Thrombosis is a dangerous disease that affects arterial and venous vessels. It is accompanied by a narrowing of the vascular cavity due to its blockage with a blood clot. Portal vein thrombosis is a dangerous disorder of the functioning of the liver and adjacent organs. Most often, blockage of this vessel is not an independent disease, but a complication of pathological processes occurring in the body. Even minor factors can provoke thrombosis. If left untreated, it can lead to internal bleeding and death.
Hepatic portal vein thrombosis
Portal vein thrombosis is a disease characterized by blocking of the vascular lumen by a thrombus, up to complete occlusion. In 5% of cases, the disease develops against the background of cirrhosis, in 30% - as a result of hepatocellular carcinoma.
Poor circulation is noted not only in the abdominal region, but throughout the body. As a result, the functioning of the digestive tract is disrupted, which is accompanied by a number of unpleasant symptoms.
According to ICD-10, portal vein thrombosis has code I81, according to which it is also called “portal vein thrombosis.”
Disease prevention
The progression of portal vein thrombosis can be avoided if you carefully follow the preventive recommendations and follow them accurately. This is especially true for those patients who are at risk. The most effective methods are:
- maintaining a normal level of physical activity, walking;
- proper nutrition;
- giving up bad habits, including excessive caffeine consumption;
- doing cardio exercises;
- using various methods to strengthen the cardiovascular system.
Read on to learn more about how acute pancreatitis complicated by portal vein thrombosis occurs.
Reasons for the development of the disease
The causes of hepatic portal vein thrombosis vary. In newborns, the disease occurs as a result of infection through the umbilical cord. In adulthood, the pathological process may develop after acute appendicitis.
The causes of the disease in adults are as follows:
- bacterial damage to the vein or the development of purulent pylephlebitis;
- the presence of cystic formations on the vein;
- cirrhosis;
- period of bearing a child;
- hereditary predisposition to vascular pathologies;
- increased blood clotting;
- chronic heart failure;
- malignant or benign tumors in the area of the affected vein and nearby organs;
- postoperative period.
Diagnostics
Laboratory research
- general blood test - decrease in hemoglobin, red blood cells and color index;
- coagulogram – increased prothrombin index, decreased blood clotting time.
Other laboratory tests (liver tests, blood biochemistry, lipid profile, general urine test, etc.) will reflect only the cause of the disease.
Instrumental studies
- Ultrasound or CT (computed tomography) of the abdominal cavity, which shows symptomatic signs of portal vein thrombosis (enlarged spleen, ascites, varicose veins in the area of portocaval anastomoses) and the blood clot itself. These research methods allow us to predict the location and size of the thrombus in the portal vein, as well as calculate the speed of blood flow;
- Angiography is a method that definitively confirms the diagnosis. A contrast agent is injected into the portal vein and the movement of this substance through the vessel is monitored using an X-ray unit, the data from which is displayed on the monitor. The method allows you to find out the exact location of the thrombus, its size, the speed of blood flow through the portal vein, through the portocaval anastomoses and through the hepatic veins.
Main symptoms
To make a timely diagnosis, you should familiarize yourself with the clinical picture of portal vein thrombosis. Symptoms vary at each stage of the disease. They depend on concomitant diseases and the location of the blood clot.
The most common signs of impaired blood flow include:
- the presence of free fluid in the abdominal cavity;
- presence of blood in the stool;
- pronounced pain in the peritoneum;
- flatulence;
- bleeding from the esophagus into the stomach;
- complete absence of stool;
- dark vomit.
In the presence of thrombosis, the patient may notice the disappearance of physiological hunger. At the same time, the urge to go to the toilet disappears, and constipation is observed.
The most significant symptom is extensive hemorrhage in the esophagus due to dilated veins.
If the disease occurs in an acute form, the stool becomes liquid. Pain sensations are concentrated in the epigastric region and periodically radiate to the right hypochondrium.
Symptoms
Against the background of the symptoms of the underlying disease, signs of damage to the portal vein appear:
- vomiting, and the vomit is dark in color and looks like coffee grounds;
- increasing pain in the abdomen - first on the right side, then in the left hypochondrium;
- intestinal paresis;
- diarrhea;
- the appearance of free fluid in the peritoneum;
- enlarged spleen;
- bleeding from dilated veins of the esophagus and stomach;
- anal bleeding;
- liver abscess;
- drop in blood pressure;
- veins appear on the skin of the abdomen and become clearly visible;
- liver encephalopathy;
- tarry stool;
- peritonitis.
The pathology develops suddenly, without previous signs.
Characterized by chills, fever, and increased temperature. With chronic thrombosis, symptoms are often absent or mild:
- constant aching pain;
- low-grade body temperature for a long time;
- chills;
- general weakness.
Classification and forms
The symptoms and manifestations of the disease largely depend on its type. According to the severity of the pathological process, severe, moderate and mild forms of thrombophlebitis are distinguished.
They differ in the following characteristics:
- In mild cases of the disease, the thrombus covers only half of the vein cavity. It is located in the area of the transition of the portal vein to the splenic vein.
