Heart layers
Layers of the Heart
The heart has 3 layers or membranes. The middle layer is the muscular, or myocardium, (in Latin the prefix myo- means “muscle”), the thickest and densest. The middle layer provides contractile work, this layer is a true hard worker, the basis of our “motor”, it represents the main part of the organ. The myocardium is represented by striated cardiac tissue, endowed with special functions unique to it: the ability to spontaneously excite and transmit impulses to other cardiac parts through the conduction system.
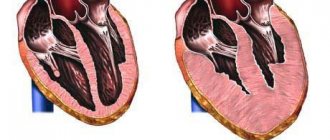
Another important difference between the myocardium and the skeletal muscles is that its cells are not multicellular, but have one nucleus and represent a network. The myocardium of the upper and lower cardiac cavities is separated by horizontal and vertical partitions of a fibrous structure; these partitions provide the possibility of separate contraction of the atria and ventricles. The muscular layer of the heart is the basis of the organ. Muscle fibers are organized into bundles; in the upper chambers of the heart there is a two-layer structure: bundles of the outer layer and the inner one.
Muscular lining of the heart
A distinctive feature of the ventricular myocardium is that in addition to the muscle bundles of the superficial layer and internal bundles, there is also a middle layer - separate bundles for each ventricle of a ring structure. The inner lining of the heart or endocardium (in Latin the prefix endo- means “inner”) is thin, one cell epithelial layer thick. It lines the inner surface of the heart, all its chambers from the inside, and the heart valves consist of a double layer of endocardium.
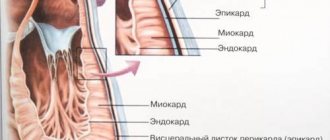
In structure, the inner lining of the heart is very similar to the inner layer of blood vessels; blood collides with this layer as it passes through the chambers. It is important that this layer is smooth to avoid thrombosis, which can form when blood cells are destroyed by hitting the heart walls. This does not happen in a healthy organ, since the endocardium has a perfectly smooth surface. The outer surface of the heart is the pericardium. This layer is represented by an outer layer of fibrous structure and an inner layer of serous structure. Between the leaves of the surface layer there is a cavity - pericardial, with a small amount of fluid.
HISTOLOGY, CYTOLOGY AND EMBRYOLOGY
The heart is compared to a pump. It pumps up to 16 tons of blood per day in an adult. The 4 chambers of the heart work in concert and continuously in accordance with the physiological needs of the body. The heart consists of three membranes: endocardium, myocardium and epicardium. The structure of the endocardium corresponds to the wall of mixed-type arteries. The myocardium consists of cardiac muscle tissue. The epicardium is a serous membrane and consists of loose connective tissue covered with single-layer squamous epithelium - mesothelium. Outside the heart is the pericardial sac, which is a double layer of the epicardium. 1. Endocardium. The structure is divided into 4 layers: endothelium on the basement membrane, then: subendothelial layer of PBCT (loose fibrous connective tissue), muscle-elastic layer (SMC and elastic fibers), outer connective tissue layer (PBCT). The heart valves are based on dense fibrous connective tissue (fibrous base), and the endocardium surrounds the fibrous base. Tendon strings from the papillary muscles of the myocardium approach the base of the valves. Development of the endocardium. The endocardium is formed from embryonic vascular tubes of mesenchymal origin, and its plates are similar to the membranes of the vessel. 2. Myocardium. The myocardium provides the contractile function of the heart. The main cell type is the contractile cardiomyocyte. Also in the myocardium there are: conducting cardiomyocytes, blood and lymphatic vessels, thin layers of RVST and elements of dense connective tissue: tendon rings at the base of the valves, tendon filaments, autonomic nerve nodes, nerve fibers and many endings of the sympathetic and parasympathetic nervous system.
