Mechanism of clot formation
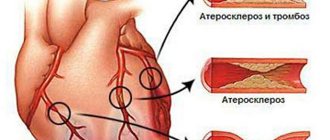
Normally, blood constantly circulating in the body should not clot during a person’s life if the vessel has not been damaged. As a result of changes in the composition of the blood due to various reasons, a violation of its coagulation occurs. A clot, whose main function is to prevent blood loss, is formed by platelets and fibrin. But when it comes to thrombosis, clots pose a serious danger, clogging blood vessels. Thrombi are divided into parietal or obturating - those that completely block the lumen of the vessel. The latter threaten the patient's life.
Thrombosis is a concern for many, even relatively healthy people.
There are also so-called emboli - clots that have broken off from the vascular wall and circulate in the bloodstream. They are dangerous because they can cause blockage of any artery. A thrombus in the left ventricle of the heart is especially dangerous. It is this section of the organ that serves as the beginning of blood circulation.
Features of blood clots
There are several forms of blood clots, which differ in appearance and structure. Depending on the type of vessel, blood clots can be:
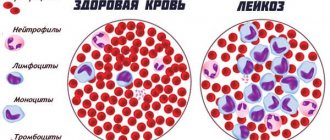
- red (formed in the veins and consists of red blood cells, fibrin, leukocytes and platelets);
- white (occur in the arteries and consist of the same cells, except red blood cells);
- hyaline (detected in capillaries of various calibers and contain protein components instead of fibrin).
Intracardiac thrombi are characterized by a mixed structure. They are variegated in appearance, so the second common definition is layered thrombi. The main parts of their structure are the head, body and tail. The initial element is like a white clot, and the last one is like a red one. It is the “white” part that in most cases attaches the blood clot to the endocardium (the inner lining of the heart).
Intracardiac thrombi can be mobile or immobile. The former are more dangerous because they can move through the ventricles and atria, often entering the general circulatory system. The main place of their formation is the left atrium.
Depending on the relationship of the thrombus to the heart cavity, occlusive and parietal thrombi are distinguished. The former often cause the death of the patient because they block the path of blood flow by completely blocking the lumen of the cavity. The second type of thrombus is more often determined and often occurs against the background of inflammatory processes passing from the endocardium to the valve structures. Due to their attachment to the atrial appendages, free space remains for blood flow, but it can be significantly narrowed, which also affects the course of the disease. Parietal thrombi are mainly formed due to coronary heart disease, chronic heart failure, and aortic aneurysm.
Etiology
This disease is constantly being studied by medical practitioners. Today, the main goal of medicine is to prevent thrombosis. But for this it is necessary to determine the exact reasons for its occurrence. It was found that a heart clot is formed due to vascular atherosclerosis or increased blood clotting, and the causes of these pathologies are different. Risk factors include:
- heart valve defects;
- atrial fibrillation;
- myocardial infarction;
- hypertension;
- endocrine diseases;
- inflammatory diseases of the cardiovascular system;
- injuries;
- bacterial infections;
- blood pathologies;
- frequent stress;
- physical inactivity;
- smoking;
- alcohol abuse;
- poor nutrition.
Today, the main goal of medicine is to prevent thrombosis.
In addition, some diseases that are not directly related to heart function may play a role. Often these are acute respiratory infections, such as tonsillitis or influenza. These diseases affect lung function, which causes problems in the functioning of the heart.
It is possible to identify certain groups of people who have been diagnosed with a ventricular thrombus. According to statistics, among patients of cardiologists:
- men over 40 years old;
- women experiencing menopause;
- pregnant women;
- patients during the recovery period after surgical treatment of thrombosis;
- people with alcohol addiction;
- smokers.
This case lists the most common causes of blood clot formation in the heart.
Small blood clots form in the vessels
Symptoms of a blood clot in the heart
With a polyp-like thrombus, signs of the disease may be absent for a long time, rarely manifesting themselves in tachycardia and shortness of breath, especially in a sitting position. When a blood clot moves, a person experiences the following symptoms:
- attacks of rapid heartbeat, which the patient feels as fluttering or movement of a foreign body in the chest;
- cyanosis of the skin;
- increased sweating;
- dizziness, lightheadedness;
- loss of consciousness;
- weakening of the pulse on the radial artery.
