5 / 5 ( 1 voice )
The conduction system of the heart is responsible for its main function - contractions. It is represented by several nodes and conductive fibers. The correct functioning of this system ensures normal heart rhythm.
If any disturbances occur, various types of arrhythmias develop. The article presents a system for conducting impulses through the heart. The importance of the conduction system, its state in normal conditions and in pathology are described.
The conduction system is a complex complex of cardiomyocytes
Opening
On a hot summer day in 1906, Martin Flack, a medical student, studied microscopic sections of a mole's heart while his mentor, Arthur Keith, and his wife cycled through the beautiful cherry orchards near their cottage in Kent, England. Upon his return, Flack excitedly showed Keith “the wonderful structure he had discovered in the mole’s right atrial appendage, exactly where the superior vena cava enters that chamber.” Keith quickly realized that this structure closely resembled the atrioventricular node described by Sunao Tawara earlier this year. Further anatomical studies confirmed the same structure in the hearts of other mammals, which they called the “sinusoidal node” (sino-auricular node). Finally, the long-awaited heart rate generator was discovered.
Beginning in 1909, using a two-string galvanometer, Thomas Lewis simultaneously recorded data from two sites on the surface of a dog's heart, making precise comparisons of the arrival of the excitation wave at different points. Lewis identified the sinusoidal node as the heart's pacemaker through two innovative approaches.
- First, he stimulated the superior vena cava (SVC), coronary sinus, and left appendage and showed that only the waveforms near the sinus node were identical to the normal rhythm.
- Secondly, it was known that the point at which contraction begins becomes electrically negative relative to inactive muscle points. As a result, the electrode near the SAU invariably had a primary negativity indicating: “The nodal area SA is the place where the excitation wave originates.”
Cooling and heating of the sinus node to study the heart rate response was carried out by G Ganter and others, who also indicated the location and primary function of the sinus node. When Einthoven was awarded the Nobel Prize in 1924, he generously mentioned Thomas Lewis, saying: “I doubt that without his valuable contributions I would have the privilege of standing before you today.” [2 - Silverman, ME; Hollman, A. (1 October 2007). "Discovery of the sinus node by Keith and Flack: on the centennial of their 1907 publication]
Special research methods
home>
Publications
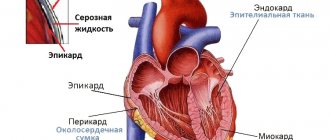
The cardiac muscle consists of two elements that differ in structure and function - the contractile myocardium and the conduction system.
The sinus node (Keith-Fluck) is located in the wall of the right atrium between the mouths of the vena cava. This is an accumulation of multinucleate embryonic fibers rich in sarcoplasm, located in a coarse fibrous connective tissue mesh. The impulse from the sinus node propagates to the atrioventricular node (atrioventricular Aschoff–Tavar node). The atrioventricular node has the same structure as the sinus node, but contains fewer connective tissue and elastic elements. The atrioventricular node passes into the atrioventricular bundle, consisting of fibers that conduct impulses. The atrioventricular bundle passes through the membranous part of the interventricular septum to the left side, where it forms the right and left legs. The right leg on the right side of the septum divides into the anterior middle and posterior branches. The left leg branches along the left side of the septum and forms a dense network of Purkinje fibers. From the sinus node, excitation spreads through the atrium myocardium causing their contraction, after 0.02–003 s the excitation reaches the atrioventricular node and after an atrioventricular delay of 0.04–007 s it is transmitted to the atrioventricular bundle. After 0.03–0.4 s, the excitation reaches the ventricular myocardium, after which systole occurs.
The cardiac cycle is divided into ventricular systole and diastole, at the end of which atrial systole occurs.
The volume of blood ejected by the ventricle of the heart is called stroke, or systolic volume of the heart, and the product of stroke volume and heart rate per minute is called minute volume. The minute volumes of the systemic and pulmonary circulation are normally equal. The minute volume of the heart divided by the body surface area, expressed in square meters (m2) is denoted by the cardiac index. The cardiac index is expressed in liters per minute per 1 m2 of body surface l (min • m2)
The ratio of stroke volume to body surface area is called the stroke index and is expressed in millimeters per minute per 1 m2
ml (min • m2).
At rest in an adult, the cardiac index value is 35 4 l/(min • m2). During physical activity, the minute volume may increase 5-10 times. Normal pressure in the left ventricle and aorta does not exceed 120 mm Hg, and in the right ventricle and pulmonary artery - 25 mm Hg. Normally, there is no pressure difference (gradient) between the left ventricle and the aorta and between the right ventricle and the pulmonary artery. The appearance of a pressure gradient may be due to obstruction in the path of blood outflow or the discharge of blood at the level of the atrium of the ventricles and the pulmonary artery through defects in the septa and abnormal intervascular communications.
The total peripheral vascular resistance is about 1000 dynes/(s • cm 5) and is 3–4 times higher than the total pulmonary resistance. This causes the difference in pressure in the right and left ventricles, in the aorta and the gallbladder artery.
