Arteries of the head and neck
On the sides of the neck you can feel the pulsation of the carotid arteries, which carry blood to the head.
The head and neck are supplied with blood through two common carotid arteries, which rise up on each side of the neck.
Together with the internal jugular vein and the vagus nerve, they are enclosed in a protective sheath of connective tissue called the carotid vagina. The common carotid arteries have different origins at the base of the neck: the left one rises directly from the aortic arch, and the right one from the brachiocephalic trunk.
Vessels of the anterior neck
In the front of the neck there are paired carotid arteries and the same paired jugular veins.
Common carotid artery (CAA)
It is divided into right and left, located on opposite sides of the larynx. The first one arises from the brachiocephalic trunk, so it is slightly shorter than the second one, which arises from the aortic arch. These two carotid arteries are called the common carotid arteries, and they account for 70% of the total blood flow going directly to the brain.
The internal jugular vein runs next to the CCA, and the vagus nerve is located between them. The entire system consisting of these three structures makes up the neurovascular bundle of the neck. Behind the arteries is the cervical section of the sympathetic trunk.
OCA does not produce branches. And upon reaching the carotid triangle, approximately at the level of the 4th cervical vertebra, the internal and external are divided. On both sides of the neck. The area where bifurcation occurs is called bifurcation. This is where the artery dilates - the carotid sinus.
On the inside of the carotid sinus is the carotid glomus, a small glomerulus rich in chemoreceptors. It reacts to any changes in the gas composition of the blood - the concentration of oxygen, carbon dioxide.
External carotid artery (ECA)
Located closer to the front surface of the neck. During its movement up the neck, the NSA gives off several groups of branches:
- anterior (directed to the front of the head) – superior thyroid, lingual, facial;
- posterior (directed to the back of the head) - occipital, posterior auricular, sternocleidomastoid;
- middle (terminal branches of the ECA, division occurs in the temple area) - temporal, maxillary, ascending pharyngeal.
The terminal branches of the ECA are divided into even smaller vessels and supply blood to the thyroid, salivary glands, occipital, parotid, maxillary, temporal regions, as well as facial and lingual muscles.
Internal carotid artery (ICA)
Performs the most important function in the general blood flow, which is provided by the vessels of the head and neck - blood supply to a larger area of the brain and the human visual organ. It enters the cranial cavity through the carotid canal and does not produce branches along the way.
Once in the cranial cavity, the ICA bends (damper), penetrates the cavernous sinus and becomes part of the arterial circle of the cerebrum (circle of Willis).
Branches of the ACA:
- ophthalmic;
- forebrain;
- middle cerebral;
- back connecting;
- anterior villous.
Jugular veins
These neck vessels carry out the reverse process - the outflow of venous blood. There are external, internal and anterior jugular veins. Blood enters the external vessel from the back of the head closer to the ear area. And also from the skin above the shoulder blade and from the front area of the face. Going lower, not reaching the clavicle, the IAV connects with the internal and subclavian. And then the inner one develops into the main one at the base of the neck and bifurcates into right and left.
The largest main vessel of the cervical spine is the IJV. It forms in the area of the skull. The main function is the outflow of blood from the vessels of the brain.
Most branches of the jugular veins bear names of the same name as the arteries. With those arteries that accompany it - lingual, facial, temporal... the exception is the mandibular vein.
Branching of arteries
The common carotid arteries divide at the level of the upper edge of the thyroid cartilage (Adam's apple) and form the internal and external carotid arteries. The internal carotid arteries penetrate the skull and supply blood to the brain. The external carotid arteries form branches that supply blood to the face and scalp.
Many branches of the external carotid artery have a wavy or loop-like course. This ensures the mobility of the vessels, and therefore when the mouth, larynx or pharynx moves, such as during swallowing, the vessels are not stretched or damaged.
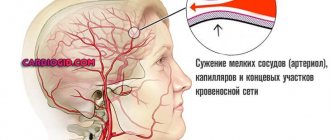
Symptoms of cervical vascular spasm
The manifestation of spasm of the cervical vessels is influenced by its intensity and localization. First of all, you need to focus on the pain syndrome.
With osteochondrosis of the spinal column, patients first experience some discomfort, a feeling of stiffness and a crunch in the neck. The pain appears after this and spreads to the back of the head, temples, arms, and shoulder girdle. With movements, for example, when turning or tilting the head, the pain intensifies. Then spasms of muscles and nerve endings occur, which manifests itself in a significant limitation of the mobility of the cervical spine.
With spasm of the cervical vessels, one of the main symptoms is the presence of a headache. It is most often localized in the occipital part. The pain can be of a different nature: dull, throbbing, aching, bursting with a feeling of pressure on the eyeballs, tightening (with muscle tension). Painful sensations of a shooting nature can manifest themselves in the shoulders and arms.
Also, with spasm of the cervical vessels, it is common to:
- blood pressure is disturbed;
- there is general weakness and a feeling of fatigue, trembling in the hands;
- sweating increases;
- darkens in the eyes;
- slight dizziness when moving the head;
- when coughing, the patient feels pain radiating to the brain;
- a pre-fainting state occurs.
Dizziness is especially pronounced in people with low blood pressure
Neurological symptoms of cervical vasospasm include disorders related to the functioning of the brain. Most often the patient has the following symptoms:
- the occurrence of tinnitus;
- vision deteriorates;
- gait becomes unsteady;
- memory deteriorates, concentration decreases;
- frequent mood changes;
- sleep is disturbed.
