What is pulmonary hypertension
Pulmonary hypertension (PH) is a group of diseases characterized by a pathological condition of the body's respiratory system caused by an increase in pressure in the pulmonary artery. The disease has a complex etiology and pathogenesis, which greatly complicates timely diagnosis and treatment.
The pulmonary artery is the largest and most important paired vessel of the pulmonary circulation, ensuring the transfer of venous blood to the lungs. The proper functioning of the respiratory system depends on its condition.
Normally, the average pressure in the pulmonary artery should be no more than 25 mm Hg. Art. Under the influence of various factors (physical activity, age, taking certain medications), these values may vary slightly, both up and down. This physiological increase or decrease does not pose a threat to health. But if the average pressure exceeds 25 mm Hg. column at rest, this is a sign of pulmonary hypertension.
The disease mainly affects women. Pulmonary hypertension is also diagnosed in children, due to the presence of heart defects.
The disease is rare. Its idiopathic form is registered in 5 - 6 cases per 1 million population.
Description of the disease, its causes
Pulmonary artery hypertension develops against the background of other diseases, which may have completely different causes. Hypertension develops due to the proliferation of the inner layer of the pulmonary vessels. In this case, their lumen narrows and disruptions in the blood supply to the lungs occur.
This disease is quite rare, but, sadly, most cases are fatal.
The main diseases that lead to the development of this pathology include:
- Chronical bronchitis;
- fibrosis of lung tissue;
- congenital heart defects;
- bronchiectasis;
- hypertension, cardiomyopathy, tachycardia, ischemia;
- thrombosis of blood vessels in the lungs;
- alveolar hypoxia;
- increased red blood cell count;
- vascular spasms.
There are also a number of factors that contribute to the occurrence of pulmonary hypertension:
- thyroid diseases;
- intoxication of the body with toxic substances;
- long-term use of antidepressants or appetite suppressants;
- use of drugs taken intranasally (inhaled through the nose);
- HIV infections;
- oncological diseases of the circulatory system;
- cirrhosis of the liver;
- genetic predisposition.
Pulmonary hypertension can form as a result of prolonged compression of the blood vessels of the lungs. This condition can occur with chest injuries, excess weight and tumors.
ICD-10 code
Pulmonary hypertension is in ICD-10 in the group with code I27, which denotes forms of pulmonary heart failure not listed in other classes.
Primary pulmonary hypertension is encrypted I27.0 and is characterized by the occurrence of a disease without a clear etiology.
Various forms of secondary pulmonary hypertension that occur as a consequence of other diseases are designated by code I27.2.
Classification of pathology
In medical practice, the following types of pulmonary hypertension are distinguished:
- Primary pulmonary hypertension . It is rare and is caused by a hereditary factor associated with mutations at the gene level. A separate idiopathic form of primary pulmonary hypertension is distinguished, the causes of which cannot be determined.
- Secondary pulmonary hypertension . This form of the disease develops against the background of another pathology or under the influence of negative external causes. Often the disease develops due to congenital heart defects, connective tissue diseases, infectious (HIV), parasitic (schistosomiasis) and systemic pathologies (for example, hemolytic anemia). Pulmonary hypertension can also develop when taking medications (antibiotics). There is evidence linking the occurrence of pathology with contact with aggressive chemical compounds, in particular asbestos.
- Thromboembolic pulmonary hypertension . The cause of its occurrence is a blood clot, which, as it moves through the bloodstream, clogs the lumen of the pulmonary artery. This form of the disease has a rapid course with the development of acute respiratory failure and orthostatic collapse.
- Mixed pulmonary hypertension . The occurrence of this form of the disease is associated with a history of other diseases (renal failure, oncological pathologies, vasculitis, etc.). The causal relationship between them and the level of pressure in the pulmonary artery is not fully determined.
Mechanisms of disease development
How does mild pulmonary hypertension develop? The reasons lie in dysfunctions or structures of the endothelium that lines the pulmonary vessels:
- Endothelial dysfunction, which may be associated with both genetic predisposition and exposure to external factors. The processes of nitric oxide metabolism are disrupted, the tone of the vascular wall changes (spasm develops), resulting in an inflammatory process with further growth of the endothelium.
- Increased endothelin content. This substance has vasoconstrictor properties. The disease in this case may be associated with both increased production of this substance in the endothelium and a decrease in the rate of its decay in the lungs.
