0
Author of the article: Marina Dmitrievna
2017.05.31
273
Heart attack
Pulmonary edema during myocardial infarction is one of the acute complications that often leads to death. This process is life-threatening, as breathing problems arise. Pulmonary edema during myocardial infarction greatly reduces the chances of a full recovery, especially if help is provided to the patient late.
A heart attack requires emergency care, regardless of its complications
Why do the lungs swell during myocardial infarction?
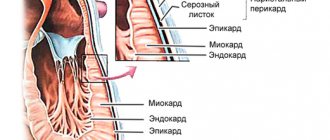
Swelling of the pulmonary system is a complication of myocardial infarction and a concomitant disease of heart failure. In this case, necrosis of cardiomyocytes and necrosis of cardiac muscle cells occurs. The main reason is a mismatch with the heart's oxygen needs. At the same time, the coronary vessels are not able to fully fill the myocardium with the necessary volume of blood for normal metabolism.
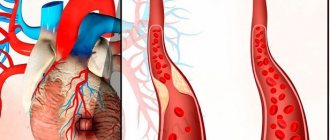
Swelling of the lungs is a consequence of blockage of the coronary arteries of the heart muscle, against which the plasma part of the blood accumulates in the alveoli, after which the lumen in the arteries of the lungs is blocked, as a blood clot and embolism are formed. This also leads to a lack of oxygen (hypoxia) and death of lung tissue, which causes respiratory failure.
There are other causes of respiratory dysfunction - mitral valve insufficiency on the left, which leads to high blood pressure. If heart failure develops rapidly, especially in a decompensated form, then congestion occurs, which causes excessive fluid to accumulate in the lungs. This contributes to an increase in pressure in the capillaries of the respiratory system, releasing plasma through the walls of blood vessels.
How does pulmonary edema occur?
During a heart attack, blockage of the coronary vessels occurs and, as a result, normal blood circulation is disrupted. The alveoli are filled with blood leaking from the vessels, and breathing deterioration quickly develops.
The worst-case scenario is the formation of blood clots, and as a result, the development of embolism. The patient has virtually no chance of survival. Parts of the lungs die, after which respiratory failure rapidly develops, ending in hypoxia and death of the patient.
Pulmonary edema can also develop as a result of acute decompensated heart failure. The work of a healthy heart occurs through rhythmic alternating contractions of the myocardium and ventricles. As a result of a heart attack, high blood pressure or coronary artery disease, the ventricles lose their mobility, stop completely relaxing, and then, when contracting, push out blood. This occurs during a heart attack due to the death of some muscle fibers.
The mechanism of development of pulmonary edema during myocardial infarction
When a significant portion of the heart muscle dies, the heart stops pumping, causing the blood supply to stop. Consequently, cells and tissues do not receive oxygen and nutrients. The myocardium tries to cope with the problem on its own, so it contracts intensively. But so little blood fluid comes in that there is only enough for the ventricles, and the aorta remains unfilled.
Against this background, the pressure in the vessels of the lungs, atrium and ventricle on the left increases retrogradely, so the pulmonary system is overloaded. In response to increased pressure, blood vessels spasm, causing them to sharply narrow, which leads to heart failure, in which liquid blood elements penetrate the interstitium (connective tissue) and alveoli. Further develops cardiac asthma and alveolar edema.
Causes of leg swelling after a heart attack
After an MI, swelling in the legs may appear for the following reasons:
- increased fluid volume in the vascular system;
- decreased cardiac output;
- violation of venous outflow;
- increasing vascular resistance.
Whatever edema develops, an imbalance between the filtration of fluid from the vessels into the tissue and its reabsorption by the venous vessels is the main reason why the legs swell after a heart attack, and the treatment of this disease should take this mechanism into account.
After an MI, the human body changes seriously, and not only due to a decrease in the pumping function of the heart, but also because the hormonal levels change, affecting the functioning of the kidneys, which also begin to work worse. As a result, a weakened heart is forced to pump an increased volume of blood, which is why swelling of the legs occurs after a myocardial infarction.
Associated symptoms
Myocardial infarction is accompanied by excruciating pain and other symptoms, but with pulmonary edema, specific symptoms arise that can be used to differentiate swelling from other complications:
- very rapid increase in symptoms;
- sudden feeling of lack of air and suffocation;
- increased shallow breathing;
- difficulty breathing;
- fear of death;
- anxiety;
- attempts to inhale air with a wide open mouth.