Thrombosis of the left atrium is often accompanied by gangrene of the fingers, a drop in blood pressure to a critical level and suffocation. A thrombus that bursts in the right atrium almost always leads to pulmonary thromboembolism and death from ischemic stroke.
The appearance of blood clots against the background of existing cardiovascular diseases is evidenced by the following facts:
- when using antiarrhythmic drugs, a positive effect is not achieved;
- the patient began to develop pulmonary hypertension;
- Medications do not relieve an attack of severe pain in the heart.
It is impossible to recognize a blood clot on the heart or in blood vessels without special diagnostic procedures. At risk are all people who lead a sedentary lifestyle, suffer from obesity, hypertension, and also have bad habits. Alcohol abuse and smoking lead to the development of an aneurysm, which, in turn, leads to thrombosis. If the patient has previously undergone heart surgery or has relatives with this disease in his family, this is an indication for two-time annual checks.
Symptoms
Unfortunately, signs of a blood clot in the heart become obvious when it has already broken off. Therefore, it is so important to know the symptoms of blockage of blood vessels or even blood thickening. Clinical manifestations will largely depend on the location. Small blood clots form in the vessels. However, the signs are not always noticeable. Sometimes patients experience slight discomfort, but they usually do not pay attention to it.
Recognizing the disease is often very difficult due to the fact that the clinical picture is blurred, too general and may indicate a number of diseases.
The first signs of a blood clot in the heart:
- increased sweating;
- increased heart rate, sometimes weakening;
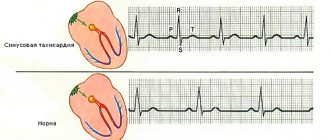
- tachycardia;
- lowering blood pressure;
- pallor or bluishness of the skin;
- numbness in the left shoulder or entire arm;
- fainting.
Angina pectoris
The most significant sign will be obvious blood thickening, which can only be confirmed by tests.
Symptoms of thickening will be: pathological fatigue, cyanosis, headaches, hypertension.
Complications and their consequences
The most dangerous complication of cardiac thrombosis is separation of the floating part and blockage of blood vessels. When a blood clot is located in the veins of the systemic circulation, right atrium or ventricle, the greatest danger is pulmonary embolism. The severity of the condition depends on the size of the blocked vessel.
When large ones are obstructed, a pulmonary infarction occurs. In this case, patients may feel pain in the chest, difficulty breathing, fever and severe weakness. There may be a drop in blood pressure and an increase in heart rate. The prognosis is unfavorable—in most cases, immediate death occurs.
Blood clots enter the systemic circulation from the left sections, from where they can move in two directions - up and down. If a blood clot breaks off in the heart and moves upward, it eventually ends up in the blood vessels of the brain. As a result, symptoms of ischemic stroke develop.
Thromboembolism of the arteries of the lower extremities, damage to the renal and mesenteric vessels occurs when the thrombus moves downwards. The most difficult course of thrombosis of the mesenteric arteries is the development of clinical peritonitis with subsequent necrosis of the mesentery. Obstruction in the lower extremities has a more favorable outcome due to the developed collateral blood flow in them.
Severance of a blood clot from the left side of the heart can lead to the following consequences:
- thrombosis of the arteries of the brain with the clinical picture of ischemic stroke;
- obstruction of the jugular vein, which is characterized by severe headache, dizziness, palpitations and visual disturbances;
- clinic of acute myocardial infarction (MI) when an embolus enters the coronary arteries;
- renal artery thrombosis is accompanied by severe pain in the lumbar region and difficulty urinating;
- blockage of mesenteric vessels is manifested by peritonitis followed by intestinal necrosis;
- the presence of a blood clot in the arteries of the extremities is accompanied by paleness and blueness of the skin, the disappearance of pulsation in them, and in the absence of timely assistance, gangrene can form.
Each of these complications requires specially selected therapy, the main goal of which is to remove the detached clot and avoid the appearance of new ones. In addition, it is important to remember that detachment of a blood clot, regardless of its primary location, is the most common cause of heart attacks.