Coronary circulation At rest, the heart absorbs up to 75% of oxygen from the blood flowing through the myocardium (skeletal muscle absorbs 40%) Coronary blood flow is 80-100 ml/min per 100 cm3 of myocardial mass (5% of cardiac output) Coronary blood flow is regulated by changes in the resistance of the coronary arteries When With an increase in oxygen demand, coronary blood flow increases (sometimes 4–5 times) and oxygen absorption remains almost constant. The amount of oxygen absorbed by the myocardium is the dominant factor in the regulation of coronary blood flow.
Special research methods
To establish an accurate anatomical diagnosis, hemodynamic state, and the degree of impairment of myocardial contractile function, noninvasive (electrocardiography, phonocardiography, echocardiography, radiography) and invasive (probing, angiocardiography) research methods are used. Echocardiography makes it possible to visualize intracardiac structures on a screen and, using a computer, to calculate basic hemodynamic parameters. Ultrasound scanning allows you to diagnose defects in the septa of the heart, fibrosis and calcification of the valves, disorders of myocardial contractile function due to cicatricial changes, myocardial hypertrophy and tumors (myxomas) of the heart. Probing of the heart During the study of the cavities of the heart and blood vessels using a catheter connected by an electromagnetic sensor to a mingograph, pressure curves are recorded, blood samples are taken to study the gas composition, a contrast agent is administered and X-ray filming is performed. To study the left parts of the heart through a catheter passed to the right heart, pass a long thin needle curved at the end, which punctures the interatrial septum and penetrates into the left atrium (transseptal puncture). Having removed the needle, the catheter is passed into the left ventricle and aorta.
A catheter passed through the femoral or ulnar artery reaches the ascending aorta and left ventricle. Using special catheters, selective coronary angiography and left ventriculography are performed.
Cinecardiography is of great importance for establishing an accurate diagnosis of many congenital heart defects.
Selective coronary angiography is aimed at determining the patency of the coronary arteries. In chronic ischemic heart disease, it is performed in several projections and at the same time left ventriculography is performed to determine the extent of the zones of hypo, dys and akinesia.
Providing operations on the heart and large vessels
Preoperative preparation of cardiac surgical patients consists of therapeutic measures aimed at reducing the symptoms of heart failure, improving the function of parenchymal organs, and eliminating disturbances in water-electrolyte and protein metabolism.
Artificial circulation During the intracardiac stage of the operation, blood circulation and gas exchange are provided using an artificial circulation apparatus (ACB), which consists of a roller pump, an oxygenator, a heat exchanger and a control system.
Through tubes inserted into the superior and inferior vena cava, blood flows due to gravity into the oxygenator. A bubble oxygenator is used, in which the blood is mixed with the supplied oxygen, and a membrane oxygenator, in which gas exchange is carried out through a special plastic film separating the blood and the injected gases. This sharply reduces injury to formed elements and blood proteins The pump pumps oxygenated blood into the ascending aorta or into the femoral artery Fill the entire extracorporeal system with donor blood for operations in children and blood substitutes, plasma, albumin solution for operations in adults, correcting the electrolyte composition and acid-base state For each 60–80 mg of heparin is added per liter of filling volume. Before connecting the lines into the vein, the patient is also given heparin at a rate of 4 mg/kg. At the end of extracorporeal circulation, heparin is neutralized by introducing a solution of protamine sulfate under the control of indicators of blood coagulation processes.
During operations on adults, artificial circulation is used (at a temperature of 28–24°C), and when correcting some complex congenital defects in children, hypothermia is used. Reducing the temperature can significantly reduce the volumetric perfusion rate, and at a body temperature of 16–18°C even stop blood circulation for 30–40 min At the end of the intracardiac stage of the operation, the blood temperature is gradually increased and the perfusion is completed after the patient is completely warmed to 37°C.
Cardioplegia. Almost all intracardiac operations under artificial circulation are performed on a temporarily stopped, relaxed heart. To achieve such a reversible cardiac arrest, special cardioplegic solutions are used, which, after clamping the ascending aorta, are injected directly into the coronary arteries through special cannulas or into the root of the ascending aorta. Conservation of energy resources is achieved. immediate cardiac arrest and rapid cooling, followed by maintaining the myocardial temperature at 12–16°C. The cardioplegic solution includes: potassium, sodium, chlorine, calcium, glucose, mannitol, albumin. Drugs that protect the myocyte membrane, preventing edema and hypoxic damage are also used. After surgery and the resumption of coronary circulation, the myocardium is warmed and heart contractions are restored.
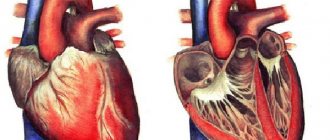
Injuries of the heart and pericardium
Most often, wounds of the heart and pericardium are stab wounds and gunshot wounds. In wounds of the heart, the external soft tissue wound is usually localized on the left half of the chest in front or on the side. However, in 15–17% of cases it is located on the chest or abdominal wall outside the projection of the heart. Wounds of the heart and pericardium are often combined with damage to other organs. Especially often, the upper or lower lobe of the left lung is damaged. Clinic and diagnosis, wounds of the heart and pericardium are characterized by the following signs - bleeding, shock, symptoms of cardiac tamponade. The severity of the condition of the wounded is primarily due to acute cardiac tamponade - compression of the heart by blood pouring into the pericardial cavity. For cardiac tamponade to occur, it is sufficient to have 200–300 ml of blood spilled into the pericardial cavity. If the amount of blood reaches 500 ml, then there is a risk of cardiac arrest. As a result of tamponade, the normal diastolic filling of the heart is disrupted and a sharp decrease in the stroke and minute volume of the right and left ventricles occurs. central venous pressure rises sharply and systemic arterial pressure drops sharply.
