The human venous system is a collection of various veins that provide adequate blood circulation in the body. Thanks to this system, all organs and tissues are nourished, as well as the regulation of water balance in cells and the removal of toxic substances from the body. Its anatomical structure is similar to the arterial system, but there are some differences responsible for certain functions. What is the functional purpose of veins and what diseases can arise when the patency of blood vessels is impaired?
general characteristics
Veins are vessels of the circulatory system that carry blood to the heart. They are formed from branched venules of small diameter, which are formed from a capillary network. The set of venules is transformed into larger vessels, from which the main veins are formed. Their walls are somewhat thinner and less elastic than those of arteries, since they are subject to less stress and pressure.
The further the blood vessels are from the heart, the lower the pressure in them
Blood flow through the vessels is ensured by the work of the heart and chest when, during inhalation, the diaphragm contracts, forming negative pressure. There are valves in the vascular walls that prevent the reverse flow of blood. A factor contributing to the functioning of the venous system is the rhythmic contraction of the muscle fibers of the vessel, pushing the blood upward, thereby creating venous pulsation.
The blood vessels that carry blood away from the tissues of the neck and head contain fewer valves because gravity allows blood to circulate more easily above the heart.
VIENNS
Veins are blood vessels that carry blood from capillaries back to the heart. The blood, having given oxygen and nutrients to the tissues through the capillaries and filled with carbon dioxide and decay products, returns through the veins to the heart. It is worth noting that the heart has its own blood supply system - the coronary circle, which consists of coronary veins, arteries and capillaries. Coronary vessels are identical to other similar vessels in the body.
The walls of the veins consist of three layers, which, in turn, include various tissues:
- The inner layer is very thin, consisting of simple cells located on an elastic membrane of connective tissue.
- The middle layer is more durable and consists of elastic and muscle tissue.
- The outer layer consists of a thin layer of loose and mobile connective tissue, through which the lower layers of the venous membrane are nourished and thanks to which the veins are attached to the surrounding tissues.
Through the veins, the so-called reverse circulation occurs - blood from the body tissues flows back to the heart. For veins located in the upper part of the body, this is possible because the walls of the veins are distensible and the pressure in them is less than in the right atrium, which performs the task of “suction”. The situation is different with veins located in the lower part of the body, especially in the legs, since in order for the blood from them to flow back to the heart, it must overcome gravity. To perform this function , the veins located in the lower part of the body are equipped with a system of internal valves that force blood to flow only in one direction - upward - and prevent the blood from flowing back. In addition, in the lower extremities there is a “muscle pump” mechanism that contracts the muscles between which the veins are located so that blood flows upward through them.
types of veins in the peripheral system : superficial veins, located very close to the surface of the body, which are visible through the skin, especially on the extremities, and deep veins, located between the muscles, usually following the trajectory of the main arteries. In addition, especially in the lower extremities, there are perforating and communicating veins that connect both parts of the venous system and facilitate the flow of blood from the superficial veins to the thicker deep veins and then to the heart.
Valves, which allow blood flow in only one direction: from the superficial to the deep veins and from the deep to the heart, consist of two folds on the inner walls of the veins, or hemispherical valves: when the blood is pushed upward, the walls of the valves rise and allow a certain amount of blood to pass through up; when the impulse dries up, the valves close under the weight of the blood. Thus, the blood cannot go down and with the next impulse rises another flight, always in the direction of the heart.
How is blood circulation carried out?
The human venous system is conventionally divided into the pulmonary and systemic circulation. The small circle is designed for thermoregulation and gas exchange in the pulmonary system. It originates from the cavity of the right ventricle, then the blood flows to the pulmonary trunk, which consists of small vessels and ends in the alveoli. Oxygenated blood from the alveoli forms a venous system, which flows into the left atrium, thereby completing the pulmonary circulation. Complete blood circulation takes less than five seconds.
Diagram of the pulmonary and systemic circulation
The task of the systemic circulation is to provide all tissues of the body with oxygen-enriched blood. The circle originates in the cavity of the left ventricle, where high oxygen saturation occurs, after which the blood enters the aorta. The biological fluid saturates the peripheral tissues with oxygen, then returns to the heart through the vascular system. From most organs of the digestive tract, blood is initially filtered in the liver rather than moving directly to the heart.
content .. 150 151 152 153 154 155 156 157 158 159 ..Veins of the upper limb (human anatomy)
The veins of the upper limb are divided into superficial
and
deep
. All of them have valves and flow into a large venous trunk - the axillary vein, v. axillaris, continuing into the subclavian vein, v. subclavia.
Superficial veins
begin with venous networks located in the subcutaneous tissue of the hand and forearm. There are two large veins (Fig. 172).
Rice. 172. Superficial veins of the upper limb, anterior (palmar) surface. 1 - rete venosum palmare; 2 - v. cephalica; 3 - v. basilica; 4 - v. mediana antebrachii; 5 - v. mediana cubiti; 6 - v. basilica; 7 - v. cephalica
1. Cephalic vein
, v. The cephalica begins from the rete dorsalis manus on the radial side of the hand. On the forearm and in the ulnar fossa it is located in front, and on the shoulder it runs along the sulcus bicipitalis lateralis. In the deltoid-pectoral groove, the vein plunges under the clavicle and flows into the v. axillaris.
