you can lead your usual lifestyle, with the possible exception of active sports.
— Is it possible to use a computer for Holter monitoring?
This is not desirable, at least not for long.
Other
Holter and ECG of the heart: which is better and what is the difference?
A correct understanding of the essence of the procedure reveals all the advantages of this method of cardiac examination. Even a stress ECG will not provide as much information as Holter monitoring.
The duration of the cardiogram is several minutes. During this period it is impossible to diagnose all ischemic changes in blood vessels, as well as paroxysms of rhythm changes. The doctor will not see pathologies, but negative symptoms will remain.
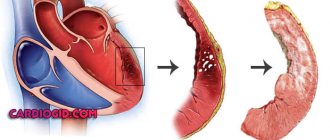
Often, an electrocardiogram is performed immediately after a myocardial infarction. The changes will be obvious. However, an ECG diagnoses a heart attack as a fait accompli. Carrying out a cardiogram shortly before an attack will not provide any prerequisites for effective treatment to prevent the incident.
A Holter study will make it possible to see changes in the coronary vessels in advance and protect the human heart from a dangerous condition.
Heart examination using the Holter method is more effective than an electrocardiogram. If there are problems with the main pump of the body, it is better to conduct a full examination in advance and prevent serious complications.
Indications for ECG according to Holter
A Holter heart examination is prescribed to diagnose the following pathologies:
- asymptomatic ischemia;
- angina pectoris;
- heart attack;
- weakness of the sinus node;
- atrial fibrillation;
- tachycardia;
- intracardiac blockades;
- congenital and acquired heart and valve defects.
This examination is also prescribed for patients already suffering from:
- pathologies of the thyroid gland;
- fainting of unknown etiology;
- high cholesterol;
- shortness of breath;
- severe obesity.
A Holter study of the heart may be recommended to monitor the dynamics of the patient's condition during drug therapy. Diagnostics allows you to determine how effective treatment is and whether adjustments in the choice of drugs or dosage are required.
Experts recommend daily monitoring before planned surgical interventions, especially for people suffering from diabetes. Such an examination is recommended for persons whose activities involve increased danger, for example, pilots or drivers.
It is effective to monitor heart activity using daily monitoring for those who have recently undergone chemotherapy or radiation exposure.
Indications for monitoring
A long-term study of the data recorded by the Holter device made it possible to determine when it is appropriate to use this method. This:
- Patient conditions that presumably indicate arrhythmia (dizziness of unknown etiology, fainting, rapid heartbeat, cardiac dysfunction).
- Detection of ECG changes, often complicated by arrhythmia (myocardial infarction, long QT syndrome).
- Conditions presumably indicating coronary artery disease (chest pain, difficulty breathing, especially after physical activity, psycho-emotional outburst), as well as diagnosis of asymptomatic cardiac ischemia.
- Monitoring the effectiveness of therapy - drug and surgical treatment of arrhythmia and coronary heart disease. Changes are assessed after the use of drugs, ablation of pathways, stenting and bypass surgery of the coronary arteries.
- Monitoring the operation of the pacemaker.
- Monitoring patients at risk of developing arrhythmia or coronary artery disease (with congenital and acquired heart pathologies, after myocardial infarction).
- Arterial hypertension with signs of cardiovascular failure.
- Circulatory failure II-III degree, renal failure.
- Preparation for surgery on the heart and other organs in people with myocardial pathologies.
For more information about the technique and its advantages, watch the video:
How often should research be carried out and why?
There is no strictly defined framework for how often such research is required. Much depends on the disease the person is facing, age and gender.
It is necessary to use this diagnostic method if there are any symptoms of cardiac origin, but the classic electrocardiogram did not provide any information.
A re-examination should always be carried out after a course of treatment.
This will allow you to evaluate its effectiveness and determine whether further therapy is required. Such diagnostics are recommended for all cardiac patients once a year.
Once every 3 years, Holter monitoring is performed for women over 40 and men over 35 to detect coronary heart disease.
How does the device itself work?
The device for Holter monitoring is a registrar (recorder) and electrodes connected to it. A recorder, or monitor, is a small portable device weighing no more than 500 grams (there are devices with a minimum weight of several grams), capable of continuous recording for more than 24 hours.
It is attached to the body using a loop around the neck or a belt. The electrodes are connected to the recorder using wires. The wires must be of sufficient length so that they do not cause discomfort to the patient when turning or tilting the body. The device itself is small in size and is placed in such a way that the patient is comfortable, regardless of whether he is a woman or a man.
Here's what it looks like in the photo:
Sometimes blood pressure monitoring is performed along with an electrocardiogram recording. The recording is carried out in digital form, the information is then transferred to a PC, where the data is interpreted.
Depending on the preliminary diagnosis, the following devices are used:
- 3-channel. They can detect rhythm and conduction disturbances. Myocardial ischemia can be recorded only if it is significantly expressed and also corresponds to the lead in which the readings are taken.
- 12-channel. These are already capable of detecting and displaying minor changes in the electrical activity of the myocardium. Just such a recorder is used to verify coronary heart disease.
