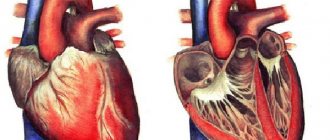
Dextrocardia is a congenital anomaly of the cardiovascular system, a type of dystopia in which the heart is partially or completely displaced to the right and occupies a position mirror symmetrical to the normal one.
The parts of the heart and all large vessels are located in a similar way. In some cases, a mirror arrangement of some or all internal organs is revealed. According to statistics, dextrocardia occurs in approximately 0.01% of the population.
If the abnormal location is not accompanied by other pathologies, dextrocardia may not manifest itself and is discovered by chance, when visiting a doctor for other reasons.
A shift of the heart to the right can also be a consequence of pathological processes in the chest: pulmonary atelectasis, hydrothorax, tumor processes. With secondary mechanical displacement they speak of pathological dextraposition of the heart.
Causes
The formation of organs and body systems occurs in the first trimester of pregnancy . The heart tube forms in the first weeks of embryonic development and, for unknown reasons, bends to the right.
The most likely cause of the abnormal structure of the cardiovascular system is considered to be mutations in the genes ZIC3Shh, HAND, Pitxz, ACVR2 . There is evidence of an autosomal recessive type of inheritance of the anomaly.
Risk factors for developing the anomaly have not been clarified.
The essence and history of the method
A phonendoscope in the hands of a doctor is so familiar that it does not evoke any emotions. However, by historical standards, it appeared recently - back in the 19th century, doctors listened to the patient’s heart and lungs directly with the ear, applying it to the patient’s body. Rene Laennec was the first to improve a procedure that was not entirely pleasant for a doctor; in order to exclude direct contact with the patient’s body, he listened to the heart using a sheet of music rolled up into a tube. And I was very sincerely surprised when I heard the heart sounds better and more clearly. Later, the doctor invented a primitive stethoscope, and even later, the Russian scientist P. N. Korotkov invented a phonendoscope, which doctors still use today.
The heart is a constantly working organ. When it contracts, peculiar sounds are formed that are well transmitted through tissue structures. It is these sounds that the doctor listens to using a phonendoscope.
The heart auscultation algorithm is quite simple, but only a doctor with practical experience can evaluate it correctly. The method has no contraindications; it can be used to examine patients of any age group.
Auscultation of the heart also has listening points - certain areas on the chest where various parts of the myocardium are projected in detail. Through auscultation you can:
- Assess heart rhythm.
- Analyze the contractile force of the myocardium.
- Assess the timbre coloring of sounds that are heard when using a phonendoscope.
- Identify extraneous noise.
Using a phonendoscope, the doctor can preliminarily determine the presence of the following pathologies:
- ischemia (CHD);
- heart muscle defects;
- ventricular hypertrophy;
- ari src=”https://davlenienorm.com/wp-content/uploads/2018/11/auskultatsiya-serdtsa-2.jpg” class=”aligncenter” width=”545″ height=”343″[/img] Arrhythmia on ECG
- inflammatory processes in the myocardium.
The results of auscultation determine further tactics for patient management. Having suspected a pathology, the doctor will refer the patient for additional examinations, after which he will be able to accurately establish the diagnosis.
Danger and complications
Abnormal location of the heart in the absence of concomitant pathologies does not pose a particular health hazard and does not affect the quality and duration of life. In such cases, patients often learn about their characteristics by chance, during a medical examination for another reason.
One of the most significant risks for a patient with undiagnosed and uncomplicated dextrocardia and organ transposition is medical error in making a diagnosis. Diagnosis of the most common diseases of internal organs is difficult due to their unusual location and the rarity of such clinical cases.
Difficulties arise when it is necessary to perform abdominal operations, especially when it comes to the need for transplantation of asymmetric organs.
As practice shows, people with a dystopic heart location are more prone to diseases of the respiratory system and other infectious diseases.
In most cases, the dystopic location is accompanied by other developmental defects , including:
- Transposition of the great arteries;
- Pulmonary artery stenosis in children;
- Endocardial defects;
- Double ventricular outlet;
- Ventricular septal defect;
- Tetralogy of Fallot.
An abnormal location of the heart can be combined with severe pathologies of organ development , for example, patients have a two- or three-chambered heart.
The danger of the patient’s condition depends on the type of concomitant pathology and its severity. Some concomitant heart defects appear immediately , in the first hours of life (the so-called “blue” defects), some (“white”) can be detected later, due to their asymptomatic course at an early age.
Sometimes a right-sided heart is combined with other pathologies of the abdominal and pleural cavities. One of the most common concomitant pathologies is heterotaxy syndrome . Patients with heterotaxy syndrome often have no spleen; in some cases, several underdeveloped spleens with significant dysfunction are found.
