The essence of pathology
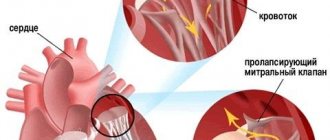
Mitral valve prolapse (MVP) is a lesion of the heart muscle of various origins or a pathology of the connective tissue formations of the heart. Leads to a change in the structure and shape of the mitral valve leaflets (at the moment of systole, they bend into the cavity of the left atrium, allowing some of the blood to flow back).
This pathology in cardiological practice is detected in 15% of children under fifteen years of age. At the same time, cardiac anomalies give rise to MVP in 40% of cases, rheumatism - in more than half of the children examined. Hereditary predisposition guarantees pathology in 100% of cases. Mitral valve prolapse is the main symptom of several congenital syndromes: Ehlers-Danlos, Marfan, contractural arachnodactyly, osteogenesis imperfecta, elastic pseudoxanthoma.
Adults suffer from MVP in 10%. The disease has a gender connotation: women over 40 years of age are more often affected.
Classification of PMC
There is a division of the disease into primary and secondary pathology, as well as according to the severity of prolapse, the degree of reverse blood flow - regurgitation. In practice, both of these classifications are considered together. Mitral valve prolapse can be:
- Primary, genetically determined, with congenital weakness of connective tissue structures. In this case, the mitral valve leaflets are stretched, and the chords that hold them lengthen. As a result, the doors cannot close and a gap remains between them. Congenital pathology does not have a significant effect on the functioning of the circulatory system, but is often accompanied by VSD, arrhythmia, and chest discomfort. Primary prolapse, according to the nature of the heart murmur, is divided into a latent, silent form, which is diagnosed on an echocardiogram, and an auscultatory form with typical noises distinguishable by the ear.
- Secondary or acquired, which develops against the background of somatic diseases, rheumatic, cardiac pathologies. In this case, pain and interruptions in the heart are relieved with medications (Nitroglycerin, Betaloc). If prolapse is caused by injury, chord rupture, emergency medical care is necessary.
Depending on the severity, leaflet prolapse can be:
- first degree – deflection up to 6 mm, with complete closure, so the patient has no symptoms;
- the second – up to 8-9 mm, the leaflets do not fit tightly, regurgitation of varying degrees is observed (backflow of blood into the atrium);
- the third – everything that goes beyond this: the leaflets do not touch, the chords may be torn off, which worsens the patient’s condition, and acute left ventricular failure is formed, requiring emergency intervention.
Moreover, each degree has its own severity of regurgitation - reverse blood flow inside the chambers of the heart (according to Doppler ultrasound):
- first degree - a slight mitral wave of reverse blood flow, which reaches the level of the leaflets;
- the second is moderate regurgitation with a wave rising to the middle of the left atrium;
- the third is a pronounced wave of reverse blood flow, which reaches the opposite end of the left atrium;
- the fourth is severe (described only clinically).
The diagnosis indicates the degree of prolapse and the degree of regurgitation.
Aortic valve regurgitation: features
Many people in everyday life do not encounter the very concept of “regurgitation,” so what is it? Explaining this term, we can say that regurgitation is a physiological phenomenon in which a return of fluid flow occurs. By adding the words “aortic valve” to the term, we conclude that this is nothing more than the reverse movement of blood into the left ventricle due to incomplete closure of the valve.
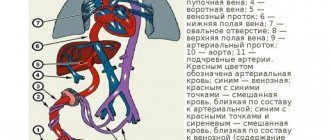
How is everything going? From the atrium, blood enters the left ventricle, which is pushed into the aorta. It is from this large vessel that the enrichment of other organs with essential nutrients and oxygen begins. The movement of blood occurs in one direction; this mechanism of action is controlled by valves. The role of the aortic in this case is to pass blood flow during compression of the ventricle and prevent its reverse ejection. If a violation of the aortic valve insufficiency is detected, the blood flows in reverse when the ventricle relaxes.