These symptoms manifest themselves in chronic pathologies. However, acute conditions are more dangerous by increasing intracranial pressure, tearing off cholesterol plaques, and their penetration into the brain - causing strokes.
Before taking measures to relieve cervical vascular spasm, it is necessary to confirm the alleged diagnosis.
Carotid angiography
An injection of contrast agent and subsequent series of x-rays allow the branching of the common carotid artery to be observed. This procedure is called carotid angiography.
Angiography is used to look at blood vessels and also to identify any abnormalities such as blockages in the carotid arteries. The accumulation of fatty deposits on artery walls, seen in atherosclerosis, can sometimes be found at the site of the division of the common carotid artery. With the help of surgery, fatty deposits can be carefully removed without damaging the walls of the blood vessels. This surgery, known as a carotid endarterectomy, effectively improves blood supply to the head and neck and reduces the risk of stroke.
Another abnormality that can be detected using angiography is an arterial aneurysm, in which a spherical dilatation is found in the wall of the vessel.
Diagnostics
Previously, vasoconstriction was considered a disease of older people, but recently this disease can also attack young people. If the disease is nevertheless detected, it requires long-term and systemic medication.
When you contact a therapist , the first thing you will do is prescribe a diagnostic test. After this, you will need to consult a neurologist and cardiologist:
- At the first examination, the doctor can determine noise in the carotid arteries and malfunctions of the entire nervous system.
- Next you need to undergo an ultrasound scan. This will allow you to find out whether there are plaques and blood clots in the vessels, as well as at what speed the blood moves and how clean the vessels are.
- If these studies are not enough, the specialist will prescribe additional procedures to the patient: SCT angiography or MR angiography. After this diagnosis, you can see the brain and carefully examine the arteries.
Important! Never start treatment without diagnostic tests. It is important to understand that you have a narrowing of blood vessels. Since osteochondrosis exhibits similar symptoms, however, the treatment will be completely different.
Veins of the head and neck
Veins are distributed throughout the head and neck like arteries. Many veins have the same names.
Blood flows from the head and neck back to the heart through the internal jugular veins, located on either side of the neck. Together with the common carotid arteries, the internal jugular veins lie in the carotid vagina.
Unlike the veins in the rest of the body, the veins in this area do not have valves, and the return of blood to the heart is carried out by gravity and negative pressure in the chest.
Superficial veins (located close to the surface) are often visible during physical activity, or, for example, you can see the veins standing out in the neck of singers.
Treatment of neck vasospasm
Based on the results of the diagnostic study, treatment of the head/neck vessels is prescribed, where applicable:
- medicines;
- physiotherapeutic procedures;
- traditional medicine as an adjuvant therapy.
As a special recommendation, experts advise the patient to refuse physical therapy during an exacerbation of the disease.
Pharmacological drugs
When the pain syndrome intensifies from the slightest movement of the head or coughing attacks, and hypothermia is considered the cause of the pain, you can try to help yourself stop this condition. To do this, you need to leave your work and lie in a warm bath. Spend the next hours in bed. Consultation with a specialist will be required if this method does not work and the pain does not stop.
- To provide quick assistance in eliminating spasms, intravenous infusions of No-shpa, Renalgan, and Baralgin are recommended.
- Prescription of antidepressants may follow when the patient is diagnosed with nervous strain.
- To improve metabolic processes in neurons, it is recommended to take nootropics with hopantenic acid. Among them, the drug Pantogam effectively restores brain function.
- Hypertensive patients are prescribed medications that regulate blood pressure, where the doctor selects the medication and determines the dose.
- If atherosclerosis of the cerebral vessels of the head is detected, Spazoverine, Drotaverine, Papaverine are suitable for relieving spasms and improving blood circulation.
Among herbal preparations, it is recommended to use adaptogens to relieve headaches. In addition to eliminating pain, these remedies have a beneficial effect on the entire body. They help strengthen the defense mechanism and stimulate the endurance of the human body:
- Ginseng has gained well-deserved popularity in the complex treatment of spinal pathologies. It is also often recommended for use in diseases of the digestive tract, thrombosis, and diabetes. For general strengthening, it is recommended to take the drug during the off-season in the morning, diluting two tablespoons with water before meals.
- Schisandra also belongs to the category of strong herbal preparations for the treatment of hypertension and depressive conditions.
The principles of relieving vascular spasm in a child are the same as in adults. A light relaxing massage affecting the neck muscles and collar area can help with this. You can also rub your child's forehead and ears with light movements. You can place a cool compress on your neck. To calm down, you can drop a couple of drops of essential oil on your child’s wrist. Lavender and jasmine oils best help with vasospasm. You can also give the child a glass of warm water with honey and put him to bed. If symptoms do not go away, you should urgently call a doctor.
- How to relieve vasospasm
Traditional medicine
Some remedies recommended by traditional healers can also help with vascular spasm.
- By placing a fresh cabbage leaf on your forehead, you can cope with ailments of this nature.
- By rubbing garlic on painful areas on the head, you can relieve throbbing pain, especially in the temporal region. You can use lemon balm oil for the same purpose.
- A decoction of calendula + St. John's wort significantly improves the patient's condition. The raw materials are poured in equal parts with water and brought to a boil. Leave for a quarter of an hour and drink a third of a glass after straining. The herbal decoction helps strengthen the blood vessels in the brain.
