One of the most important organs in the human body is the heart. This organ is studied by many specialists working in a variety of sciences. They want to make the chambered heart work for a long time.
How many chambers are there in the human heart?
How many circles of circulation are there, where do they begin and end?
How is the heart muscle nourished?
Our article is dedicated to solving these problems.
A little about cardiac anatomy
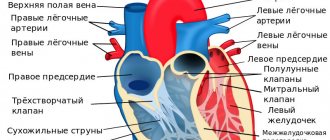
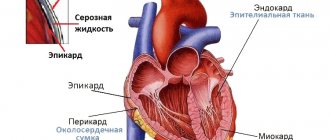
The human heart is a muscular organ, similar to a pouch, consisting of three layers. The organ is covered on the outside with pericardial tissues, which form the so-called protective bag. Under the pericardial layer is the myocardial region, which is a contractile muscular system, as well as the endocardium, which is a thin mucous membrane located in the inner part of the heart chamber.
This human organ is located in the central part of the sternum. It has some deviation from the center line to the left.
The heart consists of four chambers, which are formed by four cavities. Communication between them occurs thanks to valves. The heart has a right and left atrium and a right and left ventricle located underneath them.
The valves that separate the chambers of the heart prevent back bleeding. The ventricles are thick compared to the atrial walls. Their functionality is to push blood into a large vessel (aorta).
At this time, the function of the atria is to passively accept blood fluid.
The structure of the three-chambered heart of a frog
Amphibians have a heart with three chambers.
The ventricle has thick walls. The atria communicate with the ventricle through a common opening. The right atrium is larger in volume. It receives blood from all over the body, which has given off an element of oxidation. The left side of the heart receives blood from the lungs. The venous sinus is connected to the right atrium. It pumps blood to the heart. On the right side is the conus arteriosus. It is also present in lower fish. Includes a number of valves. Serves to pump blood into vessels. In amphibians, the cone is divided into two sections by a septum.
How many chambers are there in the heart during fetal development?
Many people are interested in the question: how many heart chambers exist in a person who is inside the mother’s body before birth. The heart organ also has 4 parts, just like a born person. But communication between the atrial chambers occurs through an opening that is visually similar to an oval and is located in the area of the septum.
A similar hole is needed to drain blood from the right side to the left. But this is not a pulmonary circulation, since the expansion of the lungs did not occur. But the developing respiratory system is supplied with blood, which carries nutrients from the aorta through the cavity of the ductus botallus.
The structure of the heart chambers of a child in embryonic development is slightly different from an adult.
Myocardial contraction occurs only by 30% of the total volume. The functionality of the human heart is related to the glucose entering the mother’s bleeding mass, which is used by the fetal muscles for nutrition.
Ventricular dilatation
The ventricle of the right chamber has an uneven surface on which three muscles are located, the name of which is papillary.
Figure 4 shows a diagram of the right camera.
Figure No. 4_Diagram of the right ventricle
As we can see, the ventricle has 2 holes in the upper region:
- Atrioventricular, with a tricuspid valve, which is attached to tendon threads. They are thin, but very strong.
- Entrance to the pulmonary trunk. It consists of 3 special valves, thanks to which the ventricle can direct blood circulation towards the lungs.
The left atrium has four such openings and two veins. There are no valves in this part of the chamber.
Externally, the left ventricle has 2 papillary muscles connected by a bicuspid valve.
Figure 5 shows the left chamber with the atrium and ventricle.
Figure No. 5_Structure of the left ventricle
The anatomical structure of the heart is such that the valves are inactive and open due to the pressure of blood flow. In other words, this can be explained this way: the muscle enters the contraction phase and because of this, the valves open and allow blood flow into the ventricles. Blood does not enter the atria, because they are protected by papillary muscles and their filaments.
The main reason for the expansion of the cavity of the left ventricle is its overflow with blood. If the semilunar valve is damaged or the ascending aorta is narrowed, then the heart muscle will need more strength and time to expel fluid into the systemic channel. Some of the blood remains in the ventricle, and over time, it stretches.