Depending on the area of incomplete closure of the valves, as well as the enlargement of the ventricle, the following degrees of damage are distinguished:
- 1st degree - reverse movement of blood occurs by 0.5 cm or less (mild).
- 2nd degree – reverse movement of blood from 0.5 to 1 cm (average).
- Grade 3 – reverse movement of blood by more than 1 cm (severe).
It is these degrees that determine the methods of medical monitoring, the necessary surgical intervention, as well as the risks of other cardiovascular complications.
Causes of the disease
In fact, mitral valve prolapse is not an independent disease. This is a clinical and anatomical syndrome that occurs in various somatic pathologies. Triggers of MVP can be both congenital anomalies and acquired diseases.
In modern cardiology, the main cause of mitral valve prolapse is considered to be a congenital pathology, which is based on myxomatous degeneration of valve structures and intracardiac nerve fibers. This prolapse is also called idiopathic, since the exact etiology of this process has not been established. Most scientists suggest that it is genetic.
Pathological destruction concerns, first of all, the fibrous layer of connective tissue, collagen and elastin, with the accumulation of polysaccharides in the intercellular substance. The connective tissue frame becomes loose, the mitral valve leaflets prolapse at the time of systole. Most often, this affects patients with autoimmune disorders, dysplasia of cartilage, ligaments, congenital defects of joint capsules, arthritis, and arthrosis.
Recent scientific research associates valve prolapse with hormonal disorders of various origins, viral diseases, and streptococcal infections, which cause direct destruction of not only the valves, but also the endocardium of the heart.
Among the secondary (acquired) causes:
- first place is given to rheumatic diseases (up to 80%) - an autoimmune pathology with combined damage to the mitral (prolapse) and aortic (stenosis) valves;
- on the second there is arterial hypertension with left ventricular hypertrophy (up to 10%);
- in the third – infective endocarditis (up to 10%).
Chest injuries, AMI, chord avulsions of various origins occupy an insignificant place (within 2%).
With age, connective tissue and autoimmune degeneration increases, so the risk of deformation of the mitral valve leaflets and damage to the chordae gradually increases and reaches its peak after 40. In adolescence, the cause of pathology is a violation of intracardiac blood flow due to dysplasia and anatomical abnormalities of the coronaries.
Causes of the defect
Based on its origin, mitral valve prolapse is of two types:
- primary;
- secondary.
Primary MVP is caused by genetic defects. And although the gene mutations responsible for the development of the pathology have not yet been precisely determined, there is evidence of the hereditary nature of the disease in the form of frequent cases of prolapse in close relatives.
Therefore, if one of your parents or siblings was diagnosed with MVP, there is a high probability that you have it too.
Primary prolapse is divided into types:
- MVP itself as an independent disease;
- MVP as a manifestation of connective tissue development disorders.
The latter refers to hereditary diseases caused by a defect in the formation of collagen protein. Such diseases include Marfan and Ehlers-Danlos syndromes, as well as common undifferentiated connective tissue dysplasias. In addition to MVP, these pathologies are characterized by different clinical manifestations:
- increased vulnerability and hyperextensibility of the skin;
- frequent subluxations and dislocations;
- hypermobility of joints - a person is able to bend his elbows and knees in the opposite direction, touch his thumb to his forearm, close his palms, placing his hands behind his back;
- chest deformities – keeled, funnel-shaped;
- curvature of the spine - scoliosis, kyphosis;
- flat feet;
- early myopia;
- aneurysms of the interatrial septum and aorta;
- early development of varicose veins of the lower extremities, hemorrhoids;
- diaphragmatic and vertebral hernias;
- frequent nosebleeds;
- prolapse of internal organs - stomach (gastroptosis), intestines (colonoptosis), kidneys (nephroptosis).
Secondary prolapse, as the name suggests, develops against the background of other diseases. MVP occurs due to expansion of the cavities of the heart, stretching of the fibrous ring of the valve, due to wrinkling, inflammation of the valve leaflets or the deposition of calcium salts in them.