The main symptoms of acute cardiac tamponade: cyanosis of the skin and mucous membranes, dilation of the superficial veins of the neck, severe shortness of breath, rapid thread-like pulse, the filling of which drops even more at the moment of inspiration, decreased blood pressure. Due to acute anemia of the brain, fainting and confusion are common. Sometimes there is motor excitement. Physical examination determines the expansion of the boundaries of the heart, the disappearance of the cardiac and apex impulses, and dull heart sounds. If the lung is simultaneously injured, hemopneumothorax appears, as indicated by the presence of subcutaneous emphysema, shortening of the percussion sound and weakening of breathing on the side of the injury.
An X-ray examination reveals an expansion of the heart shadow, which often takes on a triangular or spherical shape, and a sharp weakening of the heart pulsation. The latter is in some cases barely noticeable. The electrocardiogram records a decrease in the voltage of the main waves, signs of myocardial ischemia Treatment: for wounds of the heart, immediate surgery is necessary, which is performed under anesthesia. The choice of access depends on the location of the external wound. The most commonly used is left-sided anterolateral thoracotomy in the fourth-fifth intercostal spaces. When the external wound is located next to the sternum, it is performed longitudinal sternotomy The pericardium is opened and the heart is quickly exposed. Temporarily stop the bleeding by closing the wound hole with a finger. After this, the pericardial cavity is freed from blood and clots. The final closure of the wound opening is carried out by suturing the wound with knotted or U-shaped sutures made of non-absorbable suture material. When cutting sutures, pads made of muscle tissue or synthetic strips are used. The operation ends with a thorough examination of the heart so as not to leave damage in other places. During the operation, the necessary intensive therapy is performed, which includes replenishment of blood loss, correction of disturbed homeostasis. In case of cardiac arrest, a cardiac massage is performed and tonogen (adrenaline) is administered intracardially. In case of ventricular fibrillation, defibrillation is performed. All measures are carried out with constant artificial ventilation. Prognosis: for heart injuries, severe. The outcome depends on the location and size of the wound, the severity of tamponade symptoms, the amount of blood loss, the timing of the operation and the completeness of resuscitation measures.
Congenital heart defects
Congenital heart defects are formed as a result of disturbances in the embryogenesis of the heart or a delay in its normal formation in the postnatal period. Among all heart diseases, they occur in 1–2% of cases. About 0.3–0.4% of all children are born with anomalies in the development of the heart and great vessels. There are more than 100 different types of congenital defects. Congenital heart defects can be conditionally grouped into the following groups. The first group is defects with intracardiac pathological messages causing the discharge of venous blood into the arterial bed (from right to left, primary blue). This group includes the triad, tetralogy and pentade of Fallot, artesia of the tricuspid valve, displacement of the tricuspid valve towards the right ventricle with an atrial septal defect, transposition of blood vessels, etc. The second group is heart defects with intracardiac pathological messages that cause the discharge of arterial blood into the venous bed (from left to right, primary white) - atrial septal defect (non-closure), ventricular septal defect, open ductus arteriosus, aortopulmonary fistula, mitral stenosis with atrial septal defect, etc. The third group - congenital heart defects in which circulatory disorders caused by narrowing of the main vessels of the heart, isolated c-genosis of the pulmonary artery, stenosis of the aortic mouth, coarctation of the aorta.
This section provides information about the most common forms of congenital heart defects, the knowledge of which is necessary for a general practitioner. Isolated narrowing of the pulmonary artery. Isolated pulmonary artery stenosis accounts for 2.5–5% of all patients with congenital heart defects. There are valvular and subvalvular pulmonary artery stenoses. In valvular stenosis, there is no division of the valve into leaflets. The valve is a funnel with a hole facing the lumen of the pulmonary artery. The round-shaped hole is located in the center of the funnel or slightly to the side. Its diameter ranges from 2 to 10 mm. There is always a post-stenotic expansion of the main trunk of the pulmonary artery, often reaching a large diameter. With subvalvular (infundibular) stenosis there is proliferation of fibrous tissue in the form of a ring in the area of the supraventricular crest or in the outflow tract of the right ventricle. Pulmonary artery stenosis is an obstacle to the flow of blood from the right ventricle into the pulmonary circulation. To ensure normal cardiac output, the right ventricle has to do a lot of work. This leads to pronounced hypertrophy of the right ventricle and then to tonogenic and myogenic dilatation. Over time, failure of the right side of the heart develops with decompensation in the systemic circulation.
Clinic and diagnosis: during the examination, shortness of breath is detected, which increases with physical activity, heartbeat, rapid fatigue. During the examination, the presence of a cardiac hump, systolic trembling in the second and third intercostal spaces at the left edge of the sternum, rough systolic murmur and weakening of the second tone above the pulmonary artery are noted. Blood pressure is reduced to 90/50–95/65 mm Hg. Venous pressure is increased.