The right ventricle may increase in size due to problems with the pulmonary valve and increased pressure in the pulmonary circulation. When the pulmonary vessels are too narrow, some of the blood from the pulmonary trunk returns to the ventricle. At this moment, a new portion of fluid enters from the atrium and the walls of the chamber stretch.
The cause of left atrium enlargement is pathology of the valves: atrioventricular or semilunar. It takes a lot of force and time to push blood into the ventricle through a small hole, so some of the blood remains in the atrium. Gradually, the amount of residual fluid increases, and a new portion of blood stretches the walls of the heart chamber. The second cause of dilation of the walls of the left atrium is atrial fibrillation. In this case, the pathogenesis is not fully understood.
The right atrium dilates in the presence of pulmonary hypertension. When the vessels of the lungs narrow, there is a high probability of blood flowing back into the right ventricle. And since it is already filled with a new portion of liquid, the pressure on the chamber walls increases. The atrioventricular valve cannot withstand and turns out.
An aortic aneurysm may be a consequence of dilation of the left ventricular cavity. It occurs in the place where the vessel wall is thinnest. Increased pressure, as well as the rigidity of surrounding tissues due to atherosclerosis, increase the load on the failing areas of the vascular wall. A sac-like protrusion is formed, which creates additional turbulence in the blood flow. An aneurysm is dangerous due to sudden rupture and internal bleeding, as well as a source of blood clots.
Blood supply and circulation
The myocardium is supplied with blood coming from the main vascular system. The heart muscle receives nutrition due to the contraction of the ventricles. This well-functioning mechanism can be disrupted, which leads to myocardial infarction. The chambers of the heart are responsible for pumping fluid that flows in a vicious circle.
The pressure created in the left ventricle allows blood to be carried to the smallest capillaries. Modern medicine distinguishes between the systemic and pulmonary circulation.
The function of the large circle allows you to nourish all tissue areas of human organisms. The pulmonary circulation helps to carry out gas exchange in the pulmonary region, as well as maintain air concentration in the required amount. Each cardiac chamber has vessels that bring blood in and out of the chambers.
The systemic circulation begins from the left atrium. Then the liquid blood substance enters the cavity of the left ventricle and completely fills its volume, which leads to an increase in cavity pressure.
When the water column reaches 120 mm, the semilunar valve opens, which separates the ventricle and the aorta, and blood enters the circulatory system. Then, when the ventricle contracts, blood is released, which reaches the most distant capillaries.
After they are fully filled, the respiratory process in the cells and their nutrition begin. Then the blood is saturated with decay products and enters the venous system. The veins return blood fluid to the heart, namely to the area of the right atrium.
The inferior and superior vena cava are connected to the right atrium. Blood from all parts of the human body is collected here. When the right cardiac chamber is oversaturated with blood, it pushes fluid into the right ventricular cavity, and this is where the pulmonary circulation originates.
At the beginning, the blood is saturated with carbon dioxide and decay products, then it moves to the area of the pulmonary trunk, and then in the pulmonary arteries and capillaries the bad blood changes to good, oxygenated blood.
Then it returns to the left atrial chamber, where a new systemic circulation begins. The whole process takes place within half a minute.
The human body must constantly be fed with the necessary substances and oxygen; for this purpose, the functioning of the heart chambers must be adjusted.
External and internal structure
How many chambers are there in the heart of a person who has not yet been born? There are also four of them, but the atria communicate with each other through the foramen ovale in the septum. At the stage of embryogenesis, it is necessary for the discharge of blood from the right parts of the heart to the left, since there is no pulmonary circulation yet - the lungs are not straightened. But blood still flows into the developing respiratory organs, and it comes directly from the aorta through the ductus botallis.
The fetal heart chambers are thinner and significantly smaller than those of an adult, and only thirty percent of the total myocardial mass contracts. Its functions are closely related to the supply of glucose into the maternal bloodstream, since the child’s heart muscle uses it as a nutrient substrate.
In order for the body to constantly receive the necessary nutrients and oxygen, the chambers of the heart must work very smoothly. There is a natural order of actions.
1. Systole is the contraction of the ventricles. It is divided into several periods:
- Tension: individual myofibrils contract, pressure in the cavity increases, the valve between the atria and ventricles closes. Due to the simultaneous contraction of all muscle fibers, the configuration of the cavity changes, the pressure rises to 120 mm of water column.