Causes of secondary prolapse:
- cardiac ischemia;
- cardiomyopathy;
- myocarditis;
- congenital and acquired heart defects;
- chronic rheumatic heart disease.
Separately, I would like to highlight the “harmless or physiological” MVP, which develops due to the immaturity of the valve itself (fibrous ring, leaflets) and the subvalvular apparatus (tendon filaments or chords and papillary muscles). During ventricular systole, the papillary muscles contract and tighten the chordae, which keep the valve leaflets from sagging.
It often happens that in a growing child’s body, some heart structures develop earlier, while others develop later.
Consequences of this:
- the formation of too long valves or chords;
- large diameter of the fibrous ring;
- insufficient contraction of the papillary muscles.
This can lead to prolapse of the mitral valve leaflets. However, physiological prolapse is called “harmless” for good reason. By the age of 18–20, all structures of the heart have fully matured, and the valve functions as in a healthy person.
What is the danger of PMK
Grade 1 MVP is practically asymptomatic, does not affect the general condition of a person, and does not require any adjustment. But from 5 to 10% of patients face the risk of complications that manifest themselves as the disease progresses, exacerbation of somatic pathologies, and with age. The most dangerous are the following:
- Acute mitral valve insufficiency, which is usually associated with chest trauma, chordae rupture: the patient is diagnosed with acute heart failure, pulmonary edema, and respiratory arrest. The chronic version of mitral regurgitation is mild: weakness, fatigue, shortness of breath.
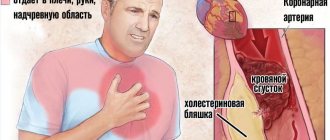
- Infectious endocarditis of various origins is manifested by increased thrombus formation in the vessels of the brain, internal organs, and great vessels with impaired left ventricular function. Risks stroke, heart attack, cardiac arrest, pulmonary embolism.
- Prolapse of the anterior leaflet most often provokes an attack of angina: impaired myocardial contractility increases the load on the left half of the heart, leading to its hypertrophy, hypoxia of the brain, all internal organs and tissues.
- Cardiac fibrillation, MVP with pulmonary congestion, mitral insufficiency can lead to death (ECG shows prolongation of the QT interval).
What diagnosis and treatment is needed?
Having noticed alarming symptoms, a person turns to a therapist or immediately to a cardiologist. At the initial appointment, the specialist collects anamnesis, examines the patient and prescribes the necessary research methods. In this case, the following diagnostics are applicable:
- EchoCG is two-chamber. In this case, the condition of the aorta, the structure of the valve and the functional characteristics of the left ventricle are assessed.
- Doppler study. Using this monitoring, the doctor can evaluate the work of the heart throughout the day.
- Breast X-ray. If there is a violation, the X-ray image will show an enlargement of the heart, as well as the aortic root.
- EchoCG. Allows you to identify the severity of the disease in order to get a definite picture of its course.
- Coronography. It is used extremely rarely, because this type of research is necessary before the actual operation.
If grade 1 aortic valve regurgitation is detected, the doctor gives recommendations on maintaining a healthy lifestyle.
Symptoms
Clinical manifestations of mitral valve prolapse depend on the degree of dysplasia of the connective tissue of the heart, the presence of vegetative-vascular, and neurological disorders. Signs of the disease that you should pay attention to in newborns include:
- asthenic body type;
- hip dysplasia;
- umbilical, inguinal hernias;
- malnutrition;
- the ability of joints to bend in all directions, including those that are anatomically unusual for them;
- varicocele;
- chest deformity.
Later, MVP manifests itself as flat feet, myopia, strabismus, nephroptosis, incorrect posture, frequent acute respiratory viral infections or acute respiratory infections, and sore throats. In adolescents, MVP is associated with vegetative-vascular dystonia.