On the electrocardiogram, there is a pravogram, sometimes an increase in the P wave, a shortening of the P-Q interval. On the phonocardiogram, a systolic murmur in the form of a diamond is recorded at the point of the pulmonary artery. On an X-ray examination, there is an increase in the shadow of the heart due to the right ventricle, an increase in the second arch along the left contour of the heart due to post-stenotic dilatation of the pulmonary artery In the second oblique position - filling of the aortic window with the dilated pulmonary artery. The pulmonary pattern is normal. The x-ray kymogram shows an increase in pulsation teeth along the contour of the right ventricle, a decrease in the pulsation of the roots of the lungs. The final diagnosis of the defect is made based on the results of an intracardiac study, which reveals an increase in pressure in the cavity of the right ventricle. It can reach 300 mm Hg; note a high pressure gradient between the right ventricle and the pulmonary artery. Recording pressure in the right ventricle and pulmonary artery and selective angiocardiography make it possible to make a differential diagnosis between valvular and subvalvular stenoses, determine the degree of narrowing, as well as the nature of dilatation of the right heart. The prognosis is unfavorable without surgery. The life expectancy of patients is no more than 20 years.
Treatment: surgical The operation is performed under conditions of hypothermia and artificial circulation. In case of valvular stenosis, the initial section of the pulmonary artery trunk is dissected and a commissurotomy is made with scissors or a scalpel - up to the walls of the pulmonary artery. In case of infundibular stenosis, the outflow tract of the right ventricle is dissected, the fibrous ring is radically excised. If it is not possible to expand the infundibular section, then a patch of synthetic material is sewn into the cardiotomy hole .
Congenital aortic stenosis. Aortic stenosis occurs in 5–6% of all patients with congenital heart defects. There are valvular, subvalvular and supravalvular stenoses.
With valvular stenosis, there is fusion of the semilunar valves along the commissures. The fused valves have the shape of a dome with a hole at the top. Often, instead of the usual three semilunar valves, there are only two. A post-stenotic expansion of the ascending aorta is observed above the narrowed valve. Subvalvular stenosis has the appearance of a fibromuscular ridge or a thin connective tissue diaphragm with a hole in the center. Supravalvular stenosis is localized in the lower third of the ascending aorta and is caused by hypoplasia of its wall in a limited area or a narrowing such as the diaphragm.
Stenosis of the aortic mouth prevents the ejection of blood from the left ventricle into the systemic circulation, which contributes to severe overload of the left ventricle and creates conditions for its hypertrophy and subsequent dilatation. Hemodynamic disturbances caused by stenosis are manifested primarily by disorders of the coronary and cerebral circulation. Left ventricular failure, due to the large compensatory capabilities of the left ventricular myocardium, occurs relatively late, but once it occurs, it very quickly leads the patient to death.
Clinical features and diagnostics with significant stenosis are characterized by symptoms, shortness of breath, fatigue, attacks of cardiac asthma, anginal pain, dizziness, fainting. An objective examination reveals a sharply intensified and shifted to the left apical impulse, rough systolic tremor in the projection of the aortic mouth. In the second intercostal space on the right, a systolic noise that is carried out on the vessels of the neck. The pulse is weakly filled and tense, pulse pressure is reduced, systolic does not exceed 80/90 mmHg, diastolic is normal or slightly increased.
Sphygmography reveals that the carotid pulse curve has a steep rise with a notch at the top in the form of a cock's crest. The electrocardiogram shows a levogram, signs of myocardial ischemia, and sometimes atrial fibrillation. The phonocardiographic recording of systolic murmur has a diamond shape. X-ray examination reveals a typical aortic configuration of the heart with a pronounced waist, a hypertrophied and enlarged left ventricle, expansion of the aorta in its ascending part. The x-ray shows rough teeth along the contour of the left ventricle. Angiocardiography allows you to accurately determine the anatomical features, location and size of the narrowing, and simultaneous determination of pressure in the aorta and left ventricle – digital value of the pressure gradient caused by stenosis.
With a slight narrowing of the aortic mouth, patients often live up to 40–50 years. With severe stenosis, the prognosis is unfavorable. Patients often die from sudden cardiac arrest due to severe disturbances of the coronary circulation.
Treatment is surgical. It is indicated for a pressure gradient exceeding 30 mm Hg. The operation is performed under conditions of hypothermia and artificial circulation. In case of valve stenosis, in the case of preserved leaflets and pronounced commissures, the latter are dissected, resulting in the restoration of the mobility of the leaflets. A similar commissurotomy is possible in children In adults due to calcification and thickening of the leaflets, elimination of stenosis becomes possible by excision of the valve followed by its prosthetics. In supravalvular stenosis, the aorta above the site of narrowing is dissected in the longitudinal direction, the fibrous ring or connective tissue diaphragm is excised, and the lumen of the vessel is expanded by sewing a patch of synthetic material into the incision walls of the aorta In case of subvalvular stenosis, the effect can be achieved only by partial excision of the narrowed area. It must be taken into account that there are fibers of the atrioventricular bundle nearby, damage to which can cause complete transverse heart block.
| back | forward |
Next: Chapter 6 Diagnosis of chronic prostatitis.
Veins of the systemic circulation.