- Expulsion: The semilunar valves open and blood enters the aorta and pulmonary trunk. The pressure in the ventricles and atria gradually equalizes, and the blood completely leaves the lower chambers of the heart.
2. Diastole is the relaxation of the myocardium and the period of passive blood intake. The upper chambers of the heart communicate with the afferent vessels and accumulate a certain amount of blood. The atrioventricular valves then open and fluid enters the ventricles.
- Electrocardiography. This is the recording of electronic phenomena that accompany muscle contractions. The chambers of the heart are composed of cardiomyocytes, which generate an action potential before each contraction. It is this that is detected by electrons applied to the chest. Thanks to this imaging method, it is possible to identify gross disturbances in the functioning of the heart, its organic or functional damage (heart attack, defect, expansion of cavities, the presence of additional contractions).
- Auscultation. Listening to the heartbeat was the oldest way to detect heart disease. Experienced doctors using this method alone can identify most structural and functional pathologies.
- Ultrasonography. Allows you to see the structure of the chambers of the heart, the distribution of blood, the presence of defects in the muscle and many other nuances that help make a diagnosis. The method is based on the fact that ultrasonic waves are reflected from solid substances (bones, muscles, organ parenchyma) and pass freely through liquid.
Chambers and valves
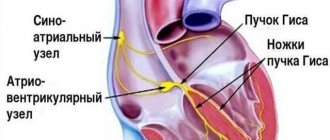
Since the supply of oxygen and nutrients to other organs directly depends on the normal functioning of the heart, it must ideally adapt to changing environmental conditions, operating in a different frequency range. Such variability is possible due to the anatomical and physiological characteristics of the heart muscle:
- Autonomy implies complete independence from the central nervous system. The heart contracts from impulses produced by itself, so the work of the central nervous system does not affect the heart rate in any way.
- Conduction consists of transmitting the generated impulse along the chain to other parts and cells of the heart.
- Excitability implies an instant reaction to changes occurring in the body and outside it.
- Contractility, that is, the force of contraction of fibers, is directly proportional to their length.
- Refractoriness is a period during which myocardial tissue is inexcitable.
Any failure in this system can lead to a sharp and uncontrollable change in heart rate, asynchrony of heart contractions, even fibrillation and death.
To continuously move blood through the vessels, the heart must contract. Based on the stage of contraction, there are 3 phases of the cardiac cycle:
- Atrial systole, during which blood flows from the atria into the ventricles. In order not to interfere with the flow, the mitral and tricuspid valves open at this moment, and the semilunar valves, on the contrary, close.
- Ventricular systole involves the movement of blood further to the arteries through the open semilunar valves. At the same time, the flap valves close.
- Diastole involves filling the atria with venous blood through the open leaflet valves.
Each heartbeat lasts approximately one second, but during active physical work or during stress, the speed of impulses increases due to a reduction in the duration of diastole. During proper rest, sleep or meditation, heart contractions, on the contrary, slow down, diastole becomes longer, so the body is more actively cleansed of metabolites.
In order to fully perform its assigned functions, the heart must not only pump blood throughout the body, but also itself receive nutrients from the bloodstream. The aortic system, which carries blood to the muscle fibers of the heart, is called the coronary system and includes two arteries - the left and the right. Both of them depart from the aorta and, moving in the opposite direction, saturate the heart cells with useful substances and oxygen contained in the blood.
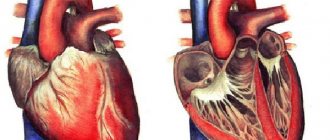
The heart is a hollow muscular organ and has an elongated cone-shaped shape. What the heart looks like from a topographical point of view can be seen in Figure 1.
Figure No. 1_What a heart looks like
The upper part of the organ has an expanded appearance and is called the base. The narrowed lower part is the apex of the heart. Weight varies in the range of 250-300 g for an adult. However, this is an average figure, because... In children, the weight of the organ is less, and in adults, the weight changes depending on physical activity, the emotional component and health. In the figure we see that the surface of the heart is dotted with a system of blood vessels. On the inside there is a system of nerve endings.