- The average form of the disease is characterized by a thrombus affecting the area of the mesenteric vessel.
- In severe cases, thrombosis affects all veins located in the abdominal cavity. Blood flow slows down significantly, which affects the functioning of the digestive organs.
There are also chronic and acute forms of the disease. In the first case, the course of the disease is long, accompanied by other pathological processes. In acute thrombosis, a rapid increase in the intensity of symptoms is observed. In this case, there is a risk of death.
After successful removal of a blood clot, the patient must undergo regular preventive examinations with a phlebologist.
Features of the pathology
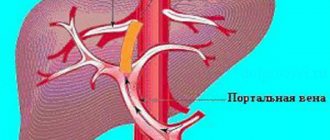
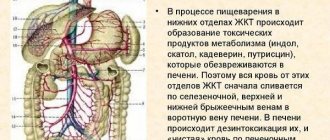
With the help of the portal vein, blood flows to the liver from other abdominal organs. It is a blood vessel only 5–7 cm long and up to 2 cm in diameter. The portal vein has many branched vessels in the liver and is responsible for detoxifying the blood, as well as for the functioning of the digestive system as a whole. None of the pathologies of this vessel goes away without a trace and causes serious consequences. Thrombosis manifests itself in the presence of blood clots that prevent its movement towards the liver, while the pressure in the vessels increases and their cavity expands. A blockage of the vessel can form anywhere in the liver along the entire length of the portal vein. There are different types of blood clots:
- Truncular. Formed in the venous trunk.
- Koreshkovy. Initially it occurs in the vessels of the stomach or spleen, and over time it spreads to the portal vein.
- Terminal. Its development occurs inside the liver.
There are four stages of thrombosis development:
Liver thrombosis
- First. No more than half of the venous cavity is blocked, there are practically no symptoms.
- Second. The first signs of the disease appear, 60% of the lumen is thrombosed, the blood flow is slightly impaired.
- Third. Many veins of the abdominal cavity are affected, blood flow is significantly slowed down.
- Fourth. Separation or destruction of a blood clot.
The blood flow in the veins is not as strong as in the arteries, so blood clots do not break off as often in this case. However, if this happens, the clot may break into several parts and cause simultaneous blockage of several vessels. If left untreated, the disease can cause a number of serious complications. Among them: liver abscess, bleeding, liver coma, esophageal varices, peritonitis, intestinal infarction. All these pathologies can lead to death if surgery or drug therapy is not started immediately.
We recommend reading:
Liver enlargement
Diagnostic measures
A thrombus in the portal vein of the liver is diagnosed using standard methods. The first priority is to examine and interview the patient.
After collecting an anamnesis, the following procedures are prescribed:
- Doppler ultrasound, which is an addition to ultrasound, helps to identify disturbances in blood flow in the abdominal cavity.
- Liver tests are necessary to assess the condition of the liver and diagnose primary diseases of the organ.
- Donating blood for coagulation tests gives an idea of the likelihood of a blood clot forming.
- Contrast venography helps to identify the exact location of the formed blood clot.
Forecast
The most severe stages of portal vein blockage have the most unfavorable prognosis, so under no circumstances should you delay treatment. The outcome of such events is almost always fatal.
The following video contains even more useful information on the issue of thrombosis:
Portal vein thrombosis is a condition that is accompanied by the formation of blood clots in the portal vein system, which can cause blockage of the lumen of this vessel. As you know, the portal vein is one of the most important vascular structures that ensure normal blood flow from the digestive tract. That is why its thrombosis is a serious pathological process that can cause acute disruption of the functioning of the organ elements of the abdominal cavity. The disease is diagnosed mainly in elderly patients who have a tendency to increased blood clotting and intravascular thrombus formation.
The pathological process and its first manifestations require an immediate response from the person and seeking medical help. Otherwise, the progression of this condition may be complicated by complete occlusion of the portal vein and death.
Treatment of portal vein thrombosis
It is highly recommended not to ignore the symptoms of portal vein thrombosis. Treatment is selected individually, taking into account the severity of the disease. The use of drug therapy is advisable for chronic thrombosis.
If bleeding develops, the patient is admitted to the hospital. A probe is inserted into the abdominal cavity to stop the bleeding. Medicines are also taken to stop bleeding.
The goals of conservative therapy are as follows:
- reduction of signs of portal hypertension;
- preventing excessive blood clotting;
- blood thinning.
Treatment
With timely diagnosis of an acute condition, conservative treatment is possible. It consists of using drugs aimed at relieving spasm of blood vessels and expanding their lumen. They use medications that thin the blood and prevent the formation of blood clots. To relieve pain, the administration of analgesics is indicated.
The translumbar aortography method, which is used in specialized vascular centers, makes it possible to establish not only the localization of the clot, but also its age. A fresh clot can be dissolved using a lytic mixture that is injected through a catheter.
Surgical treatment consists of thrombectomy. In severe cases, resection of part of the aorta is performed with further plastic surgery of the vessel. In case of infarction of the spleen or kidney, their removal is indicated.