In 25% of cases, patients with dextrocardia are diagnosed with primary ciliary dyskinesia (PCD), a rare pathology of the development of the ciliary epithelium. Normally functioning cilia influence the processes of formation of internal organs and often cause their transposition.
Half of patients with PCD are diagnosed with Kartagener-Sievert syndrome , which is inextricably linked with the abnormal position of internal organs. In such patients, pathological disorders of the anatomical structure of the upper respiratory tract and numerous bronchiectasis are detected.
Cilia on the surface of the mucous membranes, which act as an active filter, may be completely absent.
Men with this disease are infertile because their sperm lack flagella.
This pathology is always combined with complete or partial transposition of internal organs, which indirectly confirms the hypothesis about the hereditary nature of dextrocardia.
Dystopic location of the heart is often found in children with Patau syndrome - trisomy of the 13th pair of chromosomes. This chromosomal disease is accompanied by multiple malformations affecting almost all organ systems; patients with Patau syndrome rarely survive to school age.
Reasons for the abnormal situation
When studying a set of genes in patients with right-sided localization of the heart, mutations were found in some regions of chromosomes that arise in the first trimester of pregnancy. They can be inherited or appear primarily under the influence of damaging factors. The heart tube, from which the heart is subsequently formed, deviates to the right side in the fetus, which leads to the formation of a mirror arrangement of the organ.
Most often, other structures of the thoracic and abdominal cavity also occupy the reverse position at the same time. Depending on the combination of developmental anomalies, the following options are formed:
- reverse arrangement of the aorta and pulmonary artery,
- pulmonary stenosis,
- defect of the septum between the ventricles,
- tetralogy of Fallot,
- two or three chambered heart,
- undeveloped or absent spleen,
- pathology of the ciliated epithelium of the bronchi,
- infertility.
The most severe form, in which right-sided localization of the heart is diagnosed, is considered Patau syndrome. Such children have developmental defects in almost all organs, so cases of them reaching school age are rare.
We recommend reading the article about acquired heart defects. From it you will learn about the classification of myocardial defects, the causes of their occurrence in adults and children, diagnosis and treatment.
Find out more about performing a heart biopsy here.
Symptoms
Uncomplicated dextrocardia in combination with complete transposition of internal organs usually does not manifest itself in any way and does not bother the patient at all. Such cases are relatively rare; much more often, dextrocardia is accompanied by other pathologies that can manifest themselves both from the first seconds and over several years of life.
There are no characteristic external symptoms caused by cardiac dystopia, but it can be indirectly indicated by:
- Jaundice discoloration of the skin and sclera from birth;
- Difficulty breathing;
- Cyanosis or pallor of the skin;
- Heart rhythm disturbances.
In older children, in addition to the listed symptoms, the following may be observed:
- Increased susceptibility to infectious diseases of the lungs and upper respiratory tract;
- Increased fatigue, muscle weakness;
- Retarded physical development.
A set of examinations to clarify the diagnosis
Taking a repeat cardiogram
- Repeated ECG. It is imperative to take a repeat cardiogram, especially if EOS displacement is detected for the first time and previous ECGs were normal. An error in the application of electrodes, which may show a distorted result, or a malfunction of the cardiograph cannot be ruled out. It is also always necessary, if possible, to compare a “fresh” ECG with a previous cardiogram to assess the dynamics of the patient’s condition and monitor changes in the work of the heart.
- Ultrasound of the heart. The most informative way to tell about the condition of the heart, its chambers, cardiac ejection fraction, and the flow of blood through the cardiac cavities is with ultrasound or echocardiography. This examination method can be supplemented, if necessary, with Doppler sonography.
- Holter ECG. If the doctor suspects a patient has conduction disturbances or rhythm disturbances, then Holter ECG monitoring will be a reliable assistant in making the diagnosis. A daily recording of a cardiogram will allow the doctor to “catch” the arrhythmia and see in which part of the heart the conductivity is changed. To ensure that Holter data is not distorted, the patient should be given detailed instructions on how to behave during the study.
24-hour blood pressure monitoring - ABPM. With high blood pressure in combination with LV hypertrophy and cardiac axis deviation, the doctor may recommend 24-hour blood pressure monitoring to the patient. This diagnostic method helps to establish a more accurate degree of hypertension and help in selecting optimal doses of antihypertensive drugs.
- Consultation with a cardiac surgeon. Consultation is required if heart defects are suspected, or after they are detected by ultrasound.
It should be understood that deviation to the left of the EOS is not a diagnosis, but an ECG sign, which can be either a variant of the norm or a symptom of numerous diseases. Only a doctor can make a conclusion about what information this symptom carries, after carrying out a set of diagnostic procedures.