When blood enters the alveoli, the following symptoms occur:
- the patient coughs heavily;
- when coughing, pink, foamy sputum comes out;
- breathing bubbles and wheezes;
- heart rate increases to 180-200 beats per minute;
- veins swell;
- a person experiences severe suffocation, especially in a horizontal position;
- cold sweat appears;
- the skin turns blue.
At the beginning of the development of pulmonary edema, the cough is characterized by dryness, but as it rapidly progresses, it becomes wet. In this case, foamy sputum mixed with blood is necessarily released.
First aid
If a myocardial infarction occurs at home, you must immediately call an ambulance. But it is also important to act independently, since the outcome of the attack depends on this.
What to do before the doctors arrive:
- put the victim to bed, placing a high pillow under his head, but it is better to give him a semi-sitting position;
- put a Nitroglycerin tablet under your tongue (then give it every 15-20 minutes);
- to thin the blood, give Aspirin (if the patient is not able to chew acetylsalicylic acid on his own, he must first crush the tablet into powder);
- measure blood pressure periodically.
First aid and treatment
Before emergency medical services arrive, a number of manipulations should be performed that can save a person’s life during a heart attack with pulmonary edema:
- It is necessary to change the body position: it is impossible to lay the patient on a horizontal surface; it is recommended to help him take a semi-sitting position.
- You need to put Nitroglycerin tablets (1-2 pcs.) under your tongue. This should be done every 10-15 minutes until the ambulance arrives.
- In order to reduce the risk of blood clots, the patient should take acetylsalicylic acid in a dosage of at least 150 mg, the upper recommended limit for the amount of this drug is 160 mg. Moreover, the drug should be chewed, which will speed up the onset of positive changes.
Qualified medical care begins with intravenous administration of Nitroglycerin (a dropper is given). Sufficient solution concentration is 1%. The rate of introduction of the substance into the body is 20 mcg per minute. To eliminate shock, pain and reduce heart rate, a combination of Dihydrobenzperidol + Fentanyl or their analogues is used.
Humidified oxygen can normalize the patient's condition with pulmonary edema. It is delivered into the body in different ways: by intubation, using a mask or nasal cannula. To reduce the intensity of foaming caused by filling the alveoli with transudate, use Antifomsilan or supply oxygen through gauze moistened with alcohol. To normalize blood pressure, excess fluid must be removed from the body. Diuretics are recommended. They allow you to reduce the volume of circulating fluid.
Important information: What are the blood pressure and pulse readings during a heart attack?
Drugs that stimulate contraction of the heart muscle and normalize blood circulation help prevent shock. Other medicines that may be used:
- anticoagulants with antiaggregation properties;
- ganglion blockers;
- drugs that prevent the development of arrhythmia;
- beta blockers;
- glucocorticosteroids;
- angiotensin-converting enzyme inhibitors.
Diagnostics
Emergency doctors can make a preliminary diagnosis; a clinical picture is enough for this. To accurately determine the nature of the pathological condition, a stethoscope is used (heart rhythm is assessed), and an ECG is performed. In a hospital setting, hardware diagnostic methods are used:
- Ultrasound of the heart, lungs;
- fluoroscopy (used to assess the condition of the lungs).
In case of myocardial infarction, a biochemical blood test is performed. Thanks to this, it becomes possible to assess the degree of cell damage by necrosis. The quantitative components of a number of indicators are determined: leukocytes, platelets, ESR, specific proteins, etc.
Surgery
In this case, medical care is provided by forcibly dilating a vessel that has undergone stenosis. The method of balloon coronary angioplasty is used. Subsequently, the balloon is removed, but this increases the risk of repeated narrowing of the vessel lumen. To prevent this from happening, a stent is installed. This type of prosthesis is located inside the affected vessel. As a result, the risk of narrowing of the lumen is eliminated.
Traditional methods
It is advisable to use such a therapeutic measure only at the stage of recovery after myocardial infarction. Taking home remedies is allowed only on the advice of a doctor. During the recovery period, decoctions of nettle, motherwort, marsh cudweed, sweet clover, hawthorn fruit, and elecampane root can be taken. Carrot juice and a mixture of honey and nuts provide a positive effect. In this case, basic drug therapy must be carried out.
Important information: Can there be a temperature during myocardial infarction?
Preventive measures
You should exercise regularly. It is important to control your weight. If you gain weight, a balanced diet is recommended. You will have to give up smoking and alcohol. It is necessary to regularly examine the patient. Timely detected pathologies of the heart, lungs or kidneys will help prevent disruption of the myocardium.