Medication method
Drug therapy for vascular thrombosis requires an integrated approach. The dosage of drugs is selected by the attending physician on an individual basis. The average duration of medication use is 1 month. After completing the treatment course, tests are taken again.
The following groups of drugs are used:
- indirect anticoagulants (Neodicoumarin and Sinkumar);
- thrombolytic drugs (Streptokinase and Fibrinolysin);
- antimicrobial drugs (Tienam, Meronem);
- direct anticoagulants (Fraxiparin, Heparin).
Saline solution or Reopoliglucin is administered intravenously in a dosage of 400 or 200 ml. Direct anticoagulants are used urgently in the first hour after the onset of symptoms of the disease.
They are administered intravenously at a concentration of 40,000 units over 4 hours. Thrombolytic drugs are administered using a dropper at a dosage of 20,000 units.
Operation
Depending on the nature of the disease, a treatment method is selected. Surgical treatment is carried out if medications are insufficiently effective in the first 3 days of hospital stay.
The following types of intervention are used:
- Sclerosing injection therapy. The procedure involves injecting a gluing solution into the vein to narrow the enlarged areas. The operation is performed in conjunction with esophagoscopy.
- Splenorenal anastomosis. This type of intervention is practiced if the patency of the splenic vein remains.
- Application of mesenteric-caval anastomosis. It is carried out if it is necessary to eliminate portal hypertension.
- Prosthetics are performed if the splenic vein is blocked. The prosthesis is placed in the area between the superior mesenteric and inferior vena cava.
In case of prolonged bleeding, they resort to surgery using the Tanner method. The stomach area is crossed in the cardiac section. After this, its walls are stitched together. If pylephlebitis develops, its complications are prevented by installing drainage.
The type of operation depends on the nature of the pathology and the doctor’s decision.
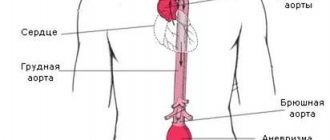
Clinical picture
When a blood clot is located directly in a vein, protrusion of blood vessels in the abdomen and chest is observed.
Swelling of the limbs and pain in the lower body also occur. Such a clinical picture develops very rarely, since a blood clot usually penetrates into the vessels of the abdominal cavity from other parts of the circulatory system. Classification of IVC segments that are susceptible to acute thrombosis:
- infrarenal;
- hepatic;
- renal;
- suprarenal.
A floating thrombus of the inferior vena cava is characterized by mild symptoms. In this case, the blood clot is localized near the wall of the vessel.
Symptoms of a thrombus in the infernal segment of the IVC are intense lower back pain, cyanosis of the skin, swelling of the extremities. Veins are clearly visible in the lower abdomen.
With thrombosis of blood vessels in the renal and suprarenal segment, symptoms arise that are characteristic of a kidney tumor. No blood flow disturbances are observed. Signs:
- severe pain in the lumbar region;
- hematuria;
- decrease in urine volume or its complete disappearance;
- development of intoxication;
- nausea and vomiting.
When blood flow is restored, the symptoms disappear completely or significantly reduce their manifestation.
Due to a thrombus in the liver segment, a large volume of blood accumulates in the organ, which leads to stretching of its fibrous membrane. This provokes the following symptoms:
- bursting pain in the right side that radiates to the scapula;
- ascites;
- development of jaundice;
- increase in the size of the spleen;
- cyanosis of the anterior abdominal wall.
On palpation, the smoothness of the liver and a change in its contour are felt. Additionally, doctors observe dilation of the veins in the upper abdomen.
The main symptom of mesenteric thrombosis is intense pain in the right side of the abdomen. Nausea develops, turning into vomiting, and loose stools. With intestinal necrosis due to circulatory disorders, a significant increase in body temperature occurs. Additionally, a complete absence of peristalsis and fecal retention are observed.
Complications and prognosis
Thromboembolism in liver cirrhosis and other diseases of internal organs leads to various complications. If treatment is not started on time, the risk of coma, the development of purulent peritonitis, intestinal infarction, hepatorenal syndrome and extensive bleeding increases.
The prognosis in these cases is unfavorable. If the mesenteric vein is completely blocked, the likelihood of death increases.
Timely therapy can prevent the clot from moving through the portal vein. Following all the doctors’ recommendations, the patient is fully back on his feet in 3-5 weeks. Small blood clots respond well to drug therapy. The earlier treatment is started, the more favorable the outcome will be.
Cardio exercises, yoga and physical therapy have a positive effect on the functioning of the vascular system.
Complications
In the absence of therapeutic measures, purulent peritonitis or another infection develops, which leads to attacks of intoxication. With a complex picture of the course of the disease, a violation of the temperature regime occurs, the liver changes pathologically, which can be felt even with palpation - it becomes lumpy, dense, enlarged, and pressure is painful.
Prolonged delay of treatment is fraught with massive bleeding, intestinal infarction, the development of various types of abscesses, or the occurrence of purulent peritonitis. All these pathologies greatly worsen the prognosis of the disease.
Read on to learn about the prognosis for portal vein thrombosis.