Two-faced Janus.
About the types of physical exercise.
3. “baby yoga”.
Examples of treatment of some diseases.
Wealth and health - the recipe is the same..
Home
>
Publications
0.0007
Location and structure
The sinoatrial node consists of a group of specialized cells located in the wall of the right atrium, just transverse to the opening of the vena cavae at the junction where the superior vena cava enters the right atrium. The SA node is located in the myocardium. This deep formation abuts the cardiac myocytes belonging to the right atrium, and its superficial part is covered with adipose tissue.
This elongated structure, which extends 1 to 2 cm to the right of the margin of the appendage, represents the crest of the right atrial appendage, and extends vertically into the superior portion of the terminal groove. SA node fibers are specialized cardiomyocytes that vaguely resemble normal, contractile cardiac myocytes. They have some contractile filaments, but they do not compress as tightly. In addition, the fibers of the SA node are noticeably thinner, more tortuous, and stain less intensely than cardiac myocytes.
Symptoms
Manifestations depend on the form and severity of pathological abnormalities. Possible signs include:
- Chest pain. The intensity varies, from a slight tingling sensation to severe bouts of discomfort. Despite its vivid expression, it is impossible to talk about its origin without a thorough diagnosis.
- Feeling of skipping heartbeats, fluttering, loud beating. In this case, tachycardia is replaced by the opposite phenomenon. Episodes last from 15 to 40 minutes or a little more.
- Dyspnea. The ineffectiveness of the pulmonary structures is due to tissue hypoxia. In this way, the body tries to normalize oxygen metabolism. At the initial stage, when there are no defects yet (the size of the heart is normal, the muscle layer is also normal, the systems work stably), the symptom occurs only with increased activity. It's still difficult to notice. In the later stages, intense shortness of breath appears even at rest. As part of advanced diagnostics, specific tests are carried out (bicycle ergometry as an example).
- Arrhythmias of a different type. In addition to accelerating the work of the heart, fibrillation, group or single extrasystoles.
The danger of a particular type is determined during an ECG and dynamic monitoring. Potentially lethal forms develop somewhat later from the onset of the main pathological process.
Cerebral structures suffer as a result of hemodynamic disturbances and decreased nutrition of the brain:
- Tinnitus, ringing.
- Vertigo. It gets to the point where the patient cannot orientate himself normally in space. The inner ear and cerebellum suffer.
- Cephalgia of unknown origin. The character resembles that of high blood pressure or migraine.
- Fainting, syncope. Up to several times a day.
- Mental disorders. According to the type of depressive episodes of a long nature, aggressiveness, increased irritability.
- Cognitive and mnestic deviations. The patient cannot remember important things or fill in new information. The efficiency of thinking decreases.
- Feeling of numbness in the limbs, weakness, drowsiness.
General symptoms:
- Paleness of the skin.
- Cyanosis of the nasolabial triangle.
- Decreased ability to work and the ability to take care of oneself at home.
Symptoms of sinus node weakness are determined by cerebral, cardiac and general manifestations.
Innervation
The sinus node is richly innervated by the parasympathetic nervous system (tenth cranial nerve (vagus nerve)) and fibers of the sympathetic nervous system (thoracic spinal nerves at the level of ridges 1-4). This unique anatomical location makes the SA node susceptible to apparently coupled and opposing autonomic influences. At rest, the functioning of the node mainly depends on the vagus nerve or its “tone”.
- Stimulation through the vagus nerves (parasympathetic fibers) causes a decrease in the speed of the SA node (which in turn reduces the heart rate). Thus, the parasympathetic nervous system, through the action of the vagus nerve, has a negative inotropic effect on the heart.
- Stimulation through sympathetic fibers causes an increase in the speed of the SA node (this increases the heart rate and contraction strength). Sympathetic fibers can increase the force of contraction because, in addition to innervating the sinus and atrioventricular nodes, they directly act on the atria and ventricles.
Thus, disruption of innervation can lead to the development of various cardiac disorders. In particular, heart rate may increase or decrease and clinical signs may occur.
Classification
Typification of the pathological process is carried out for a number of reasons.
Based on the origin of the disease, they talk about the following types:
- Primary SSSU. Develops against the background of cardiac problems themselves. Some doctors (theorists and practitioners) understand by this term the formation of a process without external factors. This is an extremely rare situation.
- Secondary variety. Formed under the influence of extracardiac causes. Occurs in 30% of recorded cases.
Depending on activity, flow:
- Latent type. Determined in 15% of situations. This is the mildest form in most cases, as it has no symptoms and does not progress over a long period of time. The opposite option is also possible, when there is movement forward, there is also aggravation, but the patient does not feel anything.
- Acute manifesting. It is characterized by the appearance of a severe attack of tachycardia or weakening of heart rate, with pronounced manifestations from cardiac structures and the nervous system. It is often impossible to immediately distinguish sick sinus syndrome from other abnormalities. Further, the course of the disease is determined by constant relapses.
- Chronic type. Symptoms are constantly present. But there are no exacerbations as such. The intensity of manifestations is also minimal. Basically it makes itself known by tachycardia.
According to the severity of objective organic deviations:
- Compensated form. The heart is still coping with disruptions. Adaptive mechanisms are activated, adequate myocardial contractility is observed.