- In some cases, endothelial proliferation is associated with additional excretion of potassium ions, as well as impaired nitric oxide synthesis and a decrease in prostacyclin levels.
Causes and risk factors
The reasons for the development of primary pulmonary hypertension are not known for certain. There is a theory that its occurrence can be correlated with genetic as well as autoimmune processes.
There have also been cases where pulmonary hypertension occurred in members of the same family in the presence of heart defects in the descending line, which indicates a significant role of the hereditary factor.
The pathogenesis of the disease is due to the gradual narrowing of the lumen in the pulmonary artery, as well as the vessels of the lungs and the pulmonary circulation in general. This is not due to atherosclerotic changes, which is typical for patients suffering from arterial hypertension, but to pathological thickening of the walls of veins and capillaries, which leads to their loss of elasticity.
The consequence of these processes is an increase in blood pressure in the pulmonary artery and vascular network of the lungs. As a result of this pathology, phenomena of general hypoxia and tissue nutritional deficiency are observed.
In severe cases of pulmonary hypertension, inflammatory processes may occur that involve the inner lining layer of blood vessels - the endothelium. This factor increases the risk of pulmonary artery thrombosis and other complications.
Therapeutic methods
Propaedeutics of PH is currently not extensive enough; the causes of the disease continue to be identified. Based on the determination of the type of hypertension (causes), the group and dosage of medications used is based. The action of the drugs is aimed at the following results:
- dilation of blood vessels;
- decreased blood clotting;
- reducing the amount of fluid in the body due to increased urination;
- improving blood oxygenation.
The most effective therapeutic method is long-term oxygen inhalation (14–15 hours/day).
Treatment of primary hypertension is very complex. Some compounds are used that lead to dilation of the pulmonary vessels, therefore reducing the pressure in the pulmonary vascular bed. One of these compounds, Sildenafil, is a 1st-line drug for pulmonary hypertension.
Important! The drug "Sildenafil" has shown a strong effect on the blood vessels in the penis, which is why its instructions for use indicate a positive effect on potency. Medicines containing Sildenafil have become popular drugs for erectile support (for example, Viagra).
Heart failure, usually present in PH, is treated symptomatically. The final solution in certain situations is lung transplantation.
In the secondary form of the disease, treatment of the underlying disease is necessary. If therapy is successful, hypertension is alleviated.
High doses of calcium channel blockers (Nifedipine, Diltiazem, Amlodipine) and nitrates are recommended only if vasoreactivity persists.
Symptoms of pathology, classes of disease
Pulmonary arterial hypertension, with the exception of its thromboembolic form, has a slow development. Clinical symptoms increase gradually and are mild. Their complete absence is also possible.
The leading symptom of pulmonary hypertension is shortness of breath, which is initially present only during intense physical activity, but as the pathological process progresses, it begins to occur at rest. In the last stages of the disease, the severity of shortness of breath is so severe that the patient is unable to perform basic everyday activities on his own.
A characteristic difference between shortness of breath in pulmonary hypertension and a similar symptom in heart failure associated with the formation of heart defects is that it does not go away when the patient’s body position changes.
In addition to shortness of breath, characteristic signs of the disease are:
- dry cough;
- liver enlargement and pain;
- swelling of the lower extremities;
- chest pain;
- increased fatigue and constant weakness;
- hoarseness of voice (not observed in all patients).
Pulmonary hypertension is a disease characterized by a gradual increase in pathological symptoms that impair the functioning of the heart. Depending on its severity, it is customary to distinguish 4 classes (stages) of the disease.
- I class . Stage 1 hypertension is the initial form of the disease. The patient does not feel any pathological changes. Physical activity is easily tolerated and motor activity is not affected.
- II class . At stage 2, physical activity is tolerated as usual, but at high intensity the patient notices the appearance of severe shortness of breath and increased fatigue. The severity of morphological changes in blood vessels and internal organs is insignificant.
- III class . At stage 3, habitual physical activity is poorly tolerated. Moderate activity is accompanied by most of the symptoms listed above. The ECG shows hypertrophy of the right ventricle of the heart.
- IV class . The manifestation of characteristic symptoms is observed in the absence of stress. There is an inability to perform daily tasks. The patient needs constant care. At stage 4, symptoms of heart failure appear.