2. Royal Vienna
, v. basilica, is formed from the venous network of the hand on the ulnar side. On the forearm and hand it anastomoses with the branches of v. cephalica, flows into the axillary vein in the axillary fossa. Its major anastomosis is v. mediana cubiti, located under the skin of the ulnar fossa and crossing it in an oblique direction. This vein not only connects the superficial veins, but also establishes an anastomosis between the superficial and deep veins of the upper limb. The position and diameter of the middle vein of the cubital fossa are not always constant.
Deep veins
, as a rule, accompany all arterial vessels of the upper limb, most often with paired trunks.
Axillary vein
, v. axillaris, is formed from the fusion of the brachial vein, v. brachialis, as well as the following veins flowing into it: 1) lateral thoracic, v. thoracica lateralis; 2) thoraco-epigastric, vv. thoracoepigas tricae. The trunk of the axillary vein in the fossa of the same name passes in front of a. axillaris to the 1st rib, continuing further into v. subclavia.
Subclavian vein (human anatomy)
In the formation of the subclavian vein
, v. subclavia, the veins of the upper limb (v. axillaris), chest and shoulder girdle (uv. perforates, uu. thoracoacromiales) and neck (i. jugularis externa, v. jugularis anterior) take part. The last two veins form in the neck and represent large trunks.
1. External jugular vein
, v. jugularis externa, steam room, merges from the occipital and posterior auricular veins below the external auditory canal. Descends along m. sternocleidomastoideus, crossing it in the middle part from front to back, and reaches the supraclavicular fossa in the region of the lateral triangle of the neck, where it flows into the subclavian vein. Anastomoses with the branches of the internal jugular vein.
2. Anterior jugular vein
, v. jugularis anterior, steam room, is formed from the veins of the skin of the chin and muscles above the hyoid bone. It then passes under the skin along the sides of the neck and joins the subclavian vein or the external jugular vein. The right and left anterior jugular veins connect to each other through the arcus venosus juguli, located above the jugular notch of the sternum in the suprasternal interfascial space of the neck.
By going around the first rib in front of m. scalenus anterior near the sternoclavicular joint, the subclavian vein connects with the internal jugular vein, forming the brachiocephalic vein, v. brachiocephalica, paired large vessel.
Brachiocephalic veins (human anatomy)
Brachiocephalic veins
,vv. brachiocephalicae dextra et sinistra, participate in the formation of the superior vena cava (see Fig. 169). The brachiocephalic veins are paired large trunks with a diameter of 15-17 mm, formed by the fusion of v. jugularis interna and v. subclavia behind the sternoclavicular joint of the corresponding side. The right brachiocephalic vein is 2-3 cm long, runs almost vertically behind the sternoclavicular joint, the left one is 2 times longer than the right one, crosses in front the large branches of the aortic arch, the left vagus and phrenic nerves. Behind the attachment of the first rib to the sternum, the left vein connects with a similar right vein, forming the superior vena cava. Smaller veins drain into the brachiocephalic veins:
1. Inferior thyroid vein
, v. thyreoidea inferior, begins from the thyroid plexus and receives blood from the thyroid gland, larynx, trachea, lower pharynx and esophagus.
2. Most inferior thyroid vein
, v. thyreoidea ima, the only one, is located in the middle part of the neck, often flows into v. brachiocephalica sinistra or at the confluence of the right and left brachiocephalic veins.
3. Veins of the mediastinum
: the thymus gland, fiber and lymph nodes of the mediastinum, bronchi, trachea and esophagus - all flow through independent trunks into the lower part of the right and left brachiocephalic veins.
4. Vertebral vein
, v. vertebralis, steam room, begins from the suboccipital plexus and the plexus of veins of the spinal column. Located together with the vertebral artery. Coming out of the opening of the transverse process of the VI cervical vertebra, it flows into the initial section of the brachiocephalic vein.
5. Deep jugular vein
, v. cervicalis profunda, steam room, accompanies the artery of the same name, flows into the initial part of the brachiocephalic vein, sometimes into the vertebral vein.
6. Internal mammary veins
,vv. thoracicae internae, paired, begin from the connection of the superior epigastric veins of the abdomen and the muscular-diaphragmatic veins. Double trunks accompany the internal thoracic artery, anastomosing with the intercostal veins. The right vein sometimes joins the superior vena cava.
7. Highest intercostal vein
, v. intercostalis suprema, steam room, collects blood from 2-3 upper intercostal muscles.
Azygos and semi-gypsy veins (human anatomy)
Azygos vein
, v. azygos, begins in the abdominal cavity from vv. lumbales dextrae and their anastomoses, which form the ascending lumbar vein at the level of the first lumbar vertebra. The azygos vein penetrates the chest cavity through the opening between the right medial and intermediate crura of the diaphragm. In the thoracic cavity, the azygos vein lies on the right side of the thoracic vertebral bodies. To the left of it are the thoracic lymphatic duct and the thoracic aorta. The vein is covered in front by the esophagus. The azygos vein, rising in the posterior mediastinum, at the level of the IV-V thoracic vertebrae lies behind the root of the right lung, then bends around the right bronchus from behind and above, flowing into the superior vena cava at the site where it perforates the pericardium.