This state of affairs can persist for years; in this case, the patient does not even suspect that he is sick.
There are no symptoms or the clinical picture is minimal. Mild palpitations, slight shortness of breath or tingling in the chest. That's all that arises against the background of this type.
- Decompensated form. Occurs more often. This is a classic option, in which the symptoms are sufficiently pronounced to identify health problems. But the manifestations are nonspecific. An objective diagnosis is required.
Finally, based on their variants of the clinical picture and the predominant symptom:
- Bradycardic appearance. Heart rate decreases. Sometimes to a dangerous minimum of 40-50 beats per minute. It happens less. There is a threat of acute conditions, such as stroke or Morgagni-Adams-Stokes attacks. Requires implantation of a pacemaker.
- Mixed, bradytahisystolic type. There is an alternating alternation of acceleration and deceleration of the heart rate. Other arrhythmias may be involved, which worsens the prognosis. The quality of life falls proportionally.
The presented classifications are clinically important because they allow one to determine the vector of diagnosis and develop competent therapeutic tactics.
Functionality
- Main pacemaker
Although some of the heart cells have the ability to generate electrical impulses (or action potentials) that cause cardiac contraction, the sinoatrial node usually initiates the heart rhythm simply because it generates impulses faster and stronger than other areas with impulse-generating potential. Cardiomyocytes, like all muscle cells, have refractory periods after contraction, during which additional contractions cannot be evoked. At such moments, their action potential is redefined by the sinoatrial or atrioventricular nodes.
In the absence of external neural and hormonal control, cells in the sinoatrial node, located in the upper right corner of the heart, will naturally discharge (produce action potentials) in excess of 100 beats per minute. Because the sinoatrial node is responsible for the rest of the electrical activity of the heart, it is sometimes called the main pacemaker.
Diagnostics
Cardiologists examine patients. Specialists in central nervous system pathologies and hormonal problems may also be involved in determining the origin of the process.
List of events:
- Oral interview of a person and collection of anamnestic data.
- Blood pressure measurement, heart rate counting.
- Electrocardiography. Basic technique. Provides an opportunity to determine the nature of functional disorders in the short term.
- Daily monitoring. The idea is to assess blood pressure and heart rate over a 24-hour period.
- Echocardiography. Visualization of cardiac structures. One of the main methods for early detection of organic defects.
- MRI when indicated to obtain clear images.
- Coronography.
Also assessment of neurological status, blood test for hormones, general, biochemical. Diagnosis is carried out on an outpatient or inpatient basis. In the second case it happens faster.
Clinical significance
Sinus node dysfunction results in irregular heartbeats caused by abnormal electrical signals from the heart. When the sinus node of the heart malfunctions, the heart rate becomes abnormal—usually too slow. Sometimes there are pauses in its effect or combination, and very rarely the rhythm is faster than usual.
Occlusion of the arterial supply to the sinus node (most often due to myocardial infarction or advanced coronary artery disease) can cause ischemia and cell death in the SA node. This often disrupts the pacemaker activity of the SAU and leads to sick sinus syndrome.
If the SA node does not work or the impulse generated in it is blocked before it travels down the electrical conduction system, a group of cells located further down the heart act as second-order pacemakers. This center is usually represented by cells within the atrioventricular node (AV node), which is the area between the atria and ventricles, within the atrial septum.
If the AV node also fails, Purkinje fibers can sometimes act as the default pacemaker. If Purkinje fiber cells do not control heart rate, it is most often because they generate action potentials at a lower frequency than the AV or SA nodes.
The mechanism of occurrence of pathology
Understanding the essence of the development of the disease lies in determining the anatomical and physiological features.
The syndrome is based on a disruption of the normal activity of the sinus node. This is a special cluster of cells responsible for generating an electrical impulse of sufficient power. Under adequate conditions, the heart works autonomously, without external stimulation factors. Generating a signal is the task of the pacemaker.
Under the influence of certain moments, the intensity of the electrical impulse decreases. It continues to be carried out along special fibers to the atrioventricular node and further along the branches of the His bundle, but the force is so small that it does not allow the myocardium to contract completely.
Recovery is carried out using radical, but not always surgical, methods. The idea is to stimulate the “lazy” heart.
As the pathological process progresses, an even greater weakening in the work of myocytes is observed.
Myocardial contractility is impaired, blood output decreases, and hemodynamics suffer. Total functional defects often lead to organ failure, heart attack or coronary insufficiency.
Sinus node dysfunction
SA node dysfunction refers to a number of conditions that cause physiological inconsistency in the atria. Symptoms may be minimal or include weakness, effort intolerance, rapid heartbeat, and fainting. The diagnosis is made on the basis of an ECG. Symptomatic patients require a pacemaker.
Sinus node dysfunction includes
- Life-threatening sinus bradycardia
- Alternating bradycardia and atrial tachyarrhythmias (bradycardia and tachycardia syndrome)
- Sinoatrial blockade or temporary stoppage of the automatic control system
- Exit blockade of self-propelled guns
Sinus node dysfunction occurs primarily in older people, especially those with other heart disorders or diabetes.
Sinus arrest is a temporary cessation of sinus node activity, observed on the ECG as disappearance of P waves within a few seconds.