Diagnostic methods
To make an accurate diagnosis, urgent diagnostic measures are carried out, which include the following:
- Visual and palpation examination of the patient, taking anamnesis, measuring blood pressure, listening to pulse rate and heart rhythm.
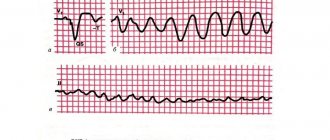
- Electrocardiogram.
- Ultrasound examination of the lungs and heart.
- X-ray of the lungs.
- Blood collection for biochemical and general analysis to determine the level of enzymes and proteins.
- Analysis of urine.
Differential diagnosis is required. Pulmonary edema is compared with embolism, internal bleeding, pneumothorax, aortic dissection, pericarditis, pancreatitis, and perforation of gastrointestinal ulcers.
Diagnostics
Diagnosis of the clinical syndrome accompanied by edema of the pulmonary tissue against the background of myocardial infarction should be comprehensive.
A preliminary diagnosis is made based on the results of a general examination, survey, analysis of complaints, and collection of the patient’s medical history. The final diagnosis is made after laboratory and instrumental examinations.
Myocardial infarction is established after studying the data obtained after interviewing, examining the patient and conducting a series of diagnostics:
- ECG. Taking an electrocardiogram for symptoms of MI is a mandatory procedure. Signs of a heart attack appear on ECG film and indicate the localization, stage and intensity of the process.
- A blood test for specific enzymes (lactate dehydrogenase, creatine phosphokinase), troponins I, T. The results of these laboratory tests will accurately indicate the presence of a heart attack.
- Echocardiography may be performed.
Common clinical manifestations of respiratory failure, such as:
- dyspnea,
- suffocation,
- tachycardia,
- varying degrees of wheezing on auscultation,
- acrocyanosis,
- forced situation
- weakness,
- cold sweat,
will arouse suspicion among the attending physician.
To clarify the diagnosis, additional research methods will be required:
- X-ray of the chest organs. The x-ray shows an increase in the size of the lungs, transudate is determined, and swelling of the hilar and basal zones is clearly visualized.
- It is possible to conduct laboratory tests, for example, sputum analysis, to clarify the etiology of pulmonary tissue edema and exclude bacterial origin, but they are not decisive in making a diagnosis.
Diagnostic measures for MI, especially complicated by the clinical syndrome of swelling of the lung tissue, should be carried out quickly.
Attention. In case of obvious and characteristic clinical symptoms, it is possible to carry out treatment procedures without a detailed and thorough examination, because such a pathological condition is extremely life-threatening.
Treatment of pulmonary edema during myocardial infarction
After the ambulance arrives, doctors administer the following medications:
- Nitroglycerin intravenously helps dilate blood vessels, reducing the return of venous blood fluid.
- To relieve pain, Inapsin or Droperidol is administered. These drugs have antishock, antiarrhythmic and adrenolytic properties. To speed up the pain relief process, the injection solution is diluted with Fentanyl. It is strictly forbidden to use Morphine and Promedol, as the drugs depress respiratory abilities.
- To relieve pulmonary edema, it is advisable to administer humidified oxygen through intubation, a cannula or a mask. Most often, in such cases, foam forms, so to avoid an adverse reaction, oxygen is administered through a gauze mask, which is moistened in an alcohol-containing solution or the drug Antifomsilan. This is necessary to prevent infection.
- To remove excess fluid from the body and lower blood pressure, the patient is given one of the medications: Uregit, Lasix, Piretanide, Bumetanide.
- If cardiogenic shock is suspected, Dopamine or Dobutamine is administered.
- To normalize heart rhythm and maintain cardiac conduction, the patient should take Amrinon, Metoprolol, Isoproterenol, Enalapril.
Upon arrival at the intensive care unit, the patient is prescribed the following groups of drugs:
- Anticoagulant agents reduce blood clotting, dilute biological fluid, and restore blood flow.
- Beta blockers reduce blood pressure.
- Ganglion blockers reduce the load on the heart.
- Antiarrhythmic drugs.
- ACE inhibitors accelerate blood supply to the myocardium.
- Glucocorticosteroids normalize cell membranes and lysosomes.
- Antiplatelet medications prevent the formation of blood clots.
If there is no positive dynamics after the administration of these drugs, specialists perform defibrillation. That is, they influence the myocardium using electrical impulses.