- An infusion of thyme will help relieve spasms. A spoonful of crushed raw materials is poured with boiling water (no more than a glass), infused and cooled. After straining the medicinal infusion, drink in small sips.
- A rosehip decoction will help prevent spasms from occurring if the patient drinks a glass of healing liquid every day after waking up.
Jugular vein
There are only slight differences in the location of the internal jugular vein, so this vein is used to control central venous pressure (blood pressure inside the right atrium of the heart). A catheter (hollow tube) is inserted into a vein and directed towards the heart. The other end of the catheter is connected to a sensor that measures pressure. This procedure can also measure blood volume.
In addition to the veins through which blood flows from the face, there is a system of emissary veins through which the venous sinuses (through which blood flows from the brain) and the veins of the scalp communicate. Together with diploic veins (located in the bones of the skull), emissary veins represent a potential route for infection to spread from the surface of the head to the brain.
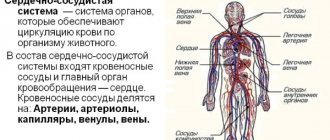
general characteristics
Aneurysms of the cervical vessels represent a limited expansion in the area of the most thinned and stretched vascular segment.
The arteries and veins of the neck are distinguished by their anatomical proximity to each other and a large number of anastomoses, which causes a relatively high frequency of mixed lesions and erased clinical picture. Women get sick 2 times more often than men.
Distinctive features:
- High frequency of arteriovenous forms (up to 15-20%);
- Effect on cerebral circulation;
- Rapid thrombus formation;
- For small sizes – rapid calcination;
- Proximity of cardiac structures;
- High risk of pulmonary embolism.
Prevention measures
To prevent spasm of blood vessels in the neck and brain, you must:
- Control emotions, monitor the state of the nervous system, preventing it from overstraining.
- Completely give up bad habits, spend at least 2 hours outdoors every day, follow a daily routine, toughen up, and don’t forget about relaxation.
- Establish a sleep schedule - the body should rest at least 8 hours a day.
- Adjust your diet: give up unhealthy foods, give preference to raw vegetables, fruits, berries, herbs (especially parsley), garlic, carrots, cabbage, and green tea as a drink. All of the products listed will help blood vessels maintain their elasticity.
- Drinking black tea, coffee, fatty and smoked foods is not permissible. Pickles and spicy foods should be consumed in limited quantities.
- Hardening methods such as taking a contrast shower or dousing your feet first with cool and then cold water will help strengthen the vascular system.
Thus, if a spasm of the cervical vessels occurs, you can try to help yourself, but only for temporary relief. In conditions caused by serious disorders in the body, only a doctor should carry out further diagnosis and prescribe adequate treatment.
Causes of development and risk groups
Etiological factors:
- Arrosion of the vessel;
- Tuberculosis;
- Vasculitis;
- Genetic syndromes;
- Syphilis;
- Atherosclerosis;
- Arterial hypertension;
- Congenital tortuosity of blood vessels.
Persons at risk are:
- Having a cholesterol level above 6.0 mmol/l;
- Over 50 years old;
- Suffering from diabetes and other metabolic diseases;
- Having suffered a transient ischemic attack or cardiac ischemia;
- With a family history;
- Suffering from atrial fibrillation and heart defects.
Characteristics and symptoms
Let's consider different types of aneurysms of the neck vessels and their symptoms in adults, differences in diagnostic signs and treatment tactics.
Aneurysm of the internal jugular vein in the neck
ICD-10 code: I72.8.
Prevalence: 7.5-9%.
Distinctive symptoms : mild asymmetric painless bulging in the neck, dry cough, pain when turning the head, fainting (compression of the common carotid artery).
Diagnosis : cyanosis and pastiness of the face and neck, headaches, continuous vascular noise on auscultation. Ultrasound - limited expansion with signs of thrombus formation, thrombophlebitis. The vein wall may be collapsed. CT scan (MRI) - hydrocephalus, local cerebral edema, thrombus and calcifications in the vein wall.
Treatment : antiplatelet agents, anticoagulants, resection with prosthetics (prosthesis from a segment of a peripheral vein).
External jugular vein
ICD-10 code: I72.8.
Prevalence: 1.2-4%.
Distinctive symptoms : swelling of the face and neck, swelling of the eyelids, difficulty in nasal breathing, enlarged tongue, congestion and tinnitus.
Diagnostics : swelling and redness of half the face without signs of inflammation, ultrasound of the neck vessels - thrombosis of the enlarged area, thinning and calcification of the vein wall, signs of thrombophlebitis. MRI (CT) - swelling of half the face and neck, calcifications, thrombosis.
Treatment : antiplatelet agents, anticoagulants, endovascular embolization. Resection is rarely performed.
Anterior jugular vein
ICD-10 code: I72.8.
Prevalence: 0.7-2.2%.
Distinctive symptoms : compression of the lobes or isthmus of the thyroid gland (concomitant thyroiditis), swelling of the anterior surface of the neck, hoarseness, swelling of the tongue. The course is often asymptomatic.
Diagnosis : Ultrasound of neck vessels - local protrusion of the PVV, involvement of small arteries (arteriovenous form), signs of arrosion or thrombophlebitis (rarely).
Treatment : symptomatic (blood pressure control), antiplatelet agents, anticoagulants, endovascular embolization.
Arteriovenous aneurysms
ICD-10 code: I72.8.
Prevalence: 9-12.4%.
Distinctive symptoms : asymptomatic, rapid calcification.