Diagnosis of blood clots
Unfortunately, due to the fact that the disease is practically asymptomatic and rapid, it is rarely diagnosed in time. If the patient has a tendency to increased blood clotting, the doctor may prescribe:
- coagulogram - biochemical analysis. This study determines the rate of formation of a blood clot;
- An echocardiogram is one of the ultrasound methods designed to study the heart. Helps identify functional or morphological changes;
- Dopplerography is another method of cardiac ultrasound. With the help of such a study, the condition of the cavities of the heart can be assessed as accurately as possible.
If a patient suspects thrombosis, the doctor will need to conduct a differential diagnosis with diseases that have similar clinical signs - pulmonary embolism or cardiac myxoma. For this purpose, a number of additional laboratory and instrumental studies are prescribed.
Pulmonary embolism
Symptoms of thrombosis of the left ventricle and apex of the heart
If the heart thrombus is motionless, then its manifestations may be absent. When large in size, it increases the signs of heart failure, disrupts the filling of the left ventricle with blood, and prevents full cardiac output. Patients develop and increase pallor of the skin with a bluish tint, difficulty breathing, the pulse quickens and weakens, and blood pressure drops.
When a clot breaks off or breaks into pieces, its fragments move into the arterial bed and lead to blockage of the vessels of the myocardium, brain, kidneys, intestines, and lower extremities . In such cases, the disease picture is determined by the localization of thromboembolism. Patients may develop a heart attack, stroke, or gangrene.
Manifestations of thrombosis as a complication of an existing heart attack cannot always be distinguished from the underlying disease, since the patient’s condition is initially severe. Indirect signs of the formation of wall thrombi are:
- protracted course;
- development of new foci;
- pronounced inflammatory reactions - increased ESR, specific enzymes and blood leukocytes, temperature with sudden changes;
- heart failure resistant to drug therapy;
- severe weakness;
- fainting conditions;
- night intense sweating.
Detection of endocarditis, aneurysm, and thromboembolic complications also indicate intracardiac thrombosis.
Treatment
Conservative therapy is ineffective. It can prevent the process of thrombosis, but it will not cope with already formed clots. A blood clot in the heart requires treatment, the essence of which is to remove the clots. The following surgical techniques are used for this:
- stenting – dilation of a vessel by installing a cylinder. Sometimes the clot can be removed with a syringe before this;
- bypass - creating an additional blood flow path that will bypass the affected artery;
- mechanical removal - physical removal of a blood clot from an artery. Practice shows that rehabilitation after such an operation is easy and in a shorter time. However, the disadvantage is the high cost of the procedure.
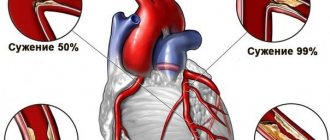
Typically, surgery is indicated in cases where the lumen of the vessel is 70% blocked by a clot. Prognosis depends on the general condition of the body, the size of the blood clot, and how much time has passed since the first symptoms appeared. Subsequently, patients are prescribed courses of anticoagulants, thrombolytics or antiplatelet agents to normalize blood viscosity. In addition, at the doctor's discretion, medications are prescribed that improve the outflow of fluid retained by tissues. A blood clot in the heart is extremely dangerous; if necessary, surgery is performed immediately.
Typically, surgery is indicated in cases where the lumen of the vessel is 70% blocked by a clot.
After the operation, the patient is given strict bed rest for some time. Sometimes it is necessary to wear elastic bandages or compression stockings.
Diagnosis of cardiac and aortic thrombosis
If intracardiac thrombosis is suspected, a comprehensive diagnosis is carried out. It includes:
- X-ray kymography - at the site of the blood clot, the amplitude of the teeth is low, and above and below it is increased;
- and MRI - detect double contours of the heart, an aneurysm of the heart wall or aorta, thrombosis of its cavity, signs of stratification of thrombotic masses; Blood and urine tests
- Ultrasound of the heart - determines the location, size and mobility of the blood clot;
- catheterization of cavities - detects a blood clot
- ventriculography – makes it possible to assess the residual volume of the heart chambers and their contractility;
- aortography – used to diagnose an aneurysm and thrombus formation in it;
- a coagulogram is not very informative for thrombosis of the cavities of the heart, since with the long-term existence of a thrombus it can show normal values, and in many myocardial diseases without thrombosis, elevated values are detected;
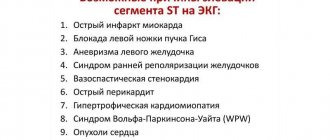
- ECG (if a blood clot occurred after a heart attack) – negative dynamics or no changes for a long period of time.
