An ECG during pregnancy is different from a cardiogram in a non-pregnant woman. This is due to developing changes in hemodynamics, electrolyte composition and hormonal changes. This must be taken into account when interpreting the result - what is normal outside pregnancy, during pregnancy can be a sign of pathology, and vice versa. This research method makes it possible to identify various abnormalities in the functioning of the heart, therefore it is widely used in obstetrics. But the ECG result must be interpreted by a specialist who has the appropriate specialization.
Historical reference! The ECG during pregnancy was first performed in 1913. The electrocardiography method itself dates back to the mid-19th century, when it was noticed that the heart generates a certain amount of electricity.
Changes in the cardiovascular system affecting ECG in pregnant women
Pregnancy is stressful for the heart and circulatory system. During pregnancy, the volume of blood in the vascular bed increases by 30–50%, this provides nutrients to the growing baby. The amount of blood pumped by the heart every minute also increases by 30–50%. In addition, the heart rate increases. All these changes make the heart work harder.
Pregnancy also affects the size of the heart and its position in the chest. The enlarged uterus puts pressure on the diaphragm, which moves upward and changes the position of the heart. Its size increases during pregnancy by approximately 12%.
These changes in the size and position of the heart, and its harder work, can lead to the characteristic ECG appearance during pregnancy.
Description of electrocardiography
During contraction, the heart generates electrical impulses that are detected using an electrocardiograph.
The first electrocardiogram was recorded by French physicist Gabriel Lippmann, who used a mercury electrometer. Later, the Dutch physiologist Willem Einthoven created a string galvanometer and was the first to determine the values of ECG waves.
When examining healthy hearts, the ECG has certain characteristics. If the ECG is abnormal, it may indicate a heart problem. Your doctor may recommend an ECG to help determine your risk of developing heart disease. This is especially true in cases where there is a hereditary predisposition to heart disease or another risk factor (smoking, excess weight, diabetes, high cholesterol or high blood pressure).
Your doctor may also recommend an ECG if you experience adverse symptoms such as chest pain, shortness of breath, dizziness, fainting, or fast or irregular heartbeat.
An ECG is a safe and non-invasive procedure without any significant risks or side effects for the health of the pregnant woman and child.
ECG procedure
There is no need to restrict yourself from eating or drinking before the test. It’s another matter when you are taking any medications and you should always let your doctor know about this. You should also be notified of any allergic reactions to adhesive tapes and substances that are often used to attach electrodes.
Before the test, you will need to remove your outer clothing so that the electrodes can be attached to your chest and limbs. (For women, wearing a separate top with trousers or a skirt can provide easy access to the chest). In some cases, it is even recommended to remove your bra so that the doctor can properly apply the electrodes.
Suction cups or sticky gel are used to attach electrodes to the chest, arms and legs. Using installed sensors, electrical currents generated by the heart are detected - they are measured and recorded by an electrocardiograph.
Three main types of ECG:
- Standard ECG - indicators are taken in a calm state, when the woman lies on the couch and the doctor records the ECG for 1-2 minutes. During the procedure, movement is not allowed, since electrical impulses generated by other muscles can interfere with those created in the heart. This type of ECG usually takes 5 to 10 minutes.
- Ambulatory ECG - It is sometimes recommended to wear a portable recording device for at least 24 hours. This type of diagnosis is also called Holter monitoring. During the study, you can move freely and lead a normal lifestyle, while the connected monitor records the electrical activity of the heart. This type of ECG is suitable in cases where intermittent symptoms are detected that do not appear during a quiet ECG recording. Additionally, you need to record your symptoms in a diary and note when they occur, so that you can then compare them with an ECG
- Stress test (stress study) - this diagnostic method is used to record an ECG while riding an exercise bike or walking on a treadmill. This type of ECG takes 15 to 30 minutes to complete.
- Fetal ECG (CTG, cardiotocography) - performed in the third trimester of pregnancy, most often in preparation for childbirth. Shows fetal activity and heart rate. If the study is done during childbirth, then the frequency of contractions.
When the procedure is completed, all electrodes are removed. An ECG is completely painless and non-invasive, since the skin is not injured in any way.
The doctor can interpret the ECG results based on the medical history, symptoms and clinical condition immediately after the examination, or the conclusion is transmitted with the pregnant woman’s card a little later. As a rule, the conclusion indicates the heart rate (HR), the position of the electrical axis of the heart (right, left, normal), the correctness or deviations of the heart rhythm.
As an example, the following ECG conclusion (normal variant) can be given: Regular sinus rhythm, heart rate 85 beats/min, normal EOS.