Diagnosis : incidental discovery on ultrasound (detecting a vascular anastomosis with limited protrusion and calcification), the diameter rarely exceeds 3 mm. CT (MRI) scans are not performed.
Treatment : blood pressure control, antiplatelet medications. If enlarged, endovascular embolization is performed.
Dilation of the subclavian arteries
ICD-10 code: I72.1.
Prevalence: 13.6%.
Distinctive symptoms : compression of the nerves and veins of the shoulder girdle, pallor and decreased sensitivity of the upper limb (paresthesia, numbness). Local swelling and pain in the collarbone area, spreading to the shoulder and shoulder blade. In case of rupture - acute ischemia of the upper limb, in the absence of treatment - mutilation (self-amputation).
Diagnosis : complaints of pain behind the collarbone and in the upper limb, numbness and swelling of the arm, decreased muscle strength. Angiography - local bulging of the vascular wall, compressing the clavicle, brachial nerve plexus, subclavian vein. Ultrasound – type and size of protrusion, thinning of the vascular wall, focal microcalcifications. CT (MRI) - thrombosis, swelling of the shoulder girdle, compression of the periosteum of the clavicle and nerve trunks.
Treatment : clipping, resection. Before the intervention, stabilization of blood pressure and prevention of thrombosis are carried out.
Carotid arteries
ICD-10 code: I72.0.
Prevalence: 32-34%.
Distinctive symptoms : pulsating bulge along the anterolateral surface of the neck, disturbances of consciousness, loss of visual fields, hypertension, cough, pain when eating, migraine, decreased cognitive function, if ruptured - stroke, paralysis.
Diagnosis : complaints of fainting, bursting headaches, convulsions, memory loss. Auscultation – vascular murmur. Blood pressure is increased. Angiography – deformation and tortuosity of the vascular wall, local expansion, defect in contrast filling, leakage of contrast into surrounding tissues. MRI (CT) – thrombosis, perivascular edema of soft tissues, thinning of the vascular wall, compression of the upper mediastinum.
Treatment : surgical (resection, embolization, clipping). Preparation for surgery - antihypertensive, nootropic, vasodilator drugs.
You can find all the details about carotid artery aneurysm in this article.
Vertebral artery
ICD-10 code: I72.6.
Prevalence: 7.6-8%.
Distinctive symptoms : difficulty swallowing, paralysis and atrophy of half the tongue, speech disorders, numbness of the lower extremities, coordination disorders, decreased temperature and pain sensitivity.
Diagnosis : complaints of occipital pain, vestibular and sensory disorders. Angiography – tortuosity, thinning of the vascular wall, thrombosis of the expanded area, signs of arrosion. CT (MRI) – compression of the spinal cord roots, local edema, calcifications, in case of complications – area of hemorrhagic impregnation.
Treatment : pathogenetic (blood pressure control, taking statins), surgical (resection, embolization, clipping).
Basilar artery
ICD-10 code: I72.5.
Prevalence: 15-17%.
Distinctive symptoms : paralysis of the eyeballs, paresis or paralysis of the oculomotor nerve. Vertical nystagmus. In case of rupture - blindness, paralysis, stroke.
Diagnosis : complaints of visual impairment, dizziness, headaches. Angiography – tortuosity of the vascular contour, filling defect and leakage of contrast in the perivascular zone. CT (MRI) - focal bulge with signs of thrombus formation, microcalcifications, in case of complications - stroke focus, hydrocephalus, hemorrhage in the brain or lateral ventricles.
Treatment : conservative (beta blockers, statins, antiplatelet agents), surgical removal.
Source: oserdce.com
Signs of vasoconstriction in the neck
Since the functionality of the cardiovascular system consists of compression and relaxation of blood vessels, the nature of which is constant. It is not difficult to guess that this process must have a leader who makes decisions about the time and place of compression/expansion of the blood vascular segment. This role in the human body is assigned to the surface of the brain - its cortex. The control tool is neurohormonal regulation, which serves as a natural blood flow mechanism. In normal condition, the operation of the system does not pose a threat to health. However, no one is immune from the occurrence of vasospasm, a situation when the vessels undergo a sharp sequential compression. This can happen for many reasons...
First symptoms
- Compression of a vessel during muscle spasm;
- constriction of blood vessels in the cold;
- physical pressure on the vessels during intervertebral hernia / cervical osteochondrosis.
Whatever the cause of the sharp narrowing of the vessel, it should be stopped as quickly as possible, since this condition is dangerous due to the onset of a lack of oxygen for the brain.
Development of brain asphyxia
Practically no different from the symptoms of general oxygen starvation of the brain, which does not pose an acute threat to the patient’s life, the indicators of the development of vasospasm will be as follows:
- Aching pain in the head, knocking in the temporal zone even with slight movement, prolonged mental/physical work contribute to an increase in pain, and at rest the pain decreases. Pain is usually observed in each of the areas of the skull, especially at the top of the head.
- Slightly dizzy, worsening when turning the head. However, if the patient suffers from low blood pressure and often suffers from migraines, the pain syndrome will become more pronounced and may be accompanied by fainting/disorientation/flickers in the eyes.
- General weakness, accompanied by trembling in the limbs as if severely hungry.
If the patient does not receive help within the next five or six hours, negative symptoms begin to increase. This is due to an increase in intracranial pressure against the background of the continued flow of blood with disruption of its outflow.
- The headache will become stronger and acquire a bursting/pressing character;
- pressure will increase in the apple of the eye, which will be manifested by the appearance of a red veil, objects will acquire blurry outlines, and a halo will appear when looking at the light.