Contraindications to treatment, complications
Therapy with drugs that are usually used to normalize blood clotting has its side effects, like any other treatment. The most dangerous effect of such drugs is bleeding. They can aggravate the patient’s existing pathologies and also affect the general condition. Bleeding is life-threatening. Before prescribing a course of treatment, you should take into account all the characteristics of the patient and contraindications to the use of drugs.
Absolute contraindications are:
- the presence of diseases that may cause bleeding (for example, stomach ulcers). Treatment is acceptable if more than 10-14 days have passed since the bleeding;
- recent surgery or biopsy;
- damage to internal organs due to injury;
- risk of aortic dissection;
- thrombocytopenia (if the number of platelets is less than 100 thousand per 1 cm3);
- hemorrhagic diathesis;
- allergy to drug components;
- acute pancreatitis;
- pericarditis;
- blood pressure from 200 to 120 mm Hg. Art.
Bleeding poses a threat to life.
In any of these conditions, the use of drugs that affect blood clotting is unacceptable. It is necessary to cure the pathology before starting treatment, or choose an alternative. There are also relative contraindications, when the use of drugs that affect coagulation is acceptable if the situation requires it. These include:
- pregnancy;
- kidney and/or liver diseases;
- history of brain or spinal cord injury;
- fractures;
- burns;
- infective endocarditis;
- use of thrombolytics APSAC or streptokinase less than 4 months ago.
The inappropriate use of drugs to normalize blood clotting, in particular thrombolytics, is fraught with a number of complications. Among them, reperfusion arrhythmia can be identified as the most common. If this complication is detected in time, treatment is not difficult, however, if possible, such situations should be avoided.
Treatment of pathology
Intracardiac thrombi are virtually resistant to dissolution by standard anticoagulant therapy. It is used more often for the prevention of thromboembolic complications or treatment when they occur. Surgical removal is also performed extremely rarely - only when the patient’s life is threatened. If there is an aortic aneurysm and the formation of a blood clot that inhibits the movement of blood, its cavity is excised, and the defect is replaced with a prosthesis.
If a blood clot blocks the valve opening inside the heart and the patient stops contracting, then chest compressions and artificial ventilation are performed. In some cases, to move the blood clot and eliminate the blockage, it is enough to change the position of the body.
We recommend reading the article about post-traumatic thrombosis. From it you will learn about the causes and clinical picture of the development of an acute form of post-traumatic thrombosis, as well as methods for diagnosing and treating the veins of the lower extremities. Read more about deep vein thrombosis here.
Parietal thrombi form on the walls of the heart and aorta during heart defects, heart attack, aneurysm, arrhythmia against the background of increased blood coagulation activity. Their manifestations are nonspecific, and the clinical picture depends on the underlying disease, the size of blood clots and their mobility.
Large formations in the cavities of the heart disrupt local and systemic hemodynamics; when parts are torn off, thromboembolic complications occur. Thrombosis of the aortic aneurysmal sac disrupts tissue nutrition, leading to stroke, heart attack, and gangrene. Treatment is carried out when the patient’s life is at risk - the blood clot is removed surgically, medications are ineffective.
Prevention
To prevent such a complex pathology as a blood clot in the heart, it is not enough just to know the symptoms. Precautionary measures should be taken even without obvious signs of illness. Prevention is based on organizing proper nutrition and changing lifestyle. It is necessary to reduce or exclude salty, smoked, fatty, fried, and spicy foods from the diet. These products contribute to the deposition of cholesterol on the walls of blood vessels, which can cause atherosclerosis and subsequently thrombosis.
Prevention is based on proper nutrition and lifestyle changes
Among the foods that do not contribute to the deposition of cholesterol are:
- fish;
- tomatoes, their juice;
- chicken, rabbit, and other lean meats;
- some berries (blueberries, raspberries, blackberries);
- onion;
- garlic;
- beets;
- low-fat (up to 1%) dairy products;
- hard cheese;
- ginger root;
- sunflower seeds;
- olive and linseed oil;
- citrus;
- some cereals (buckwheat, wheat, oatmeal, rice).
The diet cannot completely guarantee safety, however, it significantly reduces the risk of developing pathology. To prevent blood clotting, it is recommended to drink plenty of water. If fluid is supplied in sufficient quantities, the body will not store it in the tissues.