The main organ is located in the chest area with a deviation to the left. The outer tissue is fused with the chest cavity and ribs, and the inner tissue covers the entire organ and is fused with the muscle of the organ. Between these parts there is a cavity filled with a special liquid that cushions the organ during diastole and systole.
The external structure of the heart has been studied. Next we will talk about the internal structure of the organ, what the heart consists of, as well as the topography of its components.
The four-chambered heart has three main muscle tissues:
- ventricular myocardium;
- atrial myocardium;
- middle layer of the conductive system.
The muscle has a mesh structure that is formed from fibers. This internal structure of the heart was formed due to interfiber relationships established by lateral bridges. As a result, we see that the system appears to be a narrowly looped sintsitii.
Figure 2 clearly shows the structure of the heart muscle.
Figure No. 2_ Structure of the heart muscle
On the outer surface of the organ there is a transverse venous groove, conditionally separating the parts of the heart.
Figure 3 shows what the organ looks like from the inside.
Figure No. 3_Internal structure of the heart
Now we will cover in detail each of the parts of the heart.
Diagnostics of cardiac dysfunctions
To diagnose various heart ailments, you should first undergo an electrocardiographic examination. During it, electronic phenomena are recorded, accompanied by muscle contraction.
The structure of the heart chambers includes a cardiomyocyte element, which helps generate the effective potential before contraction. This is determined by electrons, which must be applied to the chest area during the examination.
This helps to identify various failures in the functionality of the heart, organic and functional lesions.
Using electrocardiography, it is possible to determine whether a patient is developing a heart attack, defect, cavitary enlargement and other diseases.
By undergoing an auscultation examination, you can determine the disease. Experienced doctors, using this technique, determine a large number of pathological conditions in structure and pathology.
Using ultrasound, you can see the heart organ, consisting of chambers, see how blood is distributed in them, and determine muscle defects. Ultrasound determines the presence of various diseases, and a diagnosis is made based on the results.
With age, people experience an accumulation of various heart ailments, provoked by various pathologies. Often, disruptions in the cardiovascular system can occur even among those who monitor their health and follow a healthy lifestyle.
The most common pathologies are dilatation of the heart chambers, enlargement of the ventricles or atria, enlargement of the aorta, aneurysm and many others.
Heart walls
The walls of the organ have three layers of the heart:
- internal;
- average;
- external.
Each wall has a different tissue thickness. The atria have thin tissue of 2 to 3 mm. The left chamber ventricle has a wall thickness of 9 to 11 mm, and the right chamber has a wall thickness of 4 to 6 mm.
The internal tissue of the human heart covers the chamber and is also responsible for the formation of valve leaflets. The myocardium was formed by muscle tissue (cardiomyocytes), which look like striated grooves. Since the atria have thinner muscle tissue, it consists of 2 layers, in contrast to the three-layer muscle of the ventricles.
The epicardium is shaped like a leaf. It is tightly fused with the myocardium. The outer shell is formed from a sheet of tissue that is covered with flat cells in the pericardial region.
In Figure 6 we can see the structure of the walls of the organ.
Figure No. 6_Walls of the heart
How to treat dilated changes
Dilatation is treated with medications and surgery. It is not possible to reduce the stretching of the heart chambers with the help of pills. Treatment helps eliminate inflammatory signs, normalize high or low blood pressure, rheumatoid, atherosclerotic or pulmonary diseases.
You should lead a healthy lifestyle and do everything that your doctor recommends. It is necessary to thin the blood with the help of medications, which will lead to passage through the heart chambers that have undergone any changes.
If all these measures do not help normalize the functioning of the heart, then it is necessary to carry out an operation during which a pacemaker device is implanted into the patient’s body cavity, which helps the heart wall contract effectively.
Preventive actions
To prevent various pathological conditions in the myocardium, the following rules must be followed:
- stop smoking and drinking alcoholic beverages;
- alternate work with periods of rest;
- Healthy food;
- engage in physical exercise.
To live happily ever after, you should take care of your heart. It is necessary to undergo an annual examination by a cardiologist and do an ECG.