Diagnostics
Suspicion of dextrocardia may arise during a routine external examination . The apex beat of the heart is detected on the right side during palpation, percussion shows displacement of cardiac dullness, and auscultation reveals an unusual location of heart sounds.
Additional instrumental studies may be required to confirm the diagnosis:
- X-ray examination;
- Ultrasound of the heart and blood vessels;
- Electrocardiography;
- Magnetic resonance imaging;
- CT scan.
- Angiography and cardiac catheterization.
The choice of examination methods depends on the type and severity of concomitant pathologies.
Since the electrical axis of the heart in dextrocardia is located in a mirror image relative to the norm, the ECG curve looks like a mirror image of the normal one . Electrocardiography is a mandatory type of examination if any cardiac abnormalities are suspected for the differential diagnosis of congenital and acquired pathologies of the cardiovascular system.
How dangerous is the Cantrell pentad and what are its main manifestations? Find out everything about this dangerous vice. Eisenmenger complex can be either a congenital or acquired disease. Find out all the details about him.
Read in detail about coarctation of the aorta in the fetus and newborn in this material - this heart defect is quite well treated.
Heart sounds
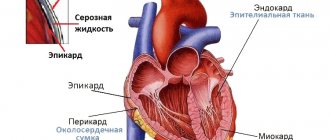
I (systolic) tone occurs predominantly in the phase of isovolumetric contraction of the ventricles of the heart.
Components of the first heart sound
- valve component;
- gastric or muscular (sharp rise in pressure in the ventricle during isovolumetric contraction);
- vascular (oscillations of the initial sections of the great vessels when they are stretched by blood in the expulsion phase);
- atrial (oscillations associated with contraction of the atria).
II (diastolic) heart sound occurs at the very beginning of ventricular diastole due to:
- slamming of the semilunar leaflets of the aortic valve and pulmonary trunk (valvular component);
- vibrations of the walls of the initial sections of these vessels (vascular component).
We recommend
Online English courses with strong teachers from Inglex. For visitors to our website we give 3 lessons using the promotional code WELCOME when paying for 5 lessons with Russian-speaking teachers
Start learning English
Change in heart sounds
- changing the volume of the main tones (I and II);
- splitting (bifurcation) of basic tones;
- appearance of additional tones:
- III and IV tones,
- sounds of mitral valve opening,
- additional systolic sound (click)
- and the so-called pericardial tone.
The volume of the first tone normally depends on the following factors:
- From the tightness of the ventricular chamber during the period of isovolumetric contraction (from the tightness of the closure of the atrioventricular valves);
- From the speed and force of contraction of the ventricles in the phase of isovolumetric contraction, which is determined by:
- intensity and speed of metabolic processes in the myocardium (contractility of the heart muscle);
- on the density of structures involved in oscillatory movements, primarily on the density of atrioventricular valves;
- from the position of the atrioventricular valve leaflets immediately before the onset of the isovolumetric contraction phase.
The volume of the second tone normally depends on the following factors:
- from the tightness of the closure of the semilunar valves of the aorta and pulmonary artery;
- on the rate of closure and oscillation of these valves during the protodiastolic period, which in turn depends on:
- blood pressure level in the main vessel,
- on the density of the structures involved in oscillatory movements, primarily on the density of the semilunar valves, as well as the walls of the great vessels;
- from the position of the semilunar valve leaflets immediately before the onset of the protodiastolic period.
Reasons for weakening of the first tone:
- leaky closure of the atrioventricular valves (with mitral or tricuspid valve insufficiency);
- a sharp slowdown in ventricular contraction and rise in intraventricular pressure with a decrease in myocardial contractility in patients with heart failure and acute myocardial damage;
- a significant slowdown in the contraction of the hypertrophied ventricle ( with stenosis of the aortic mouth);
- unusual position of the atrioventricular valve leaflets immediately before the onset of isovolumetric contraction of the ventricles.
Strengthening the 1st tone:
Causes:
- An increase in the rate of isovolumetric contraction of the ventricles (with tachycardia or thyrotoxicosis, when the rate of all metabolic processes in the body, including the heart, increases);
- Compaction of the heart structures involved in vibrations and the formation of the first sound (with mitral stenosis).
A loud (popping) first heart sound with mitral stenosis is caused both by the compaction of the leaflets of the mitral valve itself, the oscillations of which occur with greater frequency, and by a change in the rate of contraction of the left ventricle and the shape of the intraventricular pressure curve.