The main clinical symptoms of mitral valve prolapse in adults are:
Vegetative-cardiac syndrome: pain behind the sternum due to emotional or physical stress, hypothermia, reminiscent of angina pectoris. Sometimes heart pain is spontaneous and can be relieved with nitrates (up to 98% of all cases).
- Arrhythmia, tachycardia (up to 80% of cases), associated with excitement, drinking strong tea, coffee, and lifting weights. They do not pose a threat to life.
- Hyperventilation syndrome resulting from dysregulation of breathing. Headache, often of the migraine type (more than half of the cases).
- Panic attacks of a non-epileptic nature occur spontaneously and do not have an exact cause.
- Depression.
- Asthenia.
- Syncope (short-term loss of consciousness) with muscle atony.
- Impaired thermoregulation.
- Dyspnea that does not correlate with heart failure.
Auscultation with MVP determines:
- isolated clicks in the left ventricle during mid or late systole (single or multiple);
- late systolic, glosystolic murmurs due to a large difference in pressure in the atrium and ventricle;
- a combination of clicks and noises.
With instrumental and laboratory examination, mitral valve prolapse gives:
- asymptomatic prolongation of the QT interval on the ECG is a marker of the development of life-threatening arrhythmia;
- high excretion of catecholamines (peak during the day, decrease at night).
Clinical severity
Before talking about possible symptoms, it is necessary to highlight the forms of its occurrence. Regurgitation occurs in the following stages of manifestation:
- acute;
- chronic.
In the acute form, symptoms may resemble those of heart failure, namely:
- the appearance of severe weakness;
- pale skin;
- decreased blood pressure;
- increasing shortness of breath.
The chronic course of this pathological disorder may not bother a person for years and not let him “know about himself.” With progression and transition to another degree of severity, the following clinical severity can be noted:
- the appearance of shortness of breath even with minor physical exercise and exertion; sudden shortness of breath at night is also a characteristic feature;
- increased heart rate;
- the appearance of pain in the chest in the area of the heart;
- systematically recurring migraine;
- sudden weight loss;
- in some cases, increased body temperature;
- dysfunctional phenomena of the left ventricle;
- headaches and dizziness.
Diagnostics
Diagnosis of mitral valve prolapse is subject to the standard algorithm for examining a heart patient:
- medical history, physical examination with stress tests (squats, holding your breath, walking in place);
- OBC, OAM, biochemistry – screening of the patient’s general condition.
- ECG, EchoCG - detect arrhythmia, the presence of regurgitation, determine the degree of MVP;
- Holter;
- radiography - determines mitral insufficiency by regurgitation;
- phonocardiography – confirms auscultatory murmurs;
- Dopplerography.
Sometimes consultation with specialists may be required. In children, MVP can be heard as a third tone, but this has no diagnostic significance. Mitral valve prolapse detected in a child may disappear on its own with age.
Symptoms of MVP
The first and second degrees of MVP are most often asymptomatic and the disease is discovered by chance when a person undergoes a mandatory medical examination. In grade 3, the following symptoms of mitral valve prolapse are noted:
- Weakness and malaise appear, low-grade fever (37-37.5°C) persists for a long time;
- There is increased sweating;
- Headache in the morning and at night;
- There is a feeling that there is nothing to breathe and the person instinctively tries to absorb as much air as possible, taking a deep breath;
- Emerging pain in the heart is not relieved by cardiac glycosides;
- A stable arrhythmia develops;
During auscultation, heart murmurs are clearly audible (mid-systolic clicks caused by high tension of the chords, which were previously greatly relaxed). They are also called slamming valve syndrome.
When performing a heart ultrasound with Doppler, it is possible to detect reverse blood flow (regurgitation). MVP does not have characteristic ECG signs.
Video: MVP on ultrasound
Features of treatment
Treatment of MVP depends on the severity of the pathology. Grade 1 mitral valve prolapse does not require any special treatment. There are no restrictions on physical activity. Any kind of sport is possible, with the exception of weightlifting and strength training equipment. The patient is not even exempt from the army.