The hemizygos vein, v., takes part in the formation of the vein. hemiazygos, which is the largest tributary of the azygos vein. The hemizygos vein is formed from the left ascending lumbar vein, v. lumbalis ascendens sinistra, in the abdominal cavity this vein anastomoses with the lumbar veins. The hemizygos vein enters the chest cavity through a hole in the diaphragm between the left medial and intermediate legs. The XI-VII left posterior intercostal veins, vv., flow into the hemizygos vein. intercostales posteriores sinistrae; accessory azygos vein, v. hemiazygos accessoria, formed from VI-III intercostal veins; esophageal veins, vv. esophageae, mediastinal veins, vv. mediastinales; The posterior intercostal veins are connected by anastomoses with the vertebral venous plexuses. In addition, the following flow into the azygos vein: 1) IV-XI right posterior intercostal veins, vv. intercostales posteriores dextrae; 2) subcostal vein, v. subcostalis; 3) bronchial veins, vv. bronchioles; 4) superior phrenic veins, vv. phrenicae superiores; 5) right superior intercostal vein, v. intercostalis superior dextra; as well as anastomoses that connect the anterior and posterior intercostal veins with the venous plexuses of the spinal column; 6) esophageal veins, vv. esophagea; 7) mediastinal veins, vv. mediastinales; pericardial veins, vv. pericardiacae.
hemiazygos, which is the largest tributary of the azygos vein. The hemizygos vein is formed from the left ascending lumbar vein, v. lumbalis ascendens sinistra, in the abdominal cavity this vein anastomoses with the lumbar veins. The hemizygos vein enters the chest cavity through a hole in the diaphragm between the left medial and intermediate legs. The XI-VII left posterior intercostal veins, vv., flow into the hemizygos vein. intercostales posteriores sinistrae; accessory azygos vein, v. hemiazygos accessoria, formed from VI-III intercostal veins; esophageal veins, vv. esophageae, mediastinal veins, vv. mediastinales; The posterior intercostal veins are connected by anastomoses with the vertebral venous plexuses. In addition, the following flow into the azygos vein: 1) IV-XI right posterior intercostal veins, vv. intercostales posteriores dextrae; 2) subcostal vein, v. subcostalis; 3) bronchial veins, vv. bronchioles; 4) superior phrenic veins, vv. phrenicae superiores; 5) right superior intercostal vein, v. intercostalis superior dextra; as well as anastomoses that connect the anterior and posterior intercostal veins with the venous plexuses of the spinal column; 6) esophageal veins, vv. esophagea; 7) mediastinal veins, vv. mediastinales; pericardial veins, vv. pericardiacae.
Superior vena cava (human anatomy)
Superior vena cava
, v. cava superior, single, 5-6 cm long, 20-23 mm in diameter, located vertically. On the right side it is adjacent to the right mediastinal pleura, and on the left - to the ascending aorta, covered in front by the thymus gland. At the level of the 2nd rib it pierces the pericardium and at the level of the 3rd rib it flows into the right atrium. The intrapericardial part is adjacent to the anterior part of the root of the right lung. V. flows into the superior vena cava before passing through the pericardium. azygos and small veins of the pericardium and anterior mediastinum.
Inferior vena cava system (human anatomy)
Inferior - vena cava, v. cava inferior, collects blood from the lower extremities, torso, paired abdominal organs and liver.
Veins of the lower limb (human anatomy)
The veins of the lower limb are divided into superficial and deep.
Superficial veins
lie in the subcutaneous tissue and merge from the small veins of the foot and leg, which form the dorsal and plantar networks. The largest are the large and small hidden veins.
1. Small hidden vein
, v. saphena parva, originates on the lateral surface of the foot. On the lower leg it is located lateral to the triceps tendon, and then lies along the midline on the back surface of the lower leg. In the popliteal fossa, perforating the fascia, it divides into two branches, connecting with the popliteal vein and with the branch of the deep vein of the thigh.
2. Great hidden vein
, v. saphena magna, formed in the area of the medial malleolus and dorsum of the foot, passes along the medial surface of the lower leg and knee joint. It crosses the thigh along the anteromedial surface, flowing into the femoral vein in the fossa ovalis area. The saphenous veins of the anterior abdominal wall, inguinal and iliac regions flow into the mouth of the large hidden vein. There are anastomoses on the lower leg between the small and large hidden veins.
Deep veins of the thigh
repeat the branches of the arteries. There are double veins on the lower leg. All veins of the lower limb merge into the femoral vein, v. femoralis, which passes behind the inguinal ligament in the lacuna vasorum medial to the femoral artery. Above the inguinal ligament, already in the abdominal cavity, it passes into the veins of the pelvis a, v. iliaca externa.
External iliac vein
, v. iliaca externa, is located first medial to the external iliac artery, and then behind it. The inferior epigastric vein, v., flows into the external iliac vein. epigastrica inferior, and the deep vein surrounding the ilium, v. circumflexa ilium profunda. These veins collect blood from the anterior abdominal wall and the inner surface of the pelvis.
Internal iliac vein
, v. iliaca interna, is formed from the veins of the same name, accompanying the parietal and splanchnic arteries of the pelvis. A special feature is that in the small pelvis around the uterus, vagina, rectum, bladder and prostate gland there are extra-organ venous plexuses. Inferior and middle rectal veins, vv. rectales inferiores et mediates, originate from these plexuses and flow into the internal iliac vein, and the superior rectal vein, v. rectalis superior, - into the inferior mesenteric vein (portal vein system). The rectum also has a well-developed submucosal venous plexus, where veins can easily expand to form hemorrhoids.
Inferior vena cava
, v. cava inferior, is formed from the confluence of the common iliac veins at the level of the IV-V lumbar vertebrae to the right of the aorta. It also receives parietal and internal branches.
Parietal
The tributaries of the inferior vena cava are as follows.
1. Median sacral vein
, v. sacralis media, originates from the venous sacral plexus.