Possible ECG complications
An ECG is a safe procedure with no known risks. The device does not transmit electrical current to the chest. Some people may have an allergy or sensitivity to the electrodes, which may result in redness of the skin, so any known reactions such as these should be reported to your physician prior to the procedure.
After the ECG there is no need to follow any regimens. The ECG is non-invasive and does not involve the use of medications (such as anesthetics), so there is no recovery time.
The ECG results allow the doctor to determine whether special treatment is needed or not.
Some of the different heart conditions that can be diagnosed using an ECG include:
- Cardiovascular heart defects associated with the conduction (electrical) system.
- Abnormal rhythm (arrhythmias)—fast, slow, or irregular heartbeat.
- Damage to the heart, for example when one of the heart arteries is blocked (coronary occlusion), resulting in poor blood supply to the heart.
- Inflammation - pericarditis or myocarditis.
- Monitor for cardiac abnormalities due to abnormal chemical reactions (electrolyte imbalances) that control cardiac activity.
- Previous heart attacks.
A woman with heart disease may have a normal ECG result if it does not cause problems with the heart's electrical activity. In such cases, other diagnostic methods may be recommended, especially if cardiac pathology is suspected.
Preparing to take a cardiogram
In order for the test to pass as quickly and efficiently as possible, the following tips may be useful:
- Tell your doctor about all the medications you are taking, as many of them may affect the test results.
- Instead, wear clothes that are easy to take off or unbutton at the chest.
- On the day before the test, no creams should be applied to the skin, as they affect electrical conductivity.
- Remove all jewelry from your neck and arms in advance.
- Ask your doctor any questions you have about this test, its risks, and its results.
No special preparation is needed to record an ECG. Immediately before the test, you should avoid physical activity and do not drink cold water.
Consequences of sinus arrhythmia for mother and baby
If we are talking about physiological arrhythmia, then there will be no consequences. In this case, arrhythmia is only a way for the expectant mother’s body to adapt to the load without harm to the fetus and her own health.
If the doctor reveals abnormalities in you during an in-depth examination, the consequences can be much more serious. Potentially dangerous rhythm disturbances are an indication for caesarean section with all the attendant complications. In addition, even during pregnancy, a woman is prescribed antiarrhythmic medications, which also affect the functioning of the fetal heart. After birth, such a child requires increased attention from a pediatric cardiologist.
He is monitored for slowing or accelerating heart rate, and changes in the electrocardiogram are monitored throughout the year.
How is the examination carried out?
Typically, an ECG during pregnancy is carried out in a medical institution - a clinic, outpatient clinic, hospital. Since the machine itself that records the cardiogram is portable, this test can be performed almost anywhere.
During the examination:
- You will have to lie down on a couch or bed, exposing the chest, forearm and lower leg area.
- The healthcare professional applies a special gel to the skin of these areas that reduces electrical resistance.
- Electrodes are attached to the skin of the arms, legs and chest, which are connected to a machine that records the electrical activity of the heart on paper.
- During the test, you need to lie still and breathe normally. Sometimes your healthcare provider may ask you to take a deep breath and hold your breath. You cannot speak during the examination.
- You need to relax and not tremble, as any movement can affect the result.
- After recording is completed, the electrodes are removed from the skin and the gel is wiped off.
The duration of ECG recording rarely exceeds 10 minutes. After this, the electrodes are removed from the skin.
In what cases is CTG performed?
Cardiotocography is used for early diagnosis of fetal pathologies. Indications for CTG may include:
- Mother's illness. This applies, in particular, to infectious and viral diseases. And the presence of a chronic infection makes the procedure necessary.
- Typically, monitoring of pregnant women includes one mandatory CTG (at 28-30 weeks). If the patient has no complaints, then a repeat procedure is not prescribed.
- Detected pathologies of fetal development.
- Unfavorable course of the previous pregnancy. Even if now carrying a child proceeds without complications, the presence of unfavorable circumstances of a previous pregnancy is an indicator for CTG. The doctor may prescribe repeated examinations. Indications include: the birth of a stillborn child, abnormalities in the development of the child’s organs, as well as genetic abnormalities.
- Disturbed child behavior. The expectant mother knows and feels how the child in her womb behaves and should behave. In particular, this applies to the regime of alertness and sleep. It happens that the fetus is characterized by high activity and short periods of rest. It also happens that the child sleeps mostly during the day, but at night, on the contrary, is active. Any persistent changes in the baby’s usual rhythm of life may indicate the presence of some discomfort.
- Transferred treatment of the unborn child. In this case, CTG data is recorded for several weeks after therapy.