The contractile cells of the myocardium have the shape of a cylinder, while the rounded bases of the cells contact each other, forming a fiber - the functional unit of the myocardium. Between cardiomyocytes, this area of contact is called an intercalary disc, consisting of plasmalemmas of two cardiomyocytes, between which there are gap-like junctions and desmomomas. Cardiomyocytes of the ventricles are located more densely to each other, with a diameter of up to 20 µm, cardiomyocytes of the atria have more lateral anastomoses (connections between the lateral surfaces of cells for contact of two adjacent fibers from cardiomyocytes). In cardiomyocytes, among the organelles, 35-50% are myofibrils, 30-35% are mitochondria, 10-14% are EPS. Each cell contacts 2-3 capillaries through the basement membrane. Every fifth cardiomyocyte has contact with a sympathetic nerve ending. Conducting cardiomyocytes are divided into P-cells (pacemaker-pacemaker), transitional and Purkinje cells. These cells have a more hydrophilic cytoplasm, the contractile apparatus and T-tubes are significantly reduced, they are specialized not for contraction, but for generating (R-cells) and conducting an impulse that is transmitted to contractile cardiomyocytes, which ensures the autonomy of myocardial contraction. β-cells are impulse generators and are concentrated primarily in the sinus node. They are located in groups, each of which is surrounded by a basement membrane. Round or oval-shaped cells with a diameter of 10-12 microns work as pulse generators, forming and “resetting” membrane potential from the cytolemma. The frequency of impulses can be accelerated by adrenaline, norepinephrine (sympathetic nerve endings), slowed down by acetylcholine (parasympathetic nerve endings). Transitional (intermediate) conduct impulses to Purkinje cells, are localized in the atrioventricular node, the legs of the conduction system (bundles of His). In humans, these cells are similar in shape and size to contractile cells. Purkinje cells form connections between transitional and contractile cells. Slightly larger in size than contractiles. Secretory cardiomyocytes. In an adult, they are located in the myocardium of the right atrium and produce natriuretic peptides (natriuretic vasodilating factor or atriopeptin) - powerful factors that lower blood pressure (hypotensive factors) and increase urination (diuresis). In secretory cardiomyocytes, the contractile apparatus is significantly reduced, the peptide synthesis apparatus (EPS group) is well developed, and there are many granules with natriuretic peptide (atriopeptin, etc.). 3. Epicardium - is a visceral layer of the pericardium, ensures the free sliding of the heart in the heart sac, has two plates: the outer one - mesothelium (single-layer squamous epithelium, capable of secreting a small amount of serous fluid); internal - RVST with vessels and nerves, there may be accumulations of adipose tissue. Examples of the clinical significance of the studied heart structures. 1. Cells of the conduction system are more sensitive to the action of chemicals and toxins than contractile cardiomyocytes; these and other non-physiological effects can lead to rhythm disturbances. 2. Hemolytic streptococci (causing, for example, sore throat) can penetrate from the blood into the subendothelial layer of the endocardium or cause destruction of the endothelium of the heart. This can lead to the formation of blood clots. When streptococcal colonies are localized in the heart valves, destruction of the PBCT fibers and deformation of the valve (valvular defect) occurs. 3. Atherosclerotic changes in the distributive (coronary) arteries of the myocardium lead to a narrowing of their lumen, to a decrease in the flow of nutrients and oxygen (ischemia) to cardiomyocytes. These disorders can be removed by bypass surgery of the altered vessel. 4. Smoking doubles the risk of developing coronary heart disease (CHD). 5. Long-term vascular hypertension increases the load on the myocardium and leads to ischemic heart disease.
Share on social media networks
RќСЂР°РІРёС‚СЃСЏ
Going deeper into the outer layer
Structure of the heart wall
So, the pericardium is not a single outer layer of the heart, but a layer consisting of several plates: fibrous and serous. The fibrous pericardium is dense and outer. It performs a largely protective function and the function of some kind of fixation of the organ in the chest cavity. And the inner, serous layer fits tightly directly to the myocardium; this inner layer is called the epicardium. Imagine a bag with a double bottom? This is what the outer and inner pericardial layers look like.
The gap between them is the pericardial cavity; normally it contains from 2 to 35 milliliters of serous fluid. Liquid is needed for softer friction of the layers against each other. The epicardium tightly covers the outer layer of the myocardium, as well as the initial sections of the largest vessels of the heart; its other name is the visceral pericardium (in Latin viscera - organs, entrails), i.e. this is the layer lining the heart itself. And the parietal pericardium is the outermost layer of all cardiac membranes.
The following sections or walls are distinguished in the superficial pericardial layer; their name depends directly on the organs and areas to which the membrane is adjacent. Pericardial walls:
- Anterior wall of the pericardium. Adjacent to the chest wall
- Diaphragmatic wall. This shell wall is directly fused with the diaphragm.
- Lateral or pleural. They are located on the sides of the mediastinum, adjacent to the pulmonary pleura.
- Rear. It borders on the esophagus and descending aorta.
The anatomical structure of this lining of the heart is complex, because in addition to the walls, the pericardium also contains sinuses. These are physiological cavities; we will not delve into their structure. It is enough just to know that between the sternum and the diaphragm there is one of these pericardial sinuses - the anteroinferior. It is this that, in pathological conditions, is pierced or punctured by health workers. This diagnostic procedure is high-tech and complex, carried out by specially trained personnel, often under ultrasound control.