- uncontrollable nausea and vomiting;
- increased sweating, desire to urinate;
- fainting;
- leg cramps.
The second stage of spasm of the cervical vessels is dangerous for the development of hemorrhagic stroke if there are weak areas of the vascular walls in the tissues of the brain of the head.
If a spasm occurs and the lumen of the vessel narrows, the brain receives less oxygen. This is expressed in loss of consciousness, headache, nausea and vomiting. Thus, the brain signals about problems in the body. Angiospasm was previously considered a disease of older people, but the disease is becoming “younger” from year to year. The reason is constant stress, modern lifestyle and poor environmental conditions. Heredity and past diseases play an important role in this.
- Vascular angiospasm (brain, eyes, limbs)
Anatomy of the head and neck: brief information
To begin with, it is worth considering general information. Before studying the veins of the head and neck, you can familiarize yourself with the anatomical features.
As you know, the head is located at the top of the spinal column. The occipital bone of the skull articulates with the atlas (the first cervical vertebra) in the area of the foramen magnum. The spinal cord passes through this hole - the structure of the skeleton ensures the integrity of the central nervous system.
The skeleton of the head and neck consists of the skull, cervical spine, auditory ossicles, and hyoid bone. The skull itself is conventionally divided into parts:
- brain part (consists of the frontal, occipital ethmoid, sphenoid, as well as paired temporal and parietal bones);
- facial part (consists of the vomer, lower jaw, as well as paired zygomatic, palatine, maxillary, lacrimal, nasal bones).
The skeleton is covered with muscles that allow flexion, rotation and extension of the neck. Of course, when considering anatomical features, one cannot fail to mention nerves, brain, glands, blood vessels and other structures. By the way, we will look more closely at the veins of the head and neck.
Vessels of the posterior neck
In the area of the cervical spine there is another pair of arteries - the vertebral ones. They have a more complex structure than the carotid ones. They depart from the subclavian artery, follow behind the carotid arteries, and penetrate in the area of the 6th cervical vertebra into the canal formed by the openings of the transverse processes of the 6th vertebrae. After leaving the canal, the vertebral artery bends, passes along the upper surface of the atlas and enters the cranial cavity through the large posterior foramen. Here the right and left vertebral arteries merge and form a single basilar artery.
The vertebral arteries give off the following branches:
- muscular;
- spinal;
- posterior spinal;
- anterior spinal;
- posterior cerebellar inferior;
- meningeal branches.
The basilar artery also forms a group of branches:
- artery of the labyrinth;
- inferior anterior cerebellar;
- pontine arteries;
- cerebellar superior;
- midbrain;
- posterior spinal.
The anatomy of the vertebral arteries allows them to supply the brain with 30% of the blood it needs. They supply the brain stem, occipital lobes of the hemispheres and the cerebellum. This entire complex system is usually called vertebrobasilar. “Veterbro” – associated with the spine, “basilar” – with the brain.
The vertebral vein begins at the occipital bone - another of the vessels of the head and neck. It accompanies the vertebral artery, forming a plexus around it. At the end of its path in the neck it flows into the brachiocephalic vein.
The vertebral vein intersects with other veins of the cervical spine:
- occipital;
- anterior vertebral;
- accessory vertebral.
Lymphatic trunks
The anatomy of the vessels of the neck and head also includes lymphatic vessels that collect lymph. There are deep and superficial lymphatic vessels. The first ones run along the jugular vein and are located on both sides of it. The deep ones are located in close proximity to the organs from which lymph flows.
The following lateral lymphatic vessels are distinguished:
- retropharyngeal;
- supraclavicular;
- jugular
Deep lymphatic vessels collect lymph from the mouth, middle ear, and pharynx.
Internal jugular vein
This is a fairly large vessel that collects blood from almost all areas of the neck and head. It begins at the level of the jugular foramen and is a direct continuation of the sigmoid sinus.
Slightly below the source of the vessel there is a small formation with expanded walls - this is the superior bulb of the jugular vein. This vessel runs along the internal carotid artery, and then passes behind the common carotid artery (this vessel lies in the same fascial sheath as the carotid artery and vagus nerve). Slightly above the place where the jugular vein merges with the subclavian vein, there is another extension with two valves - this is the inferior bulb.
The sigmoid sinus, where this vessel actually begins, receives blood from the entire system of dural sinuses. In turn, blood is carried to them by the cerebral veins, as well as the vessels of the labyrinth and ophthalmic veins.
Diploic veins
These are wide vessels with thin walls. They do not have valves. The vessels begin in the area of the spongy substance of the cranial vault and collect blood from the inner surface of the bones. Inside the cranial cavity, these veins communicate with the sinuses of the dura mater and meningeal vessels. Outside the skull, these vessels connect with the veins of the outer integument.
The frontal veins are the largest diploic vessels - they flow into the sagittal sinus. This group also includes the anterior temporal vein, which carries blood to the sphenoparietal sinus. There are also posterior temporal and occipital diploic veins, which drain into emissary vessels.
Features of blood flow through emissary vessels
Emissary veins provide connection between the sinuses of the dura mater and vessels located in the tissues outside the skull. By the way, these vessels pass through small bony valves and exit to the outside of the skull, where they communicate with other vessels.
- The parietal emissary vein, which connects the superior sagittal sinus with the external vessels. In their skulls it comes out through the parietal opening.