Surgery
If the risk of death is high, surgical intervention is prescribed. It involves opening a blood vessel in which a blockage (thrombus) has formed with the obligatory installation of a balloon pulsator (coronary). During the operation the following manipulations :
- The surgeon makes a puncture in the femoral artery through which a special catheter with a polyurethane balloon is inserted. It contains helium, which is pumped in. When bloated, the pressure in the aorta increases, which speeds up blood circulation. This leads to reduced stress on the myocardium and improved heart function.
- The balloon is then deflated, reducing resistance and pressure to blood flow. Thanks to this, the heart does not need an increased supply of oxygen.
- A stent or shunt is installed in the damaged vessel, depending on the situation. Stenting is used to prevent the artery from narrowing further. Bypass surgery is needed when the vessel is too damaged. A stent is a mesh-type prosthetic pad that is installed inside a vessel. A shunt is a kind of implant that is removed from the saphenous veins of the lower limb. This segment is implanted into the damaged area.
- In case of complete occlusion, coronary bypass surgery is used, which involves removing the blocked part and installing an artery from the left side of the chest.
surgical intervention method
- clinical course of the attack;
- examination results;
- degree of neglect;
- the presence of concomitant pathologies and complications;
- general condition of the patient.
There are a number of contraindications to the operation:
- atherosclerosis;
- diabetes;
- cancerous tumors;
- inability to reduce high blood pressure;
- inflammatory processes.
Folk remedies
Traditional therapy methods are not used for inpatient treatment, but they are recommended for use during the rehabilitation period and in the future. Each recipe is based on natural ingredients that have a comprehensive effect on the body.
What you can do:
- Eat more nuts mixed with honey, which will significantly strengthen the immune system and the myocardium, as well as the walls of blood vessels.
- Brew rosehip and hawthorn in the standard way.
- Drink motherwort tincture from the pharmacy.
- Prepare fresh juices from carrots, pomegranates, beets, and pumpkins at home.
- Edema of cardiac origin can be eliminated using this decoction: take 2 tbsp. l. horsetail, pour a glass of boiling water (in a thermos) and let it brew for 40-60 minutes. Take the received dose per day. The duration of therapy is 21 days.
- Pour 4 tsp of boiling water over a glass. seed part of parsley, boil for 5-7 minutes, let cool. Drink 1 tbsp up to 6 times a day. l.
- Use corn silk. For 200 ml of water you need to take 30 grams of herb. Infuse in a thermos or under a warm blanket for 2-3 hours. Consume 1 tbsp half an hour before meals. l. three times a day.
- There is an excellent herb for swelling - hernia. For a glass of boiling water you need to take 1 tbsp. l., let it brew in a warm place for a couple of hours, then drink throughout the day half an hour before meals.
- Use fresh viburnum. Mash the berries. Add honey to taste. The resulting mass can be eaten 1 tbsp. l. 4-5 times a day or pour boiling water and drink as a tea drink.
You can use traditional medicine recipes only after consultation with treating specialists (cardiologist, pulmonologist). It is strictly undesirable to self-medicate.
Other techniques
After the patient has completed the main course of treatment, he is sent to the rehabilitation department, where the following activities are carried out:
- Bed rest for 3 days.
- If there are no complications, the patient should get out of bed twice a day, taking a sitting position. Initially, you are allowed to sit for 15 minutes, after which the time gradually increases to an hour.
- The process of defecation and urination is carried out in a vessel, the patient is fed by health workers or relatives.
- After about 5 days (if there are no serious complications), the patient is raised to his feet and walked along the corridor to develop motor abilities. The distance is determined by the attending doctor.
- The patient is discharged after 10-12 days, after which he is recommended to visit a sanatorium for rehabilitation.
- During recovery, specialists work with the patient - they carry out physiotherapeutic procedures and massages. The program necessarily includes a complex of physical therapy.
Particular attention is paid to diet, so you will have to adhere to the following rules:
- The diet is low-calorie, selected on an individual level by a nutritionist.
- In the first week, food should be pureed and have the structure of a puree soup.
- The daily norm is divided into 6 doses, the portions are small.
- Avoid consumption of salt, foods that are rich in cholesterol, animal fats, fiber, and nitrogenous substances.
- Dishes are prepared exclusively with water or steam.
- Fried, smoked, pickled, canned, fatty, fast food is prohibited.