2. Lumbar veins
,vv. lumbales, paired, begin in the muscles of the lateral wall of the abdomen. The posterior muscular and dorsal branches flow into them. Near the diaphragm they form v. lumbales ascendens, and below they anastomose with v. iliommbalis, which flows into the common iliac vein. The lumbar veins connect to the vertebral venous plexus.
3. Veins of the spinal column
conditionally divided into external and internal vertebral venous plexuses. At the top (cervical part of the spinal column) they anastomose with the venous sinuses and branches of the superior vena cava system, at the bottom - with the parietal branches of the inferior cava and internal iliac veins. The outflow of blood from the plexuses occurs in vv. lumbales, intercostales posteriores et vertebrales.
Internal
The branches of the inferior vena cava consist of two groups. The first group includes veins that flow directly into the inferior vena cava. The veins of the second group merge into a single trunk - the portal vein, which again divides into capillaries of the liver lobules, which are tributaries of the hepatic veins; these veins drain into the inferior vena cava.
The first group of branches. 1. Testicular vein (ovarian)
, v. testiculars (v. ovarica), steam room, collects blood from the gonad, forming a pampiniform plexus, plexus pampiniformis, in the spermatic cord (in women in the lig. suspensorium ovarii). The right vein of the testicle (ovary) flows directly into the inferior vena cava, the left into the left renal vein.
2. Renal vein
, v. renalis, steam room, exits the portal of the kidney in front of the renal artery. The left renal vein crosses the abdominal aorta, 15-20 mm longer than the right one. The veins of the kidney capsule flow into the renal vein. The latter anastomose with the lumbar and ureteral veins.
3. Adrenal vein
, v. suprarenalis, steam room, wide (3-4 mm); the right one flows into the inferior vena cava, the left one into the left renal vein.
4. Hepatic veins
,vv. hepaticae, 3-4 trunks flow into the inferior vena cava at the point of passage through the notch in the posterior edge of the liver.
Portal vein system (human anatomy)
Portal vein
, v. porta, collects blood from the unpaired organs of the abdominal cavity (stomach, small and large intestines, pancreas and spleen) and goes to the liver, where it branches into right and left branches, then lobar, segmental, interlobular veins. From them originate sinusoids (capillaries), which in the center of the lobule merge into the central veins. The central veins of the lobules are the drainages of the hepatic veins. The portal vein is formed by the following veins (Fig. 173).
Rice. 173. Diagram of the formation of the portal vein. 1 - v. mesenterica superior; 2 - stomach tilted up; 3 - origin of the greater omentum; 4 - v. gastrica sinistra; 5 - spleen; 6 - tail of the pancreas; 7 - v. lienalis; 8 - v. mesenterica inferior; 9 - descending colon; 10 - rectum; 11, 12, 13 - vv. rectales inferior, media et superior; 14 - ileum; 15 - ascending colon; 16 - head of the pancreas; 17 - v. colica media; 18 - v. portae; 19 - gallbladder vein; 20 - gall bladder; 21 - beginning of the duodenum; 22 - liver (thrown up); 23 - v. gastroepiploica dextra; 24 - v. gastrica dextra
1. Superior mesenteric vein
, v. mesenterica superior, single, collects blood from the small intestine (vv. jejunales et ilei), appendix and cecum (vv. iliocolicae), ascending colon (v. solica dextra), transverse colon (v. colica media), pancreas glands and duodenum (vv. pancreaticoduodenales). At the root of the mesentery of the small intestine, the superior mesenteric vein is located to the right of the artery of the same name.
2. Splenic vein
, v. lienalis, single, drains blood from the spleen, fundus, body and greater curvature of the stomach (v. gastroepiploica dextra, vv. gastricae breves), and pancreas (vv. pancreaticae). The splenic vein connects behind the head of the pancreas and the upper horizontal part of the duodenum with the superior mesenteric vein.
3. Inferior mesenteric
, Vienna, v. mesenterica inferior, collects blood from the descending colon (v. colica sinistra), sigmoid (vv. sigmoideae) and upper part of the rectum (v. rectalis superior). The inferior mesenteric vein joins the splenic vein in the middle of the pancreas or flows into the junction of the superior mesenteric and splenic veins.
4. Directly with the portal vein
connect: cystic vein, v. cystica, periumbilical veins, vv. paraumbilicales, located in lig. teres hepatis, left and right gastric veins, vv. gastricae sinistra et dextra, prepyloric vein, v. prepylorica.
The portal vein from the place of formation (behind the head of the pancreas) to the portal of the liver has a length of 6-8 cm, a diameter of 15-20 mm, and lies in the lig. hepato duo denote, where the ductus choledochus passes to the right of it, and a. hepatica propria. At the porta hepatis, the portal vein divides into two large branches, which in turn branch into 8 segmental veins. Segmental veins are divided into interlobular veins, which form sinusoids of lobules. Ultimately, all the blood passes through the capillaries of the lobules, from which large branches are again formed - the hepatic veins, vv. hepaticae, flowing into the inferior vena cava. Thus, venous blood from the internal organs of the abdominal cavity passes through the liver before entering the lower vein.
Anastomoses between the branches of the portal, superior and inferior vena cava (human anatomy)
Anastomoses of the branches of the portal vein with the branches of the superior and inferior vena cava - porta-caval anastomoses, anastomoses portacavales, ensure the passage of blood from the portal vein to the superior and inferior vena cava when blood flow through the liver is disrupted. There are four main portacaval anastomoses (Fig. 174).