Why does the heart need a bag?
Pericardium and its structure
Our main “motor” of the body requires extremely careful treatment and care. Probably for this purpose, nature clothed the heart in a bag - the pericardium. First of all, it performs a protective function, carefully wrapping the heart in its shell. Also, the pericardial sac fixes and secures our “motor” in the mediastinum, preventing displacement during movements. This is possible due to the strong fixation of the surface of the heart with the help of ligaments to the diaphragm, sternum, and vertebrae.
It should be noted the role of the pericardium as a barrier to cardiac tissue from various infections. The pericardium “fences off” our “motor” from other organs of the chest, clearly defining the position of the heart and helping the heart chambers to better fill with blood. At the same time, the surface layer prevents excessive expansion of the organ due to sudden overloads. Preventing chamber overdistension is another important role of the outer wall of the heart.
The structure of the human heart - anatomy
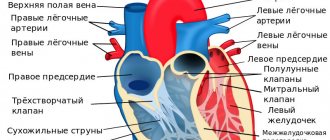
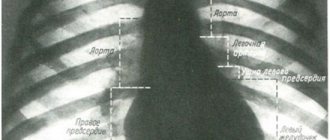
The heart muscle consists of 4 chambers - 2 atria and 2 ventricles. The left ventricle and left atrium form the so-called arterial part of the organ, based on the nature of the blood found here. In contrast, the right ventricle and right atrium make up the venous part of the heart.
The circulatory organ is presented in the shape of a flattened cone. It consists of a base, apex, lower and anterosuperior surfaces, as well as two edges - left and right. The apex of the heart has a rounded shape and is formed entirely by the left ventricle. The atria are located in the base area, and in its anterior part lie the pulmonary trunk and aorta.
When the pericardium is sick
Pericarditis - inflammation of the pericardial sac
Inflammation of the outer lining of the heart is called pericarditis. The causes of the inflammatory process can be infectious agents: viruses, bacteria, fungi. This pathology can also be triggered by chest trauma, direct cardiac pathology, for example, acute heart attack. Also, exacerbation of systemic diseases such as SLE and rheumatoid arthritis can serve as the beginning of a chain of inflammatory phenomena in the superficial cardiac layer.
Pericarditis often accompanies tumor processes in the mediastinum. Depending on how much fluid is released into the pericardial cavity during inflammation, dry and effusion forms of the disease are distinguished. Often these forms replace each other in this order with the course and progression of the disease. A dry cough, chest pain, especially when taking a deep breath, changing body position, or coughing are characteristic of the dry form of the disease.
The effusion form is characterized by a slight decrease in the severity of pain, and at the same time, chest heaviness, shortness of breath, and progressive weakness appear. With pronounced effusion into the pericardial cavity, the heart appears as if squeezed in a vice, and the normal ability to contract is lost. Shortness of breath haunts the patient even at rest, active movements become completely impossible. The risk of cardiac tamponade increases, which can be fatal.
What is responsible for the work of the heart?
As is known, the functioning of the heart muscle is not a voluntary act. The organ remains active continuously, even when a person is in a state of deep sleep. There are hardly people who pay attention to their heart rate during activity. But this is achieved due to a special structure built into the heart muscle itself - a system for generating biological impulses. It is noteworthy that the formation of this mechanism occurs in the first weeks of intrauterine conception of the fetus. Subsequently, the impulse generation system does not allow the heart to stop throughout life.
Heart injection or pericardial puncture
Cardiac puncture
This manipulation can be carried out both for diagnostic and therapeutic purposes. The doctor performs a puncture when there is a threat of tamponade, with significant effusion, when it is necessary to pump out fluid from the heart sac, thereby providing the organ with the opportunity to contract. For diagnostic purposes, a puncture is performed to clarify the etiology or cause of inflammation. This manipulation is very complex and requires a highly qualified doctor, since it carries a risk of heart damage.
Epicard
The presented membrane of the heart muscle has the smoothest, thinnest and somewhat transparent structure. The epicardium forms the outer tissue of the organ. In fact, the membrane acts as the inner layer of the pericardium - the so-called cardiac sac.
The surface of the epicardium is formed from mesothelial cells, under which there is a connective, loose structure represented by connective fibers. In the region of the apex of the heart and in its grooves, the lining in question includes adipose tissue. The epicardium fuses with the myocardium in the areas of least accumulation of fat cells.