Complications of pulmonary hypertension
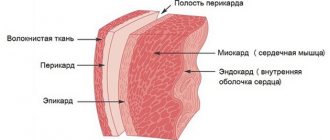
Pulmonary hypertension, associated with increased pressure in the pulmonary artery, is accompanied by serious complications from the cardiovascular system. During the development of pathological processes associated with pulmonary arterial hypertension, hypertrophy of the right ventricle of the heart muscle occurs. This occurs due to the increased load on this chamber, as a result of which its contractility deteriorates, which leads to the development of heart failure.
Hypertension of the 1st degree is characterized by the fact that patients may experience disturbances in the functioning of the heart, expressed in cardiac tachycardia and atrial fibrillation.
As the vascular walls change, blood clots - thrombi - form in the veins. They narrow the lumen of blood vessels, which leads to increased severity of symptoms. A detached blood clot can block blood flow, which leads to pulmonary embolism, which, in the absence of timely medical care, ends in the death of the patient.
If there is a history of arterial hypertension, pulmonary hypertension increases the frequency and severity of crises, which are fraught with the development of a heart attack or stroke.
A serious complication of the disease is death, which occurs either as a result of respiratory failure or as a consequence of disturbances in the functioning of the heart.
How does the disease manifest itself?
Moderate pulmonary hypertension develops slowly; at the initial stage, the symptoms of the disease are not pronounced. The main clinical sign of the disease is cor pulmonale. The pathology is characterized by hypertrophic changes in the right parts of the heart.
What signs should you see a doctor for:
- The main manifestation of the disease is shortness of breath, which worsens even with minor physical exertion.
- Cardiopalmus. The cause of tachycardia is respiratory failure, lack of oxygen in the blood.
- Pain syndrome. Compressive pain occurs behind the sternum and in the region of the heart. With strong physical exertion, fainting is possible.
- Dizziness, weakness, fatigue.
- Accumulation of fluid in the peritoneum (ascites), severe swelling and blueness of the limbs, bulging veins in the neck. These symptoms develop against the background of chronic right ventricular failure - the heart muscle of the right ventricle cannot cope with the load, which leads to disturbances in the systemic circulation.
- An enlarged liver leads to heaviness and pain under the right ribs.
- Nausea, flatulence, vomiting are caused by accumulation of gases in the intestines. Weight loss with normal, nutritious nutrition.
The fingers thicken in the upper phalanges, the nails become like watch glass. As the pathology develops, sputum mixed with blood appears, which signals the onset of pulmonary edema. The patient suffers from attacks of angina pectoris and arrhythmia. At the terminal stage of the disease, active tissue begins to die.
Important! Pulmonary hypertension is a hereditary disease caused by a genomic defect.
Diagnostics
Diagnosis of pulmonary hypertension begins with a history. The nature and duration of symptoms, the presence of chronic diseases, the lifestyle of patients and associated risk factors are clarified.
Upon direct examination, the following characteristic signs are revealed:
- cyanosis of the skin;
- liver enlargement;
- swelling of the neck veins;
- changes in the heart and lungs when listening to them using a phonendoscope.
The leading role in the diagnosis of pulmonary hypertension belongs to instrumental methods.
Pulmonary artery catheterization. This method measures the pressure in the pulmonary artery. The essence of the study is that after puncture of the vein, a catheter is inserted into its lumen, to which a device for measuring blood pressure is connected. The method is informative in identifying any forms of hemodynamic disorders. And it is included in the standard of research for suspected pulmonary hypertension. Catheterization is not indicated for all patients; in the presence of heart failure or tachyarrhythmia, the possibility of its implementation is assessed after consultation with a cardiologist.
General recommendations
Patients with a similar diagnosis are advised to follow some rules. For example, in the presence of systemic diseases (lupus, scleroderma), it is important to carry out prevention in order to prevent the development of another exacerbation.
A necessary aspect of treatment is proper nutrition and physical activity (the degree of physical activity is determined individually, as it depends on the condition and age of the patient).
Women with pulmonary hypertension are advised to protect themselves from pregnancy. The fact is that the growth and development of the fetus means additional stress on the heart. In some cases, doctors even recommend terminating a pregnancy that has already begun.
Treatment methods for pulmonary hypertension
Treatment of patients with pulmonary arterial hypertension consists of eliminating symptoms and stopping the development of pathological processes. Various therapy methods are used for these purposes.