Requirements for the patient when conducting Holter monitoring
In order for a Holter study to be as informative as possible, the patient must be willing to cooperate with the medical staff and be able to strictly follow instructions.
The following requirements are imposed on the people being studied:
- keep a diary of activities while recording the device;
- if such a need arises during a Holter heart study, reattach the fallen electrode, which is necessary for successful data recording;
- do not wash while wearing the device;
- do not visit the physical office;
- do not use heating pads;
- do not undergo x-rays;
- Minimize the use of radio devices, including telephones, in everyday life.
If you strictly follow all the recommendations, the doctor will receive all the information necessary for further treatment.
How is the device installed and the examination carried out?
The study does not require any preliminary preparation. It is recommended only on the appointed day to remove all metal jewelry, take a shower and remove hair in the areas where the electrodes are intended to be installed.
Drugs taken to correct blood pressure, antianginal, antiarrhythmic drugs are taken in the same regimen.
Algorithm:
- The patient undresses to the waist. On the anterior surface of the chest, the skin is degreased with 72% alcohol.
- Electrodes (sensors) are attached to prepared areas of the body. To improve electrical conductivity, the sensors are pre-treated with a contact gel. If the study is carried out in the hot season and increased sweating is expected, then it is better to additionally secure the electrodes with adhesive tape.
There are several options for attaching electrodes. It all depends on the type and model of the recorder. Here is an example of their location when recording in three leads:
| Color | Mounting location |
| White | 1st intercostal space at the right edge of the sternum |
| Brown | 1st intercostal space at the left edge of the sternum |
| Blue | 4th intercostal space 1.5 cm outward from the left edge of the sternum |
| Orange | 3rd intercostal space along the left midclavicular line |
| Red | 5th intercostal space 2 cm outward from the left midclavicular line |
| Black | 4th intercostal space at the left edge of the sternum |
| Green | 8th intercostal space along the right midclavicular line |
- The recording device is attached to the belt, hung around the neck using a loop, or directly attached to the body with an adhesive tape. Sometimes carried in a separate bag slung over the shoulder. It all depends on the recorder model.
- To eliminate the possibility of the sensors coming off, wear tight-fitting clothing on top.
- Opening hours may vary. It is carried out both continuously and only when symptoms appear (fragmentarily). In the latter case, the patient turns on the device himself.
Daily monitoring is more often carried out if the purpose of the study is to diagnose heart rhythm disturbances. To verify fainting conditions, it is recommended to monitor for at least three days.
- After installing the device, the signal quality and data recording are checked in various positions, standing, sitting, and while holding your breath. Sometimes a life-threatening arrhythmia, for example, ventricular tachycardia, is immediately detected. Then the person is urgently hospitalized in a cardiology hospital.
- The patient must keep a diary throughout the study. All daily activities are recorded there with a time stamp. Also noted are meals, physical and emotional stress, exercise, rest, sleep both day and night, taking medications, and the like. Any disturbances in the general condition, the appearance of pain, the nature of the pain, and the conditions for relieving symptoms must be recorded.
- The doctor is obliged to instruct the patient in case of unforeseen situations with the device when he needs to turn it off himself.
Methodology for Holter monitoring
Almost all centers perform the Holter study in the same way. The patient will feel more at ease if he knows how the procedure is performed and what awaits him in the doctor's office.
Preparation for the procedure
No special preparation is required. Eating before installing the equipment should be as usual. You only need to exclude alcohol and coffee . It is better to quit or minimize smoking.
How to put Holter on the heart
Depending on the model of the device, disposable electrodes are glued to the patient’s chest. The procedure does not cause pain or discomfort. Lasts 10-15 minutes.
Waiting time for results
The device is worn for 1-3 days, depending on the doctor’s prescription. Then the doctor removes the device and transfers the received data to a computer, where he analyzes the information received.
Holter ECG results. Decoding
The doctor describes the following parameters:
- the presence of arrhythmia and its type;
- the nature of the heart rhythm;
- the largest and smallest pulse;
- reaction of the heart muscle to stress;
- the presence of extrasystoles and tachycardias;
- changes in the blood supply to the myocardium.
Only a specialist can correctly decipher the received data.
The essence of the Holter monitoring technique
The patient should not change his lifestyle during the diagnostic procedure. This allows the doctor to assess changes in cardiac activity during the following periods:
- during sleep, complete rest;
- during physical stress or sports;
- with emotional stress.
Simultaneously with recording ECG readings, it is necessary to keep a diary, which reflects all actions, treatment taken and complaints about well-being.
It is a comprehensive analysis of changes in the cardiogram and the time of their appearance in the patient that can help determine the functional class of angina pectoris, the degree of insufficiency of heart function, identify hidden rhythm and conduction disturbances, and also study resistance to physical activity.
We recommend reading about how an ECG is performed. You will learn about the principles of operation of an electrocardiograph, preparation for an ECG and its conduct, the peculiarities of conducting an ECG for pregnant women, and deciphering ECG indicators. And here is more information about the manifestations and relief of an attack of paroxysmal ventricular tachycardia.