It is recommended to walk more and spend a lot of time outdoors. This will saturate the blood with oxygen. Moderate physical activity will be beneficial.
Disease prevention
Since it is impossible to see the formation of a clot in your vessel in advance, doctors recommend undergoing regular medical examinations and following the following recommendations:
Lead an active life. You need to take care of yourself and follow all the rules of a healthy lifestyle from a young age in order to avoid a detached blood clot and death in the future. Eat a balanced diet. Every person's diet should contain only high-quality and natural products. Every day, meals should be filled with a vitamin complex and healing drinks that will help prevent pathological changes in the cardiovascular system.
Avoid stressful situations and strong worries. For detached blood clots, sometimes strong excitement and anxiety are enough. Vascular spasms and the release of additional adrenaline are a direct threat to human health. What you definitely need to give up is alcohol and smoking. Systematic physical activity. With regular and sufficient exercise, it is possible to train not only the muscular, but also the vascular system.
If the patient is diagnosed with intracardiac thrombosis, he also needs regular preventive measures.
These include:
Examination by a cardiologist at least once every 6 months. Prescribing Acetylsalicylic acid or Aspirin on a regular basis. Wearing courses of compression garments, which are used for varicose veins.
A blood clot in the heart is a serious condition that requires immediate medical attention. Only timely consultation with a doctor, correct diagnosis, and a developed treatment regimen will avoid the development of serious complications or death.
Compliance with the basic rules for the prevention of vascular thrombosis, playing sports, visiting a doctor or diagnostic laboratories at least once a year allows everyone to be healthy until the end of their days!
We recommend reading:
adminHome page » Blood clots
ratings, average:
out of 5)
Blood clot in the heart
Folk remedies for thrombosis
In most cases, specialists also prescribe folk remedies for symptoms of a blood clot in the heart. Death can occur if you do not take care of your health and start the disease. It is recommended to use herbal teas, decoctions and compresses. Some of them are presented below:
- Pour one hundred grams of horse chestnut with a liter of vodka and let it brew for two weeks. Take 20-25 drops several times a day for one month.
- Take 130 ml of hawthorn, motherwort, valerian and peony, add 45 ml of eucalyptus, 15 ml of Corvalol, echinacea and mint. Mix and add 10 finely chopped clove buds. Leave the solution to infuse for a week. Take several times a day for one month.
- Grind two lemons, add a head of garlic (chopped) and pour one glass of cold water. Let it brew in the refrigerator for several days. Strain and drink one tablespoon three times a day.
The above recipes should be discussed with your doctor if you have a blood clot in the heart. Symptoms may not appear immediately, but you need to start taking care of your health now.
Diagnostics
Primary diagnosis consists of an external examination of the patient to determine the nature of the complaints.
Suspicions of cardiac thrombosis are confirmed during a secondary examination using a coagulogram, which allows one to determine APTT, INR, D-dimers, PTI (prothrombin index) coefficient, etc.
Blood clots in blood vessels can also be detected using the instrumental method.
In particular, spectral Dopplerography makes it possible to determine not only the location of thrombotic clots, but also to determine their size, as well as analyze the state of blood flow in the vessels.
The venography method involves the introduction of an X-ray contrast agent into the vascular cavity with subsequent examination of the results obtained.
Additional methods include MRI, lung radiography, ultrasound of internal organs, etc.
Rehabilitation period
You can make an appointment with a doctor working in your city directly on our website.
To register, follow the link.
After thrombectomy, regardless of the treatment method, patients must follow a number of medical recommendations.
- Take blood thinners: anticoagulants, antiplatelet agents.
- To prevent the risk of inflammation, you should take non-steroidal anti-inflammatory drugs.
- If pain is present, the use of analgesics is allowed.
- You should wear compression garments for the first few months.
- It is necessary to exclude: any sports exercises and long walks, alcohol and tobacco products, cosmetic and hygiene procedures that involve heating the skin.
Causes
Blood flow through the coronary vessels can be disrupted under the influence of such factors:
- Atherosclerosis is one of the most common diseases of old age. Atherosclerosis leads to changes in the inner layer of blood vessels, due to which the tendency to form a blood clot increases significantly.
- Imbalance of the blood coagulation and anticoagulation systems.