General recommendations
The presence of pulmonary hypertension requires adjustments to the lifestyle of patients. Such measures should include:
- performing daily physical therapy exercises that help improve the tone of blood vessels, but do not require increased respiratory activity;
- avoiding excessive physical activity;
- prevention of infectious and inflammatory diseases of the respiratory system (bronchitis, pneumonia), and if they occur, timely treatment;
- prevention of anemia, which consists of taking special medications (Sorbifer);
- refusal of hormonal methods of contraception;
- quitting smoking and excessive consumption of alcoholic beverages.
Drug therapy
- Vasodilators (for example: Nifedipine, Cardilopin ). Widely used in the treatment of PH. They reduce the tone of the vascular walls, promoting their relaxation and reducing the overall pressure in the veins and arteries. As a result, the diameter of the vessels increases and blood flow improves.
- Prostaglandins (for example: Treprostinil ). Medicines that help relieve vascular spasm. Taking prostaglandins helps prevent blood clots. Effective for all types of PH.
- Cardiac glycosides ( Digoxin, Strophanthin, Korglykon ). When taken, vascular spasm decreases, blood flow to the heart muscle increases, and the vascular system's tolerance to external unfavorable factors increases. In pulmonary hypertension, they are used to prevent and treat heart damage.
- Anticoagulants ( Aspirin, Eliquis ). They prevent the development of thrombosis and also dissolve existing blood clots.
- Diuretics ( Furosemide ). Diuretics ensure the drainage of excess fluid from the body, which reduces the volume of circulating blood. This minimizes the load on the cardiovascular system and helps reduce pressure in the systemic and pulmonary circulation.
- Endothelin receptor antagonists ( Bosentan, Tracleer ). The pathological process in blood vessels in patients with pulmonary arterial hypertension is caused by the proliferation of the internal lining surface of blood vessels - the endothelium. Taking medications from this group significantly slows down the development of the disease.
Features of the course of PH in children
Increased pressure in the lungs in childhood, in most cases, is observed against the background of congenital anomalies of the cardiovascular system and respiratory tract diseases. As a rule, the causes of pathology are defects in the development of blood vessels and the heart. Anatomical and functional disorders lead to the discharge of blood through structural defects into the right side of the heart, which provokes the formation of secondary PH. The period up to one year becomes critical, since only half of children survive without surgery. The condition may stabilize for a short time, but symptoms of circulatory failure gradually begin to increase.
The cause of the disease in infants can be hypoplasia of the lungs due to the ingress of amniotic fluid or intestinal contents into the respiratory tract at the time of birth. In children, the number of alveoli and bronchial branches decreases, and the structure of the arteries remains in its original form, as in a newborn (small vascular lumen and thick muscle wall).
The main manifestations of the disease in a child are diagnosed during the period of irreversible changes. Viral diseases, influenza, and pneumonia become the trigger mechanism for the occurrence of pathology.
Prevention
There are no specific prevention methods.
General preventive measures are aimed at eliminating risk factors and improving the health of the body:
- timely treatment of infectious diseases;
- eliminating the effects of heavy physical activity on the body;
- moderate physical activity;
- elimination of bad habits (alcohol, smoking);
- taking medications to prevent blood clots;
- treatment of heart defects.
If pulmonary hypertension has already been diagnosed, then prevention is aimed at reducing the likelihood of developing possible complications. In case of primary pulmonary hypertension, it is necessary to take all medications prescribed by the doctor and follow his recommendations in full. Moderate physical activity helps maintain an active lifestyle.
Forecast for life
How long can you live with this disease? The prognosis depends on the neglect of pathological processes in the vessels. When PH is diagnosed in late stages, the five-year survival rate of patients is low.
The prognosis of the outcome of the disease is also influenced by the body’s reaction to the treatment. If the pressure in the pulmonary artery begins to decrease or remains at the same level, then with maintenance therapy the patient can live up to 10 years. When it increases to 50 mm Hg. Art and above, the disease enters the stage of decompensation, when normal functioning of the body is impossible even under conditions of adequate drug therapy.
The five-year survival rate at this stage of the disease is no more than 10%.
Pulmonary arterial hypertension is a dangerous disease with a very serious prognosis for life. Despite the fact that it is quite rare, being, in most cases, a consequence of other diseases, a complete cure is impossible. Existing treatment methods are aimed at eliminating unfavorable symptoms and slowing down the development of pathological processes; they cannot be completely eliminated.