- Late toxicosis (preeclampsia) in a pregnant woman. This condition significantly impairs the blood supply to the fetus. Lack of sufficient blood supply can lead to delays in the child's development.
- Consumption of alcohol, tobacco, and drugs by pregnant women. The presence of chronic addiction (even if the woman is in the recovery stage) requires mandatory cardiotocography.
- The presence of chronic diseases of internal organs. These primarily include diabetes mellitus, obesity, heart defects, and high blood pressure.
- Post-term fetus.
CTG and ECG are very important procedures during pregnancy. It is on the basis of these studies that the further course of the process of bearing a child is predicted.
Diseases that can be detected using an ECG
Registration of an ECG during pregnancy helps diagnose many heart diseases in expectant mothers. With this test, doctors can detect:
- fast or slow heartbeat;
- heart rhythm disturbances (arrhythmias);
- disturbances in the passage of electrical impulses in the heart (blockade);
- an increase in the size of the heart and thickening of its walls (hypertrophy);
- the cause of heart disease symptoms (eg, shortness of breath, heart pain, dizziness, fainting);
- signs of congenital heart defects in a pregnant woman;
- signs of electrolyte disturbances (increased or decreased levels of potassium, magnesium, calcium in the blood).
ECG during pregnancy: interpretation of indicators
Electrocardiography (cardiogram, ECG) is an additional research method that allows you to evaluate the functioning of the electrical conduction system of the heart. The study takes no more than 5-10 minutes and has a minimum number of contraindications.
To conduct an ECG, a special medical device is used, which, by placing sensors on the chest, arms and legs, records the electrical activity of the heart and displays the results on paper in graphical form or on a digital monitor.
During pregnancy, all women who register with the antenatal clinic are given an ECG twice. The first time is after the initial examination, which allows for a general assessment of the heart function of the pregnant woman. The second time was before taking maternity leave. If necessary, if there are symptoms of heart disease, an ECG can be prescribed at any time.
Video: Decoding the cardiogram: norm and pathology
ECG procedure
Effect of ECG on the fetus
An important question for an expectant mother is: “is it possible to do an ECG during pregnancy?” and “what impact does it have on the baby?”
It is known that ECG is harmful to the child and is strictly prohibited for pregnant women. However, this judgment has been refuted by doctors - a cardiogram is recognized as a safe, painless procedure and cannot have a detrimental effect on the developing embryo.
The impulses are not reflected negatively on the placenta, organs and tissues, or on the milk of the expectant mother.
The procedure has no contraindications.
It is known that ECG is harmful to the child and is strictly prohibited for pregnant women. However, this judgment has been refuted by doctors - a cardiogram is recognized as a safe, painless procedure and cannot have a detrimental effect on the developing embryo.
Holter monitoring
The recording of an ECG examination lasts minutes, this is not enough, especially in unstable forms of rhythm disturbance, then Holter monitoring is done. This is essentially an ECG, only the recording is extended by 24-48 hours. This is also a completely harmless examination.
A Holter ECG during pregnancy is performed using a small device that is attached to the body. The Holter monitor constantly captures and records all electrical phenomena that occur as a result of the work of the heart. At the end of the examination, all data is decrypted and given to the patient in the form of a printout. This is a wealth of factual material necessary for a doctor to resolve the issue of further management of the patient.
Pregnancy is an important and very difficult stage in the life of any woman. In order for it to go as calmly as possible and end with the birth of a healthy child, the woman needs to follow all the doctors’ orders and undergo all the necessary examinations during the tests. And the most important thing is to know that all examinations permitted during pregnancy cannot in any way harm her or her unborn child, and among them, the simplest and safest ECG examination.
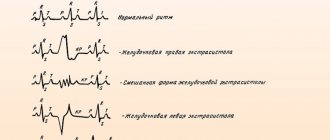
All these forms of arrhythmias are detected using a very simple and completely harmless ECG examination.
Significance of the procedure
A study using a cardiotocograph is of high importance in assessing the condition of the fetus. Along with procedures such as ultrasound, Doppler, in-depth electrocardiography, it allows you to promptly suspect abnormalities in the baby’s cardiovascular activity and take measures to correct them.
During multiple pregnancies, when it is not possible to evaluate the heart function of each baby using a stethoscope, CTG is the only correct way to assess their condition.
If a woman is carrying identical twins, using a stethoscope to evaluate heart function is unacceptable, as the results obtained will be false.
Childbirth is also not complete without CTG. With its help, the doctor assesses the condition of the fetus during contractions and between them, determines the most suitable period for inducing labor, if necessary, and calculates the dosage of drugs.