- Vasospasm.
In half of patients with coronary thrombosis, changes occur against the background of unchanged vessels.
Predisposing factors:
- elderly age;
- overweight;
- smoking and drinking alcohol;
- hereditary predisposition;
- diseases of the endocrine system (diabetes mellitus, menopause), taking hormonal medications;
- arterial hypertension;
- eating foods rich in fats and carbohydrates.
Interestingly, coronary thrombosis also occurs in young people (under 35 years of age) who do not have all of the above predisposing factors.
Removing a blood clot with a laser
It is used, among other things, when diagnosing ascending thrombosis of the large or small vein of the thigh, when there is a risk of blockage of larger vessels.
How to remove a blood clot in the leg using the laser method?
The patient receives local anesthesia, then a catheter is inserted into the vein cavity above the area where the clot is located, through which laser beams are sent, gluing the venous lumen. With this treatment, only the affected areas of the vessel are closed.
Advantages
- Low invasiveness, no incision required. After local anesthesia, the venous wall is pierced with a special needle through which an LED passes. The ultrasound method allows you to monitor the action of the laser inside the vessel cavity.
- No pain. The patient feels only moderate pain from the anesthetic injection.
- Short rehabilitation period: sick leave lasts 4-5 days. As a rule, after the procedure, the patient can go home, subject to the use of recommended medications and compression stockings.
- Blood clots can be removed with a laser on both extremities at once, due to the low level of trauma.
- No visible scars on the skin. Immediately after the procedure, the marks are slightly noticeable, but after 2 months they disappear on their own.
- Low risk of relapse.
- The vessel is not removed. At the site of exposure to rays, they are glued together using connective tissue.
A blood clot has broken off - how to find out: can you feel and see a blood clot, is it possible to save a person?
Thrombus
Only a doctor can see the presence of a blood clot using ultrasound diagnostics. It is almost impossible to feel it, but you can only feel the consequences of its presence in the body. Also, when you press on the skin in the area where the blood clot is located, you will feel pain.
If a blood clot breaks off, how can you tell, can you feel it or see it? If an attached blood clot has come off, you can tell by the person’s condition. Depending on the location of the vessel, painful symptoms may be as follows:
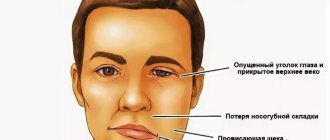
- In the brain , this will lead to a stroke. As a result, asymmetry of facial features, difficulty swallowing, and unclear speech.
- heart attack is possible in - pressing, sharp pain in the chest, or complete blockage of the heart vessels, which leads to death.
- In the intestines - a feeling of sharp pain in the abdomen and peritonitis.
- If a blood clot has blocked a vessel in the leg , swelling, blueness, redness, and severe pain are observed. In the absence of proper treatment - gangrene and amputation.
- Blockage in the lungs , also known as pulmonary embolism, is an acute condition that requires immediate hospitalization. It is characterized by a lack of oxygen, due to which the patient’s skin acquires a blue tint, shortness of breath is observed, and untimely assistance can lead to respiratory arrest and death.
Is it possible to save a person and how to provide first aid?
- An ambulance must be called immediately.
- In this case, painkillers and antispasmodics are important, but they should be taken only as directed by the emergency doctor.
- You also need to help the person find a comfortable position.
Often the correct actions of people around them help a person with an acute condition save a life.
Contraindications
Surgery to remove a blood clot on the leg is contraindicated under the following circumstances:
- The patient is in serious condition with concomitant illnesses.
- Exhausted state of the body.
- Blood sepsis.
- Personal intolerance to blood thinning drugs.
- Oncological diseases.
- Gangrene at the site of thrombosis.
- Thrombosis after radiation therapy.
- Difficult pregnancy.
- Postphlebitic syndrome.
Main causes of cardiac thrombosis
- Installation of a venous catheter. For patients undergoing long-term hospital treatment, a catheter is often installed in the subclavian vein.
Ideally, the diameter of the catheter should be smaller than the diameter of the vessel to maintain blood flow. However, if the diameters of the catheter and vein do not match, the outflow of venous blood from the upper limb is disrupted. As a result, blood stagnates in the vein and thickens.When the catheter is removed, blood circulation is normalized and the formed thrombus enters the right atrium through the superior vena cava.
