In the scientific literature and medical practice, changes in the intensity of the heart's work are collectively called arrhythmia. We are talking about either an uneven distribution of time between impacts, or correct, but not intense enough or too strong activity. The first option is called bradycardia, the second - tachycardia.
A decrease in heart rate is no less dangerous than other types of disorders. In general, a signal of the onset of problems is a decrease in the number of heart contractions to 60 beats per minute or less (60 is the lower limit).
The muscular organ does not pump enough blood and is not able to provide the tissues with nutrients and oxygen, which the liquid connective substance is rich in. Hence hypoxia with all the ensuing consequences: up to stroke, heart attack or cardiac arrest.
Sinus bradycardia is a decrease in heart rate to 60 beats or less, due to disruption of the heart node of the same name, a kind of regulator of the cardiac impulse.
The mechanism of pathology development
The process under consideration is formed according to textbook rules. We need to start with a brief anatomical background.
The heart usually works without external stimuli, autonomously. This explains why a brain-dead person still continues to “live,” or better yet, exist vegetatively.
The rhythm can be adjusted by the brain stem or other external stimuli, but this does not have a significant effect.
The main structure responsible for generating an electrical impulse and muscle contraction is the so-called sinus node or pacemaker, as it is also called.
This is a collection of heart cells. However, this formation alone is not enough for the complete conduction of the impulse. The sinoatrial and atioventricular nodes serve the same purpose (further along the bundle of His to other tissues). That is, in the optimal position, the speed of cardiac activity is regulated by the driver.
Sinus rhythm is the normal physiological activity of the heart.
In case of disturbances from the nodes, two types of bradycardia are formed: sinus bradycardia itself (which will be discussed) and non-sinus bradycardia (located in other nodes or associated with impaired conduction of the His bundle). Mixed types are possible, and most often they are found.
The essence and danger of sinus bradycardia
A healthy heart contracts on its own without any stimulating influences. This is possible thanks to spontaneous excitatory impulses that arise in the cardiac nerve cells. The largest cluster of them is called the sinus node. Its impulses are rhythmic, strong and pass through all parts of the heart, producing regular, uniform contractions of the myocardium. Therefore, a healthy heart rhythm is called sinus (its frequency per minute is 60–90 beats).
With sinus bradycardia, the sinus node generates few impulses, the heart contracts less frequently than it should - less than 60 times per minute. This leads to a slowdown in blood circulation in all organs and tissues, which is accompanied by oxygen starvation (hypoxia). The brain and heart muscle suffer the most. The more pronounced the bradycardia, the more severe the disturbances in the body. A threat to life occurs when the heart rate slows down to less than 40 beats per minute, and numbers less than 30 beats per minute are a signal of impending cardiac arrest.
Reasons for the development of the process
They are always divided into pathogenic and physiological.
Natural factors
In such a situation, bradycardia is a variant of the norm and does not reach values less than 50 beats per minute (mild disturbance of heart rate). No treatment is required either.
- General body fitness. During physical activity, a muscular organ shows less intensity of functioning due to familiarity and adaptability. Tachycardia almost never occurs in professional and amateur athletes. But in a calm state, the heart rarely accelerates to 80-90 beats or more; bradycardia is typical. For comparison, if the average person takes the same load, it will all end in a heart attack or cardiogenic shock. Advice for lovers of active recreation: increase the load evenly, gradually, do not force it.
- Staying in one position for a long time. An example is bedridden patients. If physical activity is minimal for 18-24 hours, it will result in a gradual but steady decrease in heart rate. After the stationary period, everything returns to normal.
- Dream. Night rest is associated with a slowdown in physiological processes: body temperature and blood pressure decrease, and less specific hormones are produced that are responsible for partial regulation of heart rate. In addition, the hypothalamus and brainstem provide fewer signals to excite the sinus node. This is the so-called circadian rhythm. If a person violates the natural regime for a long time, the biological clock gets lost, and it is much more difficult to restore the normal situation.
- Changes in climatic conditions. When moving from warm to cold. Hypothermia is associated with temporary processes of inhibition of all body functions. Adaptation lasts no more than 3-7 days. If more, there is reason to suspect a pathological process.
- Insufficient consumption of table salt. For normal conduction of cardiac structures, a sodium compound is required. Complete refusal is unacceptable.
- Puberty, peak hormonal conditions. In addition to puberty, we are talking about pregnancy. During gestation, a decrease in blood pressure and cardiac activity is observed. Another option is the beginning of the menstrual cycle. Women react to it differently, but, as a rule, they are aware of their problems.
- Age over 55-60 years. In older years, bradycardia occurs as a result of weakening of the heart muscle. The same processes are observed with constant load on the myocardium as a result of hypertension.