- The mastoid emissary vein exits through the opening of the mastoid process. It connects the sigmoid sinus with the occipital vein.
- The condylar vein leaves the skull through the condylar canal (it is part of the occipital bone).
Brief description of the superior and inferior ophthalmic veins
The superior ophthalmic vein is the larger one. It includes vessels into which blood flows from the tissues of the forehead, nose, upper eyelid, membranes and muscles of the eyeball. Approximately at the level of the medial corner of the eye, this vessel communicates with the facial vein through an anastomosis.
Blood from the vessels of the lower eyelid and adjacent eye muscles drains into the inferior vein. This vessel runs along the lower wall of the orbit, almost under the optic nerve, and then flows into the superior ophthalmic vein, which carries blood to the cavernous sinus.
Extracranial tributaries
The internal jugular vein is quite large and collects blood from many vessels.
- Pharyngeal veins, which collect blood from the pharyngeal plexus. This vascular structure collects blood from the tissues of the pharynx, auditory tube, occipital part of the dura mater, and soft palate. By the way, the pharyngeal vessels are small and do not have valves.
- The lingual vein, which is formed by the sublingual, deep and paired dorsal veins of the tongue. These structures collect blood from the tissues of the tongue.
- The thyroid vein (superior), which collects blood from the sternocleidomastoid and superior laryngeal veins.
- The facial vein communicates with the internal jugular at the level of the hyoid bone. This vessel collects blood from almost all tissues of the face. Small vessels drain into it, including the mental, supraorbital, angular, external palatine and deep facial veins. Blood also flows here from paired vessels, including the upper and lower labial, external nasal, as well as the veins of the parotid gland, upper and lower eyelid.
- The mandibular vein is considered a fairly large vessel. It begins in the area of the auricle, passes through the parotid gland, and then flows into the internal jugular vein. This vessel collects blood from the pterygoid plexus, the middle ear vein, as well as the middle, superficial and deep temporal vessels, the vein of the temporomandibular joint, and the anterior ear veins.
Structure and features of work
The distribution of superficial and deep vessels is represented by a large number. They provide high reliability of uninterrupted power supply to the tissues of the skull. The superficial ones include:
- upper outlet;
- inferior outlet;
- superficial average;
- superior anastomotic;
- lower anastomotic.
The deep cerebral veins are represented by a large list. They are divided into upper and lower.
The main task of deep venous vessels is to collect blood. Flowing from the basal ganglia, vascular plexuses and diencephalon.
The upper group includes the following veins:
- Lateral ventricle;
- internal brain;
- superior thalamostriatal.
Representatives of the lower group:
- Paired basal, formed from the vessels of the medulla oblongata, pons;
- large brain
Other types:
- Cerebellar;
- sinuses of the dura mater;
- superior inferior and sagittal sinus;
- straight, transverse, occipital sinus;
- sigmoid and sinus drainage.
The veins of the neck are divided into vessels of the anterior and posterior sections. The vascular network of the upper body has some differences with the base of the body. Since the arterial branches are not duplicated with the venous branches and are located completely differently.
Internal jugular vein
Refers to the anterior cervical region, like the outer one.
Anatomically located in the jugular foramen and occupies most of the space. It is the largest main vessel of the cervical spine.
IJVs are presented in the form of slit-like channels, placed in a connective tissue membrane of increased density.
The lumen of the vessel is constantly open, due to which the outflow of blood occurs continuously, preventing stagnation.
At the levels of the larynx, the PU of the internal section comes into contact with the carotid artery on both sides. The outflow of blood is carried out through the sinus system. From the left and right sides, the collected blood enters the superior vena cava.
The upper section is equipped with valves. Here there is a merger with the subclavian vascular system. The IJV is divided into intracranial and external cranial branches.
Ducts of the IJV:
- snail plumbing;
- pharyngeal;
- meningeal;
- lingual;
- superior thyroid;
- middle thyroid;
- sternocleidomastoid.
Diploic veins of the brain
Located in the diploic substance of the cranial bones, they are represented by a developed canal system.
There are no valves in the lumens of the vessels, since the outflow of blood occurs from the bones of the skull. Inside the cranium, they communicate with the meningeal and sinuses of the meninges. The outside is covered with emissary veins.
The group includes the following representatives of the venous system:
- Frontal diplodic;
- Anterior temporal diploic;
- Posterior temporal;
- Occipital.
Diploic veins of the brain are their own cerebral veins. They lie deep in the canals of the bone, originating from the spongy substance.
Emissary veins
The main function is to connect the venous vessels of the skin with deeply located vessels.
To perform its task, the emissary system passes through a series of cranial foramina. According to their localization, there is a classification:
- Occipital;
- mastoid;
- parietal;
- condylar.
The name corresponds to the location of the bones. The emissary veins are designated in the diagram as vessels of the systemic circulation of the head vault.
Superior and inferior ophthalmic veins
Due to the branched network, they connect with the facial, frontal and paranasal veins. As in previous cases, an inextricable connection is formed with the sinuses of the dura mater.
The vessels do not have a valve apparatus and therefore the blood flow can vary from facial to cavernous sinusitis. Due to this structure of the orbit, the upper and lower eyelids are susceptible to inflammatory processes.
Features of blood flow through the external jugular vein
This vessel is formed by the confluence of two tributaries, namely:
- anterior tributary (it forms an anastomosis with the mandibular vein);
- posterior (this tributary collects blood from the occipital and posterior auricular veins).