Rice. 174. Anastomoses between the superior and inferior vena cava and with the portal vein. 1 - v. subclavia; 2 - v. brachiocephalica dextra; 3 - chest wall; 4 - v. thoracoepigastrica; 5 - v. thoracica interna; 6 - v. azygos; 7 - v. esophagea; 8 - vv. intercostales posteriores; 9 - v. portae; 10 - desolate v. umbilicalis; 11, 14 - vv. paraumbilicales; 12 - navel; 13 - residual channel; v. umbilicalis; 15 - v. lumbalis; 16 - v. lum-balis ascendens; 17 - abdominal wall; 18 - v. epigastrica interior; 19 - v. iliaca communis; 20 - v. epigastrica superficialis; 21 - vv. restates media et inferior; 22 - v. iliaca externa; 23 - v. iliaca interna; 24 - plexus rectalis; 25 - v. rectalis superior; 26 - v. cava inferior; 27 - v. mesenterica inferior; 28 - v. mesenterica superior; 29 - v. porta; 30, 31 — veins of the esophagus; 32, 33 - v. hemiazygos accessoria; 34 - v. cava superior; 35 - v. brachiocephalica sinistra; 36 - v. hemiazygos; 37 - v. gastrica sinistra
1. Blood from the portal vein is directed retrogradely to the veins of the stomach, which anastomose with the veins of the esophagus. The veins of the esophagus flow into v. azygos and v. hemiazygos (tributaries of the superior vena cava).
2. Blood from the portal vein flows back into v. mesenterica inferior, and then in v. rectalis superior, which anastomoses in the wall of the rectum with vv. rectales media et inferior, which are branches of the internal iliac vein. From it the blood passes into the common iliac and inferior vena cava.
3. Blood from the portal vein enters vv. paraumbilicales, which are connected through v. thoracica interna and v. thoracoepigastrica - with the superior vena cava and through anastomoses with vv. paraumbilicales, vv. epigastricae inferiores and vv. epigastricae superficiales - with the inferior vena cava.
4. The veins of the kidney capsule anastomose with the splenic and inferior mesenteric veins, on the one hand, and the renal veins, on the other, thus forming porto-caval anastomoses on the posterior abdominal wall.
Anastomoses between the branches of the superior and inferior vena cava - cava-caval anastomoses, anastomoses cavacavales, are developed in every person. They function especially well when blood flow through the inferior or superior vena cava is obstructed. The following anastomoses are distinguished.
1. The veins of the anterior abdominal wall (vv. thoracoepigastricae, vv. epigastricae superiores) from the superior vena cava system in the area of the umbilical ring anastomose vv. epigastricae inferieres, vv. epigastricae superficiales from the inferior vena cava system.
2. On the posterior wall of the body there are anastomoses between the superior and inferior vena cava due to the vertebral venous plexuses. These plexuses in the cervical part of the spinal column connect to the veins of the head and neck, which are branches of the superior vena cava system. In the lower part of the spinal column, the vertebral plexuses anastomose with the lumbar veins, which are branches of the inferior vena cava.
3. On the posterior wall of the body there are anastomoses between the lumbar veins (inferior vena cava system), azygos and semi-gyzygos veins (superior vena cava system) due to the ascending lumbar veins and venous plexuses of the spinal column.
Fetal circulation (human anatomy)
The fetus is nourished in the womb by the placenta (baby place), which grows with its villi into the mucous membrane of the uterus (Fig. 175). The umbilical vein, which contains arterial blood, departs from the placenta. The vein passes along the umbilical cord and through the umbilical opening in the anterior abdominal wall into the abdominal cavity. In the abdominal cavity, the umbilical vein divides into two branches: one goes to the inferior vena cava, and the second goes to the portal vein. In the portal and inferior vena cava, arterial blood first mixes with venous blood, which flows through these vessels. Mixed blood flows through the inferior vena cava into the right atrium of the fetal heart, and then a significant portion of the blood flows through the foramen ovale into the left atrium. This is facilitated by the difference in blood pressure, since very little blood enters the left atrium through the pulmonary veins and the pressure will be lower than in the right atrium. The blood of the inferior and superior vena cava in the right atrium hardly mixes. Due to the structural features of the heart, the blood of the inferior vena cava, being more arterialized, is directed through the foramen ovale into the left atrium, and a smaller part of the blood of the right atrium (mainly blood from the superior vena cava) enters the right ventricle through the right atrioventricular foramen.
From the right ventricle, blood is ejected into the truncus pulmonalis, where at the site of its branching into the right and left aa. pulmonales, under the aortic arch there is an arterial duct, ductus arteriosus, through which part of the venous blood from the truncus pulmonalis enters the aorta. The ductus arteriosus enters the descending aorta below the point where the great vessels arise headward from the aortic arch. This creates conditions for a richer supply of oxygen to the nervous system, since the blood of the left ventricle entering the aortic arch is more arterialized than the blood of the aorta below the confluence of the ductus arteriosus.
Mixed blood through the aorta is distributed to the vessels supplying blood to the organs. Among the branches going to the pelvic organs from the internal iliac artery, the umbilical artery (paired), a. umbilicalis.
On the anterior abdominal wall, the umbilical arteries are located on the sides of the bladder and come together at its apex. Through the umbilical opening they penetrate the umbilical cord and reach the placenta. In the placenta, arteries form capillaries of the villi.
In the placenta, mixing of the blood of mother and fetus does not occur. The placental villi are immersed in the lacunae of the uterine mucosa, through which the mother’s blood circulates. Gases, nutrients and toxic substances, hormones and water penetrate by diffusion from the mother's blood into the fetal blood and vice versa.