Rheumatic carditis is one of the manifestations of rheumatism (a systemic disease of connective tissue), accompanied by damage to different layers of the heart muscle and valve apparatus.
When the heart muscle is damaged, myocytes are replaced by connective tissue (cardiosclerosis), which directly leads to rhythm disturbances.Damage to the valves is characterized by the formation of vegetations on their valves (overgrowth of connective tissue). Blood cells adhere to the vegetations and blood clots form.
- Valve prostheses lead to disruption of endocardial thromboresistance and the formation of turbulent blood flows through the prosthesis.
The synthetic valve triggers immune system activity, which causes platelets to “stick” to the valves. And disrupted blood flow only aggravates the situation and can lead to a blood clot. - An aneurysm is a separation of the heart wall with the formation of an intermuscular pocket in which blood collects and stagnates.
Subsequently, the blood in the aneurysm thickens and a blood clot forms. Excessive physical activity or nervous tension lead to increased heart rate and increased heart rate. As a result, the clot is pushed out of the aneurysmal pocket and enters the systemic circulation. - Atrial fibrillation is a disease accompanied by irregular heart rhythm. The atria contract incorrectly and do not push blood into the ventricles. As a result of congestion, clots form in the atrial appendages (the left atrial appendage is most often affected).
- Congenital and acquired heart defects. A large group of anomalies of cardiac structure.
These include valve stenosis, an abnormal number of valve leaflets (instead of three leaflets - 2 or 4), patent oval window (located in the wall between the right and left atria), additional chords in the ventricles (forming obstacles to blood flow), etc.Defects disrupt normal blood flow, which further damages the walls of the heart. Damaged areas release tissue plasminogen, which activates the blood coagulation system. As a result, there is impaired blood flow, damage to the walls and changes in blood composition.
Blood clots can be avoided only by promptly seeking medical help.
- Myocardial infarction is damage and shutdown of a section of the heart muscle.
As a result, the contractility of the ventricles decreases (most often the ventricles are susceptible to a heart attack), which leads to incomplete emptying of the cavities. Excess blood accumulates and stretches the injured walls of the ventricles. Such violations lead to the development of post-infarction aneurysms, arrhythmias and severe heart failure. What has already been written about above.
Risk groups for increased blood clot formation in the heart include:
- experienced smokers;
- patients with arterial hypertension;
- pregnant and postpartum women;
- obese patients;
- persons who frequently drink alcohol;
- people leading a sedentary lifestyle;
- patients after surgery on the pelvic organs, etc.
Symptoms and diagnosis
Making such a diagnosis is difficult. Most often, the patient has no complaints until a blood clot or fragment of it breaks off in the heart.
Unfortunately, the most common heart test - electrocardiography - will not help a specialist in identifying a blood clot.
People with frequent complaints relating to the heart need to regularly undergo ultrasound examination of the organ and Doppler ultrasound (vascular ultrasound). These two techniques will allow you to visually view the cavities of the heart and blood vessels and detect blood clots.
A carefully collected anamnesis is extremely important for diagnosis. It will help the doctor prescribe the right tests for the patient.
Diagnosis of intracardiac thrombosis is based on a thorough history of the clinical course of the disease. However, without an instrumental examination it is impossible to confirm the presence of a blood clot in the heart.
In this regard, the most informative are the following methods:
- Echocardiodopleographic examination (transesophageal ECHO-CG and transthoracic ECHO-CG).
- Transesophageal ECHO-CG, which has almost 100% diagnostic value.
Auxiliary techniques that suggest the presence of a blood clot in the heart are: scintigraphy, which allows you to determine the degree of filling of the myocardium with blood, Dopplerography, which measures the speed of blood flow and cardiac pressure.
It is also possible to conduct an MRI, which makes it possible to determine the presence of a heart tumor, the condition of its tissues, and the quality of its functioning. The earlier concomitant cardiovascular diseases are identified, the higher the likelihood that the patient’s life can be saved.
Your doctor will order an electrocardiogram (ECG), which will determine if you have a myocardial infarction. ECGs are not 100 percent accurate. If the pain remains constant, a second ECG can be taken only after half an hour. Once the patient is admitted to the hospital, a series of blood tests will be performed within the first 24 hours. They will check whether there was injury to the heart muscle and its extent.