A pause usually causes evacuation activity in lower pacemakers (eg, atrial or connective), preserving heart rate and function, but prolonged pauses cause dizziness and syncope.
With the exit block of the SA node, its cells are depolarized, but the transmission of impulses to the atrial myocardium is disrupted.
- With 1st degree block of SAU, the impulse slows down slightly, but the ECG remains normal.
- With blockade of the 2nd degree ACS of type I, pulse conduction slows down until complete blockade. On the ECG, abnormalities are visible as PP intervals, which gradually decrease until the P wave disappears altogether. Instead, there is a pause and grouped strikes. The pulse delay duration is less than 2 PP cycles.
- During blockade of type II SAU of the 2nd degree, the conduction of impulses is blocked without previous slowdown, resulting in a pause that is a multiple of the PP interval and appears on the ECG as grouped heartbeats.
- With 3rd degree ACS blockade, the conduction of impulses is completely blocked; There are no P waves, resulting in complete failure of the sinus node.
Etiology
Sinus node dysfunction can develop when the heart's electrical system is damaged due to organic or functional abnormalities. Causes of sinus node dysfunction include:
- Aging . Over time, age-related wear and tear on the heart can weaken the sinus node and cause it to malfunction. Age-related damage to the heart muscle is the most common cause of sinus node dysfunction.
- Medications . Some medications to treat high blood pressure, coronary artery disease, arrhythmias, and other heart conditions may cause or worsen sinus node function. These drugs include beta blockers, calcium channel blockers, and antiarrhythmics. Still, taking heart medications is extremely important and, if you follow your doctor's recommendations, in most cases they do not cause problems.
- Heart surgery : Surgery involving the upper chambers of the heart can create scar tissue that blocks electrical signals from the sinus node. Postoperative scarring of the heart is usually the cause of sinus node dysfunction in children with congenital heart disease.
- Idiopathic fibrosis of the SA node , which may be accompanied by degeneration of the underlying elements of the conduction system.
Other causes include drugs, excessive vagal tone and various ischemic, inflammatory and infiltrative disorders.
Symptoms and signs
Often, sinus node dysfunction does not cause symptoms. It is only when the condition becomes serious that problems arise. Even signs of the disease may be vague or caused by other pathologies.
Symptoms of sinus node dysfunction include:
- Fainting or lightheadedness caused by the brain not getting enough blood from the heart. Dizziness may also occur.
- Chest pain (angina-type) occurs when the heart lacks oxygen and nutrients.
- Fatigue caused by a malfunction of the heart, which does not pump blood efficiently enough. When blood flow decreases, vital organs do not receive enough blood. This can leave muscles without enough nutrition and oxygen, causing weakness or lack of energy.
- Dyspnea occurs mainly when heart failure or pulmonary edema is associated with dysfunction of the SA node.
- Poor sleep caused by abnormal heart rhythm. Sleep apnea, in which a person experiences pauses in breathing, can contribute to sinus node dysfunction by reducing the supply of oxygen to the heart.
- Abnormal heartbeat changes most often in the direction of increased heart rate (tachycardia). Sometimes you feel that the rhythm is incorrect or, on the contrary, you feel a pounding in your chest.
Diagnostics
After the doctor takes a medical history and performs a physical examination, tests used to diagnose sinus node dysfunction are ordered. Most often these include:
- Standard electrocardiogram (ECG). Widely used to detect irregular heart rhythm. Before the test, electrodes are placed on the chest, arms and legs to provide a comprehensive measurement of the heart. Wires attach the electrodes to equipment that measures the electrical activity of the heart and converts the impulses into lines that look like a series of teeth. These lines, called waves, show a specific part of the heart rate. During an ECG analysis, the doctor examines the size and shape of the waves and the amount of time between them.
- Holter monitoring . The device continuously records your heartbeat for 24-48 hours. Three electrodes attached to the chest are connected to a device that the patient carries in his pocket or wears on a belt/shoulder strap. Additionally, the patient keeps a diary of his actions and symptoms while wearing the monitor. This allows doctors to determine what exactly was happening at the time of the rhythm disturbance.
- Event Monitor . This method records the heartbeat only when symptoms of the disease are experienced. An event monitor may be used instead of a Holter monitor if the patient's symptoms occur less frequently than once a day. Some event monitors have wires that connect them to electrodes attached to the chest. The device automatically starts recording when it detects an irregular heartbeat, or the patient starts recording when symptoms occur.
- Treadmill stress test e. This testing can be performed to determine the appropriate response to training, represented by a change in heart rate.
Forecast
The prognosis for sinus node dysfunction is ambiguous.
If untreated, mortality is about 2%/year, mainly as a result of progression of the underlying disease, often representing structural heart disease.
Each year, approximately 5% of patients develop atrial fibrillation, causing complications such as heart failure and stroke.
Causes
Development factors are divided into two groups. Primary ones are caused by disruption of the heart itself, as well as blood vessels. Secondary - extracardiac events and diseases.
Primary
- IBS. Accompanies patients over 40 years of age. In rare cases, disturbances may form in the early period.
The bottom line is the impossibility of normal blood supply to the cardiac structures themselves.