After birth, when the placental circulation is interrupted, the small (pulmonary) circle turns on more intensely. At this point, the lung tissue and vessels of the pulmonary circulation are well prepared for intense gas exchange. The lumen of the ductus arteriosus gradually closes due to the growth of the intima. This is facilitated by contraction of the muscles of the duct wall. After 6-8 months, the ductus arteriosus turns into a ligament.
From the moment of complete inclusion of the pulmonary circulation, equilibrium occurs in the flow of blood into the right and left atria. The valve of the foramen ovale remains inactive and between 6-8 months the closure of this hole occurs. It has been established that in 20-25% of adults the septal valve does not heal completely. If the holes are small, this does not cause noticeable functional impairment.
When the umbilical cord is ligated in a newborn, involution of the umbilical vein and arteries is observed after 3-5 weeks. The umbilical vein, running from the umbilical ring to the porta hepatis, becomes the round ligament of the liver and the venous ligament, extending from the liver to the inferior vena cava. In these ligaments, partial patency of the reduced vein is observed. The umbilical arteries are also partially obliterated. In an adult, patency remains only in their initial part, and the proximal part turns into a ligament. umbilicale medium.
content .. 150 151 152 153 154 155 156 157 158 159 ..
Functional purpose
The full functioning of blood circulation depends on many factors, such as:
- individual features of the structure and location of veins;
- gender;
- age category;
- lifestyle;
- genetic predisposition to chronic diseases;
- the presence of inflammatory processes in the body;
- metabolic disorders;
- actions of infectious agents.
If a person is identified with risk factors that affect the functioning of the system, he should follow preventive measures, since with age there is a risk of developing venous pathologies.
Vessels contribute to the saturation of tissues with carbon dioxide
Main functions of venous vessels:
- Blood circulation. Continuous movement of blood from the heart to organs and tissues.
- Transport of nutrients. They ensure the transfer of nutritional components from the digestive tract into the bloodstream.
- Distribution of hormones. Regulation of active substances that carry out humoral regulation of the body.
- Excretion of toxins. Removal of harmful substances and metabolic end products from all tissues to the organs of the excretory system.
- Protective. The blood contains immunoglobulins, antibodies, leukocytes and platelets, which protect the body from pathogenic factors.
Veins carry out general and local regulation of blood circulation
The venous system takes an active part in the spread of the pathological process, since it serves as the main route for the spread of purulent and inflammatory phenomena, tumor cells, fat and air embolism.
Structural features
The anatomical features of the vascular system lie in its important functional significance in the body and in conditions of blood circulation. The arterial system, unlike the venous system, functions under the influence of the contractile activity of the myocardium and does not depend on the influence of external factors.
The anatomy of the venous system implies the presence of superficial and deep veins. Superficial veins are located under the skin; they begin from the superficial vascular plexuses or venous arch of the head, torso, lower and upper extremities. Deeply located veins, as a rule, are paired, originate in separate parts of the body, and accompany the arteries in parallel, which is why they get the name “satellites”.
The structure of the venous network consists of the presence of a large number of vascular plexuses and communications, which ensure blood circulation from one system to another. Veins of small and medium caliber, as well as some large vessels, contain valves on the inner lining. The blood vessels of the lower extremities have a small number of valves, so when they weaken, pathological processes begin to form. The veins of the cervical region, head and vena cava do not contain valves.
The venous wall consists of several layers:
Related article:What is the difference between a vein and an artery
- Collagen (resist internal blood flow).
- Smooth muscle (contraction and stretching of the venous walls facilitates blood circulation).
- Connective tissue (provides elasticity during body movement).
Venous walls have insufficient elasticity, since the pressure in the vessels is low and the blood flow rate is insignificant. When the vein is stretched, outflow is impeded, but muscle contractions help the fluid move. An increase in blood flow speed occurs when exposed to additional temperatures.
Veins of the upper limb
Rice. 318. Superficial veins of the forearm and hand, right. Back surface. I-dorsal venous network of the hand; 2-intercephalic veins; 3-dorsal metacarpal veins; 4-medial saphenous vein of the arm; 5-subcutaneous venous network of the forearm; 6th and 7th lateral saphenous vein of the arm. Fig. 318. Superficial veins of the forearm and hand, right. Back surface. 1-retc venosum dorsale manus; 2-vv. intercapitales; 3-vv. metacarpeae dorsales; 4-v. basilica; 5-rete venosum subcutancLim antebrachii; 6.7-v. cephalica. Fig. 318. Superficial veins of right forearm and hand. Dorsal surface. I -dorsal venous network of hand; 2-intercapitular veins; 3-dorsal metacarpal veins; 4-basilic vein; 5-subcutaneous venous network of forearm; 6 and 7-cephalic vein. Rice. 319. Superficial veins of the forearm and hand, right. Palmar surface. 1st medial saphenous vein of the arm; 2-median vein of the forearm; 3-palmar venous network of the hand; 4-palmar digital veins; 5-superficial palmar venous arch; 6-lateral saphenous vein of the arm. Fig. 319. Superficial veins of the forearm and hand, right. Palmar surface. 1-v. basilica; 2-v. intermedia antebrchii; 3-rete venosum' palmarc; 4-vv. digitales pal-mares; 5-arcus venosus pal-maris superficialis; 6-v. cephal-ica. Fig.319. Superficial veins of right forearm and hand. Palmar surface. I -basilic vein; 2-median vein of forearm; 3-palmar venosons network of hand; 4-palmardigital veins; 5-superficial venous palmar arch; 6-cephalic vein. Rice. 320. Deep palmar venous arch and its tributaries, li deep palmar venous arch; 2-palmar metacarpal veins; 3-deep palmar arterial arch; 4-venous network of the wrist; 5-ulnar veins; 6-radiate veins; 7 radiate artery; 8 loc artery. Fig. 320. Deep palmar venous arch and its tributaries. 1-arcus venosus palmaris profundus; 2-vv. meiacarpales palmares; 3-arcus arteriosus palmaris protundus; 4-rete venosum carpi; 5-vv. ulnares; 6-vv. radials; 7-a. radialis; 8-a. ulnaris. Fig. 320. Deep palmar venosous arch and its inflows. 1-deep venosus palmar arch; 2-palmar safa! veins; 3-deep palmar arterial arc; 4-venosous network of wrist;5-ulnar veins; 6-radial veins; 7-radial artery; 8-ulnar artery. Rice. 321. Lateral and medial saphenous veins of the arm, right. Front view. I-lateral saphenous vein of the arm; 2-median ulnar vein; 3-medial saphenous vein of the arm; 4-intermediate vein of the forearm. Fig. 321. Lateral and medial saphenous veins of the arm, right. Front view. 1-v. cephalica; 2-v. mediana cubiti; 3-v. basilica; 4-v. intermedia antebrachii. Fig. 321. Cephalic and basilic veins of the right arm. Frontal view. 1-cephalic vein; 2-median cubital vein; 3-basilic vein of arm; 4-intermediate antebrachial vein.