The external jugular vein forms approximately at the anterior edge of the sternocleidomastoid muscle. From here it follows along the anterior surface of the muscle, pierces the plate of the cervical fascia and flows into the confluence of the internal jugular and subclavian veins. This vessel has two paired valves. By the way, it also collects blood from the suprascapular and transverse veins of the neck.
Anterior jugular vein
When considering the superficial veins of the head and neck, one cannot fail to mention the anterior jugular vein. It is formed from small vessels that collect blood from the tissues of the chin area, follows down the front of the neck, and then penetrates into the space above the sternum.
At this point, the left and right veins are connected through a transverse anastomosis, resulting in the formation of the jugular venous arch. On both sides, the arch flows into the external jugular veins (left and right, respectively).
Optimal methods of therapy
How to relieve spasm of blood vessels in the head and neck? Sometimes you just need to take a lying position, relax, provide plenty of fresh air, and massage your neck. If the cause of the spasm is hypothermia, you should take a warm shower or bath.
For spasm of blood vessels in the head, treatment can be either medicinal or non-medicinal.
Currently, there are various medications that will help significantly improve your condition. But you should not self-medicate. For competent and effective therapy, medications must be prescribed by a doctor individually for each patient. The most commonly prescribed tablets for vasospasm in the head are:
| Valerian | Makes you feel better and has a calming effect |
| Ginkgo biloba | Normalization of blood circulation in the head |
| Papaverine | Emergency vasodilation |
| Statins | Keep the vascular system in normal condition, avoiding complications |
The main goal of non-drug treatment is to eliminate the pathology that caused the spasms. In the future, actions will be aimed at taking measures to rehabilitate the patient.
An important role is given to physiotherapeutic procedures: physical therapy, massage, relaxation exercises, sanatorium-resort therapy.
To prevent and improve the condition, it is worth doing regular physical exercise.
It is worth reviewing your diet and adjusting your nutrition. The optimal diet excludes fatty, smoked, salty foods, large quantities of sweets, and drinks containing caffeine. You need to give preference to natural low-fat dairy products, raw vegetables and fruits, and protein foods.
Prevention of pathology includes the need to strengthen blood vessels. In addition to regular exercise and proper nutrition, you should follow a few general recommendations:
| Drink the recommended amount of water per day |
| Temper yourself, take a contrast shower (helps improve blood circulation) |
| Avoid stressful situations and nervous tension |
| Give up bad habits |
Subclavian vessel
The subclavian vein is an unpaired vessel that arises from the axillary vein. This vessel passes along the surface of the anterior scalene muscle. It starts at approximately the level of the first rib and ends behind the sternoclavicular joint. It is here that it drains into the internal jugular vein. At the beginning and end of the subclavian vessel there are valves that regulate blood flow.
By the way, this vein does not have constant tributaries. Most often, blood enters it from the dorsal scapular and thoracic venous vessels.
As you can see, the tissues of the neck and head have a very developed venous network, which ensures the timely outflow of venous blood. However, if the functioning of certain organs is disrupted, natural blood flow may be disrupted.
Causes of spasm
The cause of pathologies of the cervical spine is:
- chronic ailments - this can be vegetative-vascular dystonia, diseases of the cardiovascular and excretory systems, malignant neoplasms, abnormalities in the thyroid gland, diabetes (of any type), as well as changes in blood pressure;
- lack of oxygen - if you often sit in a stuffy room that is crowded with people, the brain feels a lack of oxygen, which causes blood circulation to be impaired and spasms to occur;
- poor sleep (or sleep in small quantities) - for proper functioning of blood vessels, a person needs to sleep at least 7 hours a day;
- smoking - this bad habit prevents oxygen from moving through the vessels, which subsequently causes the vessels to narrow;
- hypothermia or overheating, frequent occurrence of stressful situations - such processes often cause vasoconstriction;
- atherosclerosis and osteochondrosis - this disease is characterized by fatty deposits, due to which the vessels of the neck and head narrow.
When is an ultrasound examination necessary?
You already know how the veins of the head and neck work. Of course, a violation of the outflow of blood is fraught with stagnation and dangerous complications, which primarily affect the functioning of the central nervous system. If you suspect various circulatory disorders, doctors recommend undergoing examinations. And ultrasound of veins today is one of the simplest, most accessible and informative tests.
In what cases are patients sent for such a procedure? The indications are as follows:
- periodic dizziness;
- frequent fainting;
- headache;
- increased cholesterol levels along with hypertension;
- constant weakness, fatigue;
- diabetes;
- suspicions of the presence of tumors, atherosclerotic plaques, blood clots and other formations that impair vascular patency;
- the procedure is carried out before surgery, as well as during one or another therapy, in order to monitor the effect of treatment.
Of course, in order to make an accurate diagnosis, additional tests and laboratory tests are carried out. It is worth noting that most often stagnation and disturbances in blood outflow are associated with thrombosis and atherosclerosis.
Treatment
Conservative methods of treating cervical artery stenosis are used only in the early stages of the pathology and in the absence of concomitant diseases.
In case of severe narrowing, only surgical intervention can save the patient’s life.
Drug therapy
Depending on the factors that narrow the vessels of the cervical spine, the drug treatment regimen may include the following drugs:
- Microcirculation correctors (Trental). Restore cerebral circulation, reducing the severity of neurological disorders.
- Neuroprotectors (Pantogam). The drugs increase the resistance of nerve cells to hypoxia, restore memory and normalize brain function.