A study using a cardiotocograph is of high importance in assessing the condition of the fetus. Along with procedures such as ultrasound, Doppler, in-depth electrocardiography, it allows you to promptly suspect abnormalities in the baby’s cardiovascular activity and take measures to correct them.
How does an electrocardiograph work?
An electrocardiograph records cardiac electrical potentials. The cardiogram is recorded using electrodes attached to the body of the subject. The main components of this device include:
- system responsible for increasing heart rate;
- galvanometer;
- registrar;
- switch.
The electrocardiograph receives a weak electrical impulse from the heart muscle, which occurs in the patient. Next, it is sensed by the electrodes, after which it is amplified and captured by a galvanometer. Any change in the electromagnetic field is recorded and then recorded by recorders on a paper tape that moves evenly.
The result is a kind of graph displaying the work of the cardiac departments. It is expressed in teeth of different sizes. The length of the graph depends on how strong the signal comes from a particular department. The electrocardiograph does not interfere with the functioning of the body, it simply records the work of the heart.
In addition, this device does not emit ionizing radiation, which is observed in computer tomographs, radiographic units, and does not generate magnetic fields, like a magnetic resonance tomograph. The operation of this device is based on recording electrical potentials created by the heart muscle and producing a cardiogram, which is deciphered by specialists.
Heart rhythm disturbances during pregnancy are felt much more strongly. Experts associate them with the excessive susceptibility of the expectant mother. However, if you feel:
Content:
- Carrying out the procedure and its safety
- Indications for an ECG during pregnancy
- The main parameters determined on the ECG
Electrocardiography (ECG) is a method of determining the electrical activity of the heart and recording it on film. Using this study, we can determine how our heart works. A special device - an electrocardiograph - records the total potential difference of all heart cells between two points, that is, in a certain lead, and writes it down on paper. The doctor, examining the electrocardiogram, evaluates the rhythm and frequency of the heartbeat, the location of the heart, and the speed of the electrical impulse. That is, an ECG can detect various arrhythmias, blockades and dysfunction of the heart muscle.
During pregnancy, a woman's heart works under increased load due to an increase in the volume of circulating blood. The level of hormones in the body that affect the functioning of the cardiovascular system also changes. Therefore, it is very important to find out possible disturbances in the functioning of the heart at the beginning of pregnancy in order to carry out the necessary treatment in time and prevent the development of complications.
If necessary, a cardiologist can prescribe an ECG recording using additional leads
:
Preparing for electrocardiography
To achieve the maximum effect from this procedure, you should tell your specialist about the medications you are taking. Their action may affect the test results. On the day of the session, do not use cream, as it affects electrical conductivity. First get rid of jewelry: chains and bracelets.
No special preparations are required for the test. On this day you need to eat one to two hours before the procedure. Immediately before the ECG, it is better to refrain from physical activity and not drink cold water.
An ECG is designed to record signals arising from the work of the heart, without any interference in the body. Electrocardiography is a fairly harmless method; it does not pose any danger to a pregnant woman and her baby. During the entire period of using this procedure, not a single case of its negative impact on the human body has been recorded. There may only be some inconvenience when removing the electrodes and, in rare cases, a slight rash may appear at the site of their installation.
Features of the procedure
For ECG interpretation, the speed of the tape in the device is of great importance. Typically it is set to 50 mm/second. However, it can be 2 times more or less. Electrodes are installed on the body of a pregnant woman in the appropriate places - there are 6 standard leads, but in some cases additional leads can be used. The latter allow you to detail previously obtained information.
To obtain the most accurate ECG, a special gel must be applied to the electrodes. It improves the conductivity of the electrical impulse from the heart to the device, since the air gap that is created between the body and the sensors is not conductive and dampens the signal.
To obtain the most accurate ECG, a special gel must be applied to the electrodes. It improves the conductivity of the electrical impulse from the heart to the device, since the air gap that is created between the body and the sensors is not conductive and dampens the signal.
Processing ECG results
Interpretation of a cardiogram recording requires quite a lot of experience from the doctor. The results of the examination will be known on the day of its conduct; decoding usually takes no more than 10–15 minutes.
In his conclusion, the doctor indicates the nature of the heart rhythm, the frequency of heart contractions, the electrical axis of the heart (characteristics of the position of the heart), and describes existing disturbances in electrical conductivity (if any). Diagnosis is not made solely on the basis of a cardiogram; symptoms and signs of the disease are also taken into account.