Rice. 322. Deep foam of the right hand. Front view. 1-axillary artery; 2-sub-muscular yen; 3-subscapular vein; 4-trunks of the brachial plexus; 5-medial saphenous vein of the arm; 6-brachial artery; 7-brachial veins; 8th median nerve (cut off); 9-median vein of the elbow; 10-lateral saphenous vein of the arm; 11-aponeurosis of the biceps humerus condyle; 12-biceps brachii: 13-major muscle; 14 deltoid muscle; 15th pectoral muscle (cut off). Fig. 322. Deep veins of the arm, right. Front view. 1-a. axillaris; 2-v. axillaris; 3-v. sub-scapularis; 4-trunci plexus brachiales; 5-v. basilica; 6-a. brachialis; 7-vv. brachiales; Xn. meduanus (cut off); 9-v. mediana cubiti; 10-v. cephalica; ll-aponeu- 10 rosus m. bicipitis brahii; 12 am. biceps brachii; 13.00 pectoralis major; 14-m. deltoideus; 15-m. pectoralis minor (cut off). Fig. 322. Deep vein of right arm. Anterior aspect. I-axillary artery; 2-axillary vein; 3-subscapular vein; 4-trunks of brachial plexus; 5-basilic vein; 6-brachial artery; 7-brachial veins; 8-median nerve (removed); 9-median cubital vein; Yu-cephalic vein: I l-bicipital aponeurosis; 12-biceps biceps brachii; 13-pectoralis major; 14-deltoid; 15-pectoral minor (removed).
Risk factors in the development of vascular pathologies
The vascular system of the lower extremities is subjected to high stress during walking, running and prolonged standing. There are many reasons that provoke the development of venous pathologies. Thus, non-compliance with the principles of rational nutrition, when fried, salty and sweet foods predominate in the patient’s diet, leads to the formation of blood clots.
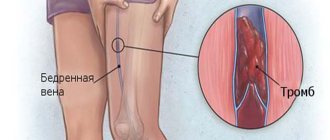
Thrombosis is primarily observed in small-diameter veins, but when the clot grows, parts of it enter the main vessels that are directed to the heart. In severe cases of pathology, blood clots in the heart lead to cardiac arrest.
Physical inactivity promotes congestion in blood vessels
Causes of venous disorders:
- Hereditary predisposition (inheritance of a mutated gene responsible for the structure of blood vessels).
- Changes in hormonal levels (during pregnancy and menopause, there is an imbalance of hormones that affects the condition of the veins).
- Diabetes mellitus (consistently elevated levels of glucose in the bloodstream lead to damage to the venous walls).
- Abuse of alcoholic beverages (alcohol dehydrates the body, resulting in thickening of the blood flow with further formation of clots).
- Chronic constipation (increased intra-abdominal pressure, complicates the outflow of fluid from the legs).
Varicose veins of the lower extremities are a fairly common pathology among the female population. This disease develops due to a decrease in the elasticity of the vascular wall when the body is exposed to intense stress. An additional provoking factor is excess body weight, which leads to stretching of the venous network. An increase in the volume of circulating fluid contributes to additional stress on the heart, since its parameters remain unchanged.
Veins of the lower extremities
Veins are made in the form of tubes with thin walls that have the property of stretching. This feature in terms of physiological conditions is quite limited by a dense frame. It has collagen and reticulin fibers. The lower limbs of a person are saturated with three venous systems. These are the superficial, deep and perforating vein system. A greater outflow of blood, namely 85-90%, is carried out through the deep venous system. The volume of blood located in the superficial veins is 10-15%.
Those veins of the lower extremities that are on the surface lie in the layer of subcutaneous tissue and form connections with each other and with the deep veins. The venous system lying on the surface includes two saphenous veins.
The great saphenous vein is one of the longest veins present in the human body. It is equipped with several pairs of valves. The diameter of this vein ranges from 3 to 5 mm. The valves of the great saphenous vein are bicuspid. Depending on the level of functional load, valves are distributed in one or another vascular segment. The leaflets of the venous valves are formed by a connective tissue base, the frame of which is expressed by a spur of the internal elastic membrane.