- Vasodilators (Cinnarizine). For vertebral artery stenosis, you need to choose medications that have anti-inflammatory and antihistamine effects.
- Statins (Atorvastatin). They reduce cholesterol levels in the blood and initiate the process of breaking down fat deposits. These drugs are recommended to treat atherosclerosis.
Important information: How to treat venous congestion of the vessels of the brain (lungs) and whether it can be removed in the pelvis in women (men)
The treatment regimen also includes drugs that eliminate the signs of the underlying disease that caused the narrowing of the arteries. For osteochondrosis, chondroprotectors (Teraflex), nonsteroidal anti-inflammatory drugs (Diclofenac), and muscle relaxants (Mydocalm) are prescribed.
Physiotherapy
The following physiotherapeutic procedures are used in the treatment of the disease:
- magnetic therapy;
- ultrasonic influence;
- mineral baths;
- low-intensity laser irradiation;
- shock wave therapy.
The methods are aimed at improving blood supply to tissues, normalizing metabolism, eliminating swelling and pain.
Massage
Massage is used for stenosis caused by osteochondrosis. The method helps relax muscles, returns the vertebrae to the correct position, and restores blood circulation.
Manual massage techniques include rubbing, stroking, tapping and kneading. Movements begin in the head area, gradually moving towards the body. This restores the flow of blood and lymph.
Manual therapy
Along with massage, manual therapy also includes manual therapy for treating narrowing of the vertebral arteries. Using special movements, the specialist stretches the spine, releasing compressed vessels.
During the procedure, a crunching sound appears, which is considered normal. This is how vertebral subluxations are reduced and muscle blocks are eliminated. Manual therapy should be performed by an experienced specialist.
Physiotherapy
Gymnastics is an important part of the treatment of diseases of the musculoskeletal system and cardiovascular system. An individual set of exercises is compiled for the patient.
This makes gymnastics as effective as possible. Compressed vessels are released when performing head tilts, flexion and extension exercises.
Operation
The operation is prescribed when the diameter of the vertebral artery decreases by more than 70%. Interventions are aimed at dilating blood vessels, releasing compressed nerve endings, and eliminating pathological formations (bone growths, hernias, tumors). The following types of operations are used:
- carotid endarterectomy (the walls of the arteries are cleared of atherosclerotic plaques, restoring blood flow);
- angioplasty (vessel patency is improved by introducing a synthetic prosthesis);
- stenting (the narrowed section of the artery is strengthened with a wire frame).
Important information: How to strengthen weak walls of blood vessels (capillaries) in the brain with folk remedies and what to do to treat brittle (fragile) veins in the legs
Description of the ultrasound procedure
Duplex scanning technique is used to diagnose various vascular diseases. This ultrasound procedure allows you to check the speed and nature of blood flow in the veins, as well as visualize them and determine the causes of disorders. For example, this procedure makes it possible to diagnose thrombosis, narrowing of a vessel, thinning of its wall, dilation of veins, etc.
The procedure is absolutely painless and lasts about half an hour. During this time, the doctor moves a special sensor over the neck, back of the head, temples and closed eyes, which directs ultrasonic waves, and then captures and records their reflection from moving red blood cells.
The veins of the head and neck perform very important functions, so their condition is worth monitoring. If you have any alarming symptoms, you should consult a specialist and undergo an examination. Diseases diagnosed in the early stages of development are much easier to treat.
Source: FB.ru
Causes
The causes of vasoconstriction can be very different and can be congenital or acquired.
The first group includes:
- hypoplasia of cervical vessels;
- carotid artery stenosis;
- pathologies of development of the vertebrae of the neck;
- vertebral arthrosis of the vertebrae in the cervical region.
Purchased:
- high blood sugar;
- atherosclerosis;
- increased blood pressure;
- injury, hernia formation in the cervical spine;
- osteochondrosis;
- bone growths;
- neoplasms of the neck organs.
One of the most common congenital vascular anomalies in the cervical spine, which can narrow the vessels, is hypoplasia of the vertebral arteries.
The reasons for the development of this disorder, like other congenital diseases, have not been precisely determined.
However, there are several risk factors, the presence of which in a pregnant woman increases the risk of developmental pathologies in the child:
- chronic poisoning of the expectant mother's body (excessive consumption of alcohol, drugs, smoking, taking specific medications, negative industrial factors);
- injuries to a woman carrying a fetus;
- infections during pregnancy (rubella, influenza, toxoplasmosis);
- exposure to radiation.
Among the acquired disorders of the neck vessels, accompanied by their narrowing, stenosis of the carotid arteries is often diagnosed.
The risk category for these diseases includes citizens exposed to:
- Atherosclerosis. Deterioration of lipid metabolism with excess cholesterol provokes the formation of atherosclerotic plaques on arterial walls.
- High blood pressure. The vessels in the head can narrow due to a persistent increase in their tone, which, in tandem with atherosclerosis, causes a sharp decrease in their optimal diameter.
- High blood sugar. With the prolonged development of this disease, the elasticity of the vascular walls is impaired, with their deformation and the appearance of cholesterol plaques.
- Cervical injuries, osteochondrosis, hernias. With such spinal problems, mechanical compression of the carotid arteries is observed;
- Cervical neoplasms.
- Excess body weight.
In addition, risk factors for the development of carotid artery stenosis include a sedentary lifestyle, frequent stress, bad habits, excessive consumption of junk food (salted, fried, smoked, etc.).