Due to constant hypoxia, organic disorders develop: muscle mass increases, chambers expand. Sinus node weakness is a possibility, but is not always observed.
- Autoimmune pathologies affecting cardiac structures and blood vessels. Vasculitis, rheumatism, systemic lupus erythematosus and others.
Affects the muscle layer. Tissue destruction leads to their replacement with scar fragments and the development of cardiosclerosis.
They cannot contract and do not have elasticity, hence the impossibility of adequate work. Blood is pumped with less intensity.
Over the course of several years, this may result in total multiple organ dysfunction or emergency conditions.
- Inflammation of the heart (myocarditis) and surrounding structures. Infectious, less often autoimmune genesis. Recovery within the walls of a hospital, with the use of antibiotics and corticosteroids. Untimely assistance leads to tissue destruction, a minimum of severe disability, and a maximum of death.
- Cardiomyopathy. Violation of the growth of the muscle layer or expansion of the chambers of the heart. Both conditions are potentially fatal without timely treatment. Radical treatment is impossible; the use of supportive drugs is required to stop the process. The duration of the beneficial effect is a lifetime.
- Heart operations. Even seemingly insignificant ones, such as radiofrequency ablation and others. There are no safe interventions on cardiac structures. There is always a risk of complications. So, against the background of cauterization of a large area or if a functionally active, healthy area is treated, the likelihood of arrhythmia is higher.
- Heart injuries. These are caused by chest bruises and rib fractures. Congenital and acquired organic abnormalities in the development of cardiac structures. Multiple in nature. The most typical are mitral valve prolapse, other conditions that cause reverse blood flow (regurgitation), aortic insufficiency and many others. In the early stages they do not manifest themselves in any way. There may be no symptoms of defects until death occurs.
In rare cases, advanced hypertension.
Secondary factors
Non-cardiac problems are less common:
- Intoxication of a pronounced nature. There are many reasons for the condition. From advanced stage cancer processes to poisoning with metal salts, decompensated liver diseases.
- Autonomic dysfunction (AVD) occurs frequently. There may be a temporary weakening of the sinus node as a result of vomiting, coughing, changes in body position, weather dependence, or playing sports. Dystonia also plays a role. But this is not a diagnosis, but a symptom of a particular disease.
- Overdose of antihypertensive and cardiac stimulating drugs. Long-term use of these funds leads to a similar result.
- Metabolic processes associated with impaired metabolism of potassium and magnesium.
- Syphilis, HIV, tuberculosis. Dangerous infectious or viral processes.
- Age from 50 years. The body loses the ability to adequately adapt to harmful external and internal factors. Therefore, the risks of developing cardiac pathologies are higher.
- Prolonged fasting, cachexia. It develops as a result of objective processes (cancer, infections, Alzheimer's disease, vascular and other dementia) or conscious refusal of food (diet, anorexia).
- Endocrine lesions. Diabetes, hyperthyroidism (excessive production of thyroid hormones), the reverse process, deficiency conditions in the adrenal glands.
In the absence of evidence for organic pathologies, they speak of an idiopathic form. This is also a common option.
Recovery consists of relieving symptoms. The effectiveness of such a measure is controversial; without the etioropic component, the effect is incomplete.
Heart functions
Before talking about the classification of pacemakers or pacemakers, it should be said about the main functions of the heart:
- The heart has automatism , which means the ability of the pacemaker system to independently produce excitation impulses in a self-oscillatory mode. The higher-lying sections of the conduction system have a depressing effect on the underlying ones, since the pacemaker of the first order has greater automaticity than the pacemaker of the heart of the second, third or fourth order.
- The heart has excitability , which means the ability of cardiomyocytes to be excited under the influence of stimuli of various origins, chemical or physical.
- The heart has conductivity , which means the ability of cardiac structures to conduct excitation from one participant of the pacemaker system to another due to a change in the action potential.
- The heart has contractility , which means the ability of the heart muscle to contract under the influence of electrical impulses, and the greater the length of the muscle fiber, the greater the contraction.
- The heart is refractory , which means the ability of cardiomyocytes to be temporarily unresponsive to any impulses after contraction. The function ensures the restoration of the action potential in the cells and the relaxation of the heart muscle.
ATRIOVENTRICULAR NODE
The atrioventricular node is located to the right of the interatrial septum above the insertion of the tricuspid valve leaflet, directly adjacent to the orifice of the coronary sinus. Its shape and size are different: on average, its length reaches 5-6 mm, and its width - 2-3 mm.
Like the sinus node, the atrioventricular node also contains two types of cells - P and T. However, there are significant anatomical differences between the sinoauricular and atrioventricular nodes. The atrioventricular node has much fewer β cells and a small amount of collagen connective tissue network. It does not have a permanent, centrally running artery. In the fatty tissue behind the atrioventricular node, near the mouth of the coronary sinus, there are a large number of fibers and ganglia of the vagus nerve. The blood supply to the atrioventricular node occurs through the ramus septi fibrosi, also called the artery of the atrioventricular node. In 90% of cases it arises from the right coronary artery, and in 10% from the ramus circumflexus of the left coronary artery.
The cells of the atrioventricular node are connected by anastomoses and form a mesh structure. In the lower part of the node, before the transition to the His bundle, its cells are located parallel to each other.