The valve leaf has two surfaces. Each of them is tightly wrapped in endothelium. They originate in front of the middle ankle, which belongs to the foot, and then continue their movement to the subcutaneous tissue and inguinal fold. At this point it unites with the femoral vein. There are cases when the large saphenous veins, located on the thigh and, accordingly, the lower leg, are expressed by several trunks. This vein includes a huge number of tributaries that take blood fluid from the lower extremities, the external genital organs, and the frontal wall of the peritoneum, as well as the skin and tissue of the buttocks area.
The small saphenous vein is considered part of the lateral marginal vein related to the foot. In the area of the shin it runs along the posterior zone and inside the popliteal fossa it reaches the popliteal vein. There are cases when the vein in question goes higher than the popliteal fossa, and then enters the femoral, large saphenous vein, or even the deep vein, which is part of the thigh. A large number of both cutaneous and saphenous veins enter the small saphenous vein; a considerable proportion of them enter here in the lower region of the leg. The small saphenous vein drains blood from the lateral and at the same time posterior zone of the leg.
The veins of the lower extremities include three pairs of deep veins, namely the tibial, that is, the anterior and posterior, as well as the peroneal vein. The main load during the outflow of blood from the periphery falls on the posterior great tibial veins, into which the small tibial veins enter. The deep veins of the dorsum of the foot originate in the area of the metatarsal veins of this part of our body, then the blood passes to the frontal great tibial veins. At almost the highest point of the leg, both large tibial veins join, creating the popliteal vein. It is a small blood trunk that is formed by the union of deep veins. Along its entire path, in addition to the small saphenous vein, it admits the veins of the knee joint, which have pairs. This vein goes higher and then enters the femoropopliteal canal. It is here that its name changes to the femoral vein. Just above the inguinal fold it transforms into the external iliac vein, and then runs to the heart.
The venous system of the surface of the lower extremities comes into contact with the deep veins as perforators. They are venous vessels with thin walls and varied diameters. It can be either a fraction of a millimeter or two millimeters, but its length always remains the same - 15 cm. The valves in the perforators are placed in such a way that they allow blood to move from the superficial veins to the deep ones. Almost half of these foot veins are not equipped with valves, so blood can easily move from the foot to the superficial veins and also do the opposite. This feature is subject to functional load and physiological conditions. Perforating veins are divided into direct and indirect.
The straight veins of the lower extremities are vessels that unite the deep and superficial veins. There are few such veins, but they are quite large and are located in the distal areas of the limbs. Indirect perforators are considered the unifying part of any of the saphenous and muscular veins, which in turn is in contact with the deep vein. There are a large number of indirect veins in the lower parts of our body. They are, however, very small and are located in the muscle mass area. Each of the perforators mostly contacts not with the main trunk of the saphenous vein, but with any of its tributaries.
Vascular pathologies
Impaired functioning of the venous-vascular system leads to thrombosis and varicose veins. The most common diseases that people experience are:
- Varicose veins. It manifests itself as an increase in the diameter of the vascular lumen, but its thickness decreases, forming nodes. In most cases, the pathological process is localized in the lower extremities, but cases of damage to the veins of the esophagus are possible.
- Atherosclerosis. A fat metabolism disorder is characterized by the deposition of cholesterol formations in the vascular lumen. There is a high risk of complications: when the coronary vessels are damaged, myocardial infarction occurs, and damage to the cerebral sinuses leads to the development of a stroke.
- Thrombophlebitis. Inflammatory damage to blood vessels, resulting in complete blockage of its lumen by a thrombus. The greatest danger lies in the migration of a blood clot throughout the body, as it can provoke severe complications in any organ.
The pathological dilatation of small-diameter veins is called telangiectasia, which manifests itself as a long-term pathological process with the formation of stars on the skin.
The first signs of damage to the venous system
The severity of symptoms depends on the stage of the pathological process. As damage to the venous system progresses, the severity of the manifestations increases, accompanied by the appearance of skin defects. In most cases, disruption of venous outflow occurs in the lower extremities, since they bear the heaviest load.
Early signs of impaired blood circulation in the lower extremities:
- strengthening of the venous pattern;
- increased fatigue when walking;
- painful sensations accompanied by a feeling of squeezing;
- severe swelling;
- inflammatory phenomena on the skin;
- vascular deformation;
- cramping pain.
At later stages, increased dryness and pallor of the skin is observed, which can later be complicated by the appearance of trophic ulcers.
How to diagnose pathology?
Diagnosis of diseases associated with venous circulation disorders involves the following studies:
- Functional tests (allow you to assess the degree of vascular patency and the condition of their valves).
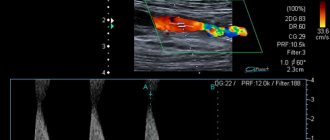
- Duplex angioscanning (real-time assessment of blood flow).
- Dopplerography (local determination of blood flow).
- Phlebography (carried out by introducing a contrast agent).
- Phleboscintiography (the introduction of a special radionuclide substance makes it possible to identify all possible vascular abnormalities).
Duplex scanning technique of venous circulation in the lower extremities
The condition of the superficial veins is examined by visual inspection and palpation, as well as by the first three methods from the list. The last two methods are used to diagnose deep vessels.
The venous system has fairly high strength and elasticity, but exposure to negative factors leads to disruption of its activity and the development of diseases. To reduce the risk of pathologies, a person needs to follow recommendations for a healthy lifestyle, normalize exercise, and undergo timely examination by a specialist.