The main treatment for stage 1 MVP is a healthy lifestyle, infection prevention, medical examination. But sometimes doctors decide to replace the mitral valve already at this stage of the disease. This happens if the cause of the pathology is autoimmune processes in the body, which will certainly progress and create a risk of fatal complications. The satisfactory condition of the patient at a given period of time allows us to predict a good effect from the operation and the absence of negative consequences. Delaying surgical intervention can lead to the impossibility of performing it even for health reasons.
Grade 2 MVP is accompanied by negative symptoms and requires not only constant monitoring of the patient, but also symptomatic drug treatment: the presence of signs of circulatory failure, arrhythmias, and syncope. The treatment regimen is strictly individual and is the exclusive prerogative of the doctor. Physical activity is not prohibited, but the type and dosage is selected by the doctor. There is no exemption from the army, with the exception of grade 2 MV prolapse with regurgitation above grade 2 or in the presence of arrhythmia, cardiac conduction disturbance. You can play sports if you lack:
- syncopation;
- no arrhythmia (24-hour monitoring);
- there is no regurgitation (Doppler sonography);
- the contractility of the heart is preserved (EchoCG);
- there was no history of thromboembolism. all indicators of the coagulation system are normal;
- no one in the family died from sudden cardiac arrest due to MVP.
To prevent the progression of pathology, it is recommended:
- sedatives: tincture of motherwort, valerian, hawthorn, Novopassit, Persen;
- mitral insufficiency or arrhythmia suggest the prescription of beta-blockers (Diltiazem, Sotahexal, Bisoprolol, Adenosine, Propanorm, Allapinin, Amiodarone), anticoagulants (Cardiomagnyl, Warfarin, Finilin, Girygen, Girylog, Argatroban), which relieve chest discomfort, rapid heartbeat, and anxiety.
Physiotherapeutic procedures (electrophoresis with bromine, magnesium on the collar area), massage, balneotherapy, hirudotherapy, acupuncture, acupuncture are indicated for MVP. Surgical intervention is used for the same indications to correct the valve or replace it. When planning minor surgical interventions, preventive antibiotic therapy is mandatory (tooth extraction, polyps in the maxillary sinuses, tonsils); courses of preventive antibiotic therapy are indicated.
Grade 3 MVP is characterized by serious structural disorders in the heart, which cause MV failure, persistent arrhythmia: expansion of the left atrium cavity, thickening of the walls of the ventricle, disturbances in the functioning of the circulatory system. This degree of pathology requires surgical correction of the valve, its suturing or prosthetics. Instead of physical education and sports, special gymnastic exercises and exercise therapy are recommended, and healthy, sound sleep is necessary.
Symptomatic treatment consists of using:
- vitamins of group B, PP, E, C;
- tachycardia is stopped by Betalok, Atenolol, Propranolol, which improve the nutrition of collagen fibers;
- vegetative-vascular dystonia is treated with adaptogens (Eleutherococcus, Schisandra, ginseng), vitamin and mineral complexes (Magne B6, Magnelis B6, Vitrum, DoppelHertz, Pikovit).
They use psychotherapy sessions (group and individual) to relieve emotional stress. Tobacco, alcohol, heavy lifting, and strength training are prohibited.
Treatment
In most cases, MVP is not accompanied by significant disturbances in the functioning of the heart and does not require special therapy. Such patients should be observed by a cardiologist and follow his recommendations on maintaining a healthy lifestyle. Patients are recommended:
- once every 1-2 years, conduct an Echo-CG to determine the dynamics of MVP;
- carefully monitor oral hygiene and visit the dentist once every six months;
- stop smoking;
- limit the consumption of caffeine-containing products and alcoholic beverages;
- give yourself adequate physical activity.