Arrhythmia during pregnancy
Pregnancy is a time of global physiological changes in the body of women. Each system increases performance to meet the needs of mother and fetus. The course of this process shows how prepared the female body is for motherhood. Arrhythmia during pregnancy can occur due to disturbances in the functioning of the neuromuscular system, water and electrolyte balance, and hormonal levels. If pathology occurs, careful diagnostics will be required to make a diagnosis.
Development of blockade in pregnant women
Normally, impulses from the pacemaker are carried along nerve fibers. However, some inflammatory diseases and foci of necrosis can disrupt coherent regulation. As a result, blockades develop. Pathologies of II–III degree of severity, which cause dizziness and loss of consciousness, are of clinical significance.
In order to restore normal rhythm in women, a pacemaker is installed. This will protect the life of the mother and the unborn baby. In such cases, natural childbirth will be contraindicated; delivery is carried out only by cesarean section.
The characteristics of a pregnant woman’s body can cause certain difficulties with the dosage of medications. Therefore, if arrhythmia occurs, inpatient treatment is indicated. This will allow you to observe the body’s reaction to the drugs used and monitor the ECG pattern.
Features of a cardiogram in pregnant women
Changes in the cardiovascular system characteristic of pregnancy change the character of the cardiogram, especially in the later stages.
ECG of pregnant women is characterized by:
- Increased heart rate.
- Shift of the electrical axis to the left.
- Shortening the PR interval.
- Negative T wave in leads III, V
- Pathological Q wave in leads III, aVF.
It should be remembered that all these characteristic features of the ECG during pregnancy are not observed in all women.
How is the research conducted?
Carrying out electrogradiography
Carrying out an ECG in women during pregnancy is no different from doing it in other patients. The examination is carried out in the supine position, the procedure is absolutely painless. Before the procedure, the woman should not exercise; it is recommended to avoid eating, smoking, and caffeine-containing drinks 1-2 hours before the procedure. General fatigue, a full stomach, and harmful addictions can distort the results of the examination.
A pregnant woman's clothing should be loose so that she can easily expose her chest, hands and ankles - the places where the electrodes are attached. During the ECG, the woman must be absolutely calm, breathe freely and evenly. If a health worker notices a pregnant woman’s anxiety before the procedure, he is obliged to calm her down and explain that the manipulation is completely safe and can be performed repeatedly at any stage of pregnancy without any negative consequences on the fetus.
After an ECG, a woman should avoid sudden rises from the couch, since in late pregnancy, too rapid a transition from a horizontal to a vertical position can cause orthostatic hypotension and even fainting.
Limitations of ECG
Like many diagnostic methods, ECG has certain disadvantages and limitations:
- This is a static method and may not reflect existing heart problems if there are no symptoms at the time of recording.
- Many pathological changes on the cardiogram can be nonspecific, that is, observed in various diseases. To clarify the diagnosis in such cases, additional examinations are carried out.
- In some heart diseases, the cardiogram may be completely normal.
What is sinus arrhythmia and what are its types?
From an anatomical point of view, all rhythm disturbances are divided according to the location of the conduction system of the heart where the failure occurred. If we conventionally imagine the heart as a system of wires intertwined with each other in certain places, we can easily explain this principle of division. So, the most important node, where all the wires begin, is called the sinus node. Normally, electrical currents come from here - it is with the help of them that the heart contracts, each contraction of this powerful muscle pump is stimulated by electricity. If impulses come from this node, but with the wrong frequency, then the arrhythmia is called sinus. This is the “safest” of all types of arrhythmias.
Sinus arrhythmias are divided into:
sick sinus syndrome, sinus node dysfunction;
respiratory sinus arrhythmia.
There are also types of rhythm disturbances
, which originate in other nodes:
atrial extrasystoles or paroxysmal tachycardias;
rhythms from the atrioventricular junction;
ventricular rhythms – extrasystoles or jogging tachycardias;
atrial fibrillation or flutter.
Possible complications
Sinus arrhythmia has serious consequences, so in no case should the disease be ignored.
Poor circulation in the mother’s body negatively affects the condition of the fetus. With blood, the baby receives the necessary microelements and nutrition that are necessary for normal development. There is also a possibility of developing placental insufficiency, in which the placenta is not able to function normally. This consequence threatens the development of fetal hypoxia.
Important! The most dangerous is the development of ventricular and atrial fibrillation. This consequence can be fatal.
A serious complication is the development of heart failure . This dangerous condition threatens the life of the mother and child. Pregnancy with such a diagnosis is very difficult.
Like other heart ailments, rhythm disturbances can become chronic . In this case, negative symptoms will be constant companions of the person.
Severe arrhythmia in some cases leads to termination of pregnancy. During childbirth, rhythm disturbances can also adversely affect the course of the process.