Allowed food:
- instead of bread - crackers;
- porridge from oatmeal, semolina, rice, buckwheat;
- meat – veal, chicken;
- low-fat fish;
- eggs in the form of an omelet, steamed;
- low-fat cheeses, cottage cheese, fermented milk products;
- butter (small portions);
- juices, fruit drinks, compotes, pure still water, herbal decoctions;
- fruits vegetables;
- honey;
- light soups.
Forbidden food:
- sausage, ham, balyk and the like;
- canned food;
- rich pastries, fresh bread;
- meat, mushroom, fish broths;
- caviar and seafood;
- tomato juice, grapes, sorrel;
- pasta;
- chocolate and other sweets;
- coffee, strong tea;
- hot spices;
- mushrooms.
Forecast
With pulmonary edema that accompanies myocardial infarction, the prognosis is considered unfavorable. In approximately 30 cases out of 100, death is noted. The following factors lead to this:
- ruptures inside the heart;
- excessively high blood pressure;
- failure to seek medical help in a timely manner;
- the occurrence of complications.
There is a risk group - elderly people. This is due to the fact that the body is no longer able to recover quickly, and many functional capabilities are limited.
What could be the consequences?
Myocardial infarction carries many dangerous complications, but when it is accompanied by pulmonary edema, the risks increase even more. The most dangerous consequence is the death of the patient, but besides this, the following complications may arise:
- ventricular fibrillation of the heart organ;
- cardiogenic shock (sharp decrease in blood pressure);
- asphyxia;
- arrhythmia;
- heart failure;
- post-infarction cardiosclerosis;
- acute fibrous pericarditis (fluid accumulation in the pericardium);
- aneurysm (the affected area of the walls of the left ventricle protrudes);
- thromboembolism of the pulmonary arteries (vascular obstruction, tissue death);
- stopping the conduction of electrical impulses inside the heart;
- ischemic stroke.
Prevention of pulmonary edema during myocardial infarction
Preventive measures are necessary for people with diseases of the cardiovascular system, representatives who are at risk, as well as in the post-infarction period. Be sure to adhere to the following recommendations:
- Lead a physically active life, because this helps strengthen the heart muscle, ensure adequate oxygen supply to the body, and improve the condition of the immune system and blood vessel walls. Loads should be moderate and correspond to the age category and physical abilities of a particular person. The most useful exercises are cardio training. Be sure to take a walk in the fresh air every day, and swimming is beneficial. Sports with intense tempo are excluded.
- Get rid of extra pounds, which put additional stress on the myocardium.
- Change your diet - consume more fresh fruits, berries, and vegetables. Avoid fatty, smoked, fried and over-salted foods. Remember that a heart attack develops against the background of atherosclerosis, which occurs due to cholesterol deposits.
- Avoid stressful situations, try to perceive any problems calmly.
- Stop smoking, because a huge amount of tar and nicotine is deposited on the walls of blood vessels.
- Do not abuse alcoholic beverages, as they contribute to the development of hypertension. The exception is red wine, which can be consumed in very small quantities.
- Treat any pathological disorders in the body in a timely manner.
- Once a year, visit a therapist or cardiologist for a preventive examination (after a heart attack with pulmonary edema - once every six months).
During myocardial infarction, swelling of the lungs greatly complicates the course of the attack. Therefore, it is important to call doctors when primary signs appear and provide the patient with all possible pre-medical care. But it’s even better to adhere to preventive measures that prevent the occurrence of a heart attack and other diseases of the cardiovascular system.
What is a massive heart attack?
Myocardial infarction is understood as a deterioration in the functioning of the heart after the death of its muscle layer due to partial or complete cessation of blood supply. Based on the affected area, doctors distinguish two forms of the condition - small- and large-focal, as well as extensive infarction.
The last type is the most dangerous, since all layers of the heart muscle are affected. The prognosis for this diagnosis is the most pessimistic - the vast majority of patients die. With timely assistance and intensive treatment, the chance of recovery is also small. Complete rehabilitation is impossible - the heart after a massive heart attack remains vulnerable to the slightest stress.
The development of an acute condition usually occurs in people with cardiovascular diseases (atherosclerosis, hypertension, coronary disease, etc.). Diabetes mellitus, smoking, obesity, renal failure can also provoke a large heart attack - the cause can be any load on the heart, leading to circulatory disorders.
You can understand that myocardial infarction is developing by:
- Chest pain, burning or stinging sensation
- Increased heart rate, interspersed with slowness
- Dyspnea (shortness of breath), asthma attacks
- Development of panic mood, fear of death
- Abdominal pain (with damage to the posterior wall of the heart).
This condition requires immediate medical attention and treatment.