The need to prescribe medications for MVP is determined individually. After assessing the results of diagnostic studies, the doctor may prescribe:
- magnesium-based preparations: Magvit, Magnelis, Magnerot, Cormagensin, etc.;
- vitamins: Thiamine, Nicotinamide, Riboflavin, etc.;
- adrenergic blockers: Propranolol, Atenolol, Metoprolol, Celiprolol;
- cardioprotectors: Carnitine, Panangin, Coenzyme Q-10.
In some cases, patients with MVP may need to consult a psychotherapist to develop an adequate attitude towards treatment and the condition. The patient may be recommended:
- tranquilizers: Amitriptyline, Azafen, Seduxen, Uxepam, Grandaxin;
- neuroleptics: Sonapax, Triftazin.
If severe mitral regurgitation develops, the patient may be recommended surgery to replace the valve.
Prolapse in pregnant women
Quite often, mitral valve prolapse is diagnosed in pregnant women during a complete mandatory examination. The first degree is usually not a concern. The pregnancy is proceeding normally, there are no negative consequences for the fetus. Moreover, prolapse can decrease during pregnancy: cardiac output increases, capillary resistance in the periphery decreases. Arrhythmias are possible, but childbirth occurs naturally and normally.
The addition of regurgitation or the transition of pathology to the second degree requires constant monitoring of the expectant mother by a cardiologist. Medicines are used only for health reasons (serious hemodynamic disturbances).
The rules of behavior for a pregnant woman with mitral valve prolapse are simple:
- avoid hypothermia and sudden temperature changes;
- move more to prevent congestion in the pelvic organs;
- rest in a reclining position.
Forecast
How MVP will behave during life depends on the reason that caused it:
- hypertensive prolapse depends on the degree of heart failure, the risk of AMI, stroke;
- rheumatic MVP can exist asymptomatically for decades, requiring preventive courses of drug therapy, and sometimes surgery;
- infective endocarditis is completely cured if the pathogen is accurately identified, treatment is long-term, and the prognosis is favorable (with the exception of drug addicts).
Uncomplicated mitral valve prolapse has a good prognosis.
How dangerous is the disease?
Common complications include cardiac problems. Basically, these are fatal abnormalities that cannot be treated in isolation.
- Heart attack. The most likely outcome. Characterized by acute circulatory disorders in muscle formations. Hence the intense clinical picture.
- Caridiogenic shock. A drop in blood pressure combined with a significant decrease in left ventricular output. A deadly complication. Mortality rate is almost 100%. Even lucky patients do not manage to live too long; within a few years, death is inevitable.
- Stroke. Acute malnutrition of the brain. It is dangerous not only in terms of mortality, but also in the likelihood of focal-type deficiency phenomena (speech, vision, hearing suffer first of all).
- Heart failure.
- Vascular dementia. It occurs relatively rarely against the background of the pathology under consideration.
Mitral valve prolapse is dangerous due to hemodynamic disturbances and threatens generalized hypoxia of all tissues and organs. Long-term course is associated with multiple failures.
Literature
- A.I. Abdrakhmanova, I.V. Abdulyanov. Mitral valve prolapse in a doctor’s practice. // Kazan State Medical Academy, 2020.
- Kuzhel D.A., Matyushin G.V., Savchenko E.A. Diagnosis and treatment of mitral valve prolapse // Rational Pharmacotherapy in Cardiology, 2010.
- Amelina T.N., Tashchuk V.K., Turubarova-Leunova N.A. Current aspects of mitral valve prolapse in athletes // Scientific notes of the University named after P.F. Lesgafta, 2013.
- Dzemeshkevich S.L., Stevenson L.W. Mitral valve diseases. Function, diagnosis, treatment. - M.: GEOTAR Medicine, 2000.
- Movshovich B.L., Lisitsa D.N. Management of patients with mitral valve prolapse in the clinic // Attending physician, No. 5, 2001.
Website editors
A team of authors with higher and secondary medical education, many years of experience in practical medicine, highly specialized specialists and general practitioners.
All articles by the author