Reasons for weakening of the second heart sound:
- violation of the tightness of the closure of the semilunar valves of the aorta and pulmonary artery;
- decrease in the speed of closing of the semilunar valves with:
- HF accompanied by a decrease in the rate of ventricular relaxation
Strengthening (emphasis) of the second heart sound
Causes of enhancement in the aorta:
- increased blood pressure of various origins (due to an increase in the rate of slamming of the aortic valve leaflets);
- compaction of the aortic valve leaflets and aortic walls (atherosclerosis, syphilitic aortitis).
Causes of enhancement in the pulmonary artery:
1) increased pressure in the pulmonary artery (with mitral stenosis, cor pulmonale, left ventricular heart failure).
Split heart sounds:
The main cause of splitting of the first heart sound is asynchronous closure and fluctuations of the mitral (M) and tricuspid (T) valves (right bundle branch block).
Did you like the site? Support us by subscribing on social networks!
- Site group in VK
- Website profile on Twitter
- Site community on Facebook
Additional heart sounds
The third heart sound occurs at the end of the phase of rapid filling of the ventricles after 0.16 - 0.20 seconds. after the second tone. It is caused by a hydraulic shock against the wall of the ventricle of a portion of blood moving under the influence of a pressure gradient from the atrium to the ventricle.
IV heart sound occurs during active atrial systole, i.e. immediately before the first tone. It is caused by a hydraulic shock of a portion of blood from the atrium against the upper front of the blood that filled the ventricle during the previous phases of fast and slow filling.
Remember!
The tone (click) of the opening of the mitral valve, together with the flapping I tone and the II tone accentuated on the pulmonary artery, form a peculiar melody of mitral stenosis, called the “quail rhythm” and reminiscent of the quail singing “it’s time to sleep.”
Treatment
With a diagnosis of cardiac dextrocardia, which is not complicated by concomitant diseases and does not in any way affect the general state of health, treatment is not required.
Treatment tactics in the presence of concomitant pathologies are aimed at eliminating them and are developed depending on the severity of the patient’s condition. Often the only possible way to alleviate the condition and save the patient’s life is surgical intervention.
In preparation for surgery, conservative treatment is performed to stabilize the patient's condition. As part of maintenance therapy, the following is prescribed:
- Diuretics;
- Antihypertensive drugs;
- Drugs that support the heart muscle.
Almost always, patients are prescribed long-term treatment with antibiotics and drugs from the group of probiotics to prevent disorders of the intestinal microflora.
The general regimen can be supplemented with other drugs depending on the characteristics of the disease.
Cardiac axis and ECG
Deviation of the electrical axis of the heart to the left
The human heart has the ability to contract. Electrical impulses sequentially cover the chambers of the heart, originating in the atrial sinus node. If you imagine the course of these pulses in the form of directed vectors, you will notice that they have a similar direction. By summing the directions of the vectors, one main vector can be obtained. This will be the electrical axis of the heart (EOS).
Functional diagnostic doctors often determine EOS from a cardiogram visually, but it is more accurate to do this using special tables. If you look carefully at the QRS complex in leads I, II, III on the ECG, you can see that R II>RI>RIII, this means that the EOS on the cardiogram is normal.
If it is difficult for a doctor to visually determine the axis of the heart, he determines the alpha angle and calculates the EOS using special tables. Without delving into the course of measurements, we note that for a normal EOS angle alpha (RII>RIII), then the doctor’s conclusion will be as follows: deviation of the electrical axis of the heart to the left. EOS deviation is confirmed when the alpha angle is in the range from 00 to -900.
Prognosis and prevention
In the absence of concomitant diseases, there is no threat to the patient’s health and life . The presence of complications from other internal organs increases the risk of developing heart failure, acute infectious diseases, male infertility, and intestinal maltoration.
In severe cases, accompanied by multiple congenital pathologies, patient mortality during the first year of life can exceed 90% (Patau syndrome).
There are no effective measures to prevent dextrocardia . Due to the likely hereditary nature of the anomaly, married couples who have proven cases of dextrocardia among relatives should especially carefully monitor their health during pregnancy planning. General recommendations include adherence to the principles of a healthy lifestyle.
Additional diagnostic methods
If the patient's ECG shows a tendency for the EOS to shift to the right, additional examination is carried out in order to make an accurate diagnosis.
Basically, this indicator indicates an increase in the mass of the right side of the heart.
The following diagnostic methods are used:
- Chest X-ray. The pictures show an enlargement of the heart muscle, if any.
- Ultrasound of the heart. The method allows you to obtain a complete visual picture of the state of the myocardium.
- Holter monitoring. Used in the presence of sinus arrhythmia or tachycardia in the patient.
- Electronic cardiogram with additional load (for example, on an exercise bike) - to determine coronary artery disease.
- Angiography - reveals disturbances in the functioning of the coronary vessels.
- MRI.