Physiological causes of sinus bradycardia include environmental conditions, circadian rhythm, peak hormonal conditions, etc. Natural factors account for up to 30% of all cases. The remaining clinical situations are of pathological origin.
The main features of physiological bradycardia:
- No obvious symptoms.
- Uniform heart rate.
- Low severity of decrease in heart rate (not lower than 50).
Pathological causes
Numerous (the pathological genesis of bradycardia accounts for up to 70% of all recorded clinical situations) and, accordingly, dangerous.
Possible diseases include:
- Poisoning with heavy metals: mercury, cadmium, as well as other substances: arsenic, phosphine. Medicines: tincture of lily of the valley, overdosing with cardiac glycosides, antihypertensive drugs, beta blockers, calcium channel blockers, ACE inhibitors, diuretics. Sinus bradycardia is most typical for chronic hypertensive patients and heart patients.
- Renal failure, pathologies of the excretory system. Accompanied by lower back pain, frequent unsuccessful visits to the toilet, and an increase in daily diuresis. It is caused by a decrease in hemodynamics, a deficiency of renin (a special prehormone responsible for the regulation of vascular tone).
- Liver failure. As a result of hepatitis or, more often, cirrhosis. The reason is again hormonal: the lack of production of angiotensinogen, the metabolites of which, along with renin, stabilize the heart rhythm. Symptoms: pain in the right hypochondrium, nausea, vomiting, yellowness of the skin, discoloration of feces.
- Hypothalamic syndrome (mistakenly called vegetative-vascular dystonia). Less often we talk about somatotrophic dysfunction. There is no diagnosis of VSD, it is just a symptom of many possible syndromes. Accompanied by dizziness, nausea, cephalgia, and less often vomiting. Causes disruption of the processes of excitation and inhibition in the central nervous system.
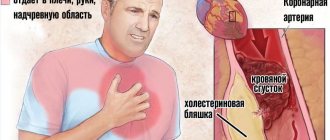
- Problems with the heart itself: coronary heart disease, previous heart attack, angina pectoris, sick sinus syndrome). Accompanied by chest pain, irregular rhythm, breathing problems, fatigue, and low performance.
- History of malignant and benign tumors. The first - any localization. The second ones are located in the heart area.
- Infectious diseases with acute intoxication: pneumonia, tonsillitis, peritonitis, sepsis.
- Hormonal imbalances as a result of damage to the endocrine system: hypothyroidism, hypocortisolism and diabetes mellitus. Symptoms are varied: weakness, weight loss, sharp decrease in blood pressure and temperature.
There are also subjective factors: smoking, alcoholism, long-term addiction to psychoactive substances.
Bradycardia during pregnancy
In women during pregnancy, bradycardia develops extremely rarely, if it did not exist before pregnancy. Bradycardia can be physiological or pathological. Physiological bradycardia is a variant of the norm and is usually noted if, before pregnancy, a woman led an active lifestyle, trained, physically worked, etc. In this case, bradycardia does not pose any danger to the fetus or to the woman herself.
Pathological bradycardia during pregnancy is usually provoked by the following pathologies:
- Thyroid diseases;
- Kidney and liver diseases;
- Diseases of the heart and blood vessels;
- Dysregulation from the central nervous system.
In the presence of pathological bradycardia, a pregnant woman should receive treatment, the purpose of which is to eliminate the diseases that caused the decrease in heartbeat. Pathological bradycardia can be dangerous for the mother and fetus.
Symptoms
Signs depend on the form of the process.
Weak and moderate
Heart rate is from 60 to 40 beats per minute.
- Headache.
- Vertigo.
- Dyspnea.
- Sweating. Especially at night.
- Sleep disorders.
- Discomfort behind the sternum. Pressing, pulling, radiating to the shoulder blade and arms.
All manifestations are mild and may be absent altogether if the process lasts a long time. The body gradually adapts to new conditions.
Expressed form
Heart rate - less than 40 beats. Symptoms are most pronounced:
- Headache.
- Vertigo up to complete lack of orientation in space.
- Shortness of breath, suffocation.
- Intense discomfort in the chest.
- Weakness, drowsiness.
All this against the background of impaired consciousness up to coma, decreased blood pressure and the inability to independently determine the pulse. The general condition is serious; urgent hospitalization in a hospital and resuscitation are required.
Acute form
Fully corresponds to a moderate or severe type of pathological process. Symptoms are sufficiently defined to identify the problem, but not sufficiently to require resuscitation.
May continue indefinitely. Gradually passes into the chronic phase. Then the intensity of the manifestations drops to a minimum, the patient adapts to new conditions, which is not good: if there is a pathology, it does not go away, it progresses, but does not let anyone know about the existence of a problem.
Fetal bradycardia
Currently, the CTG (cardiotocography) method allows you to record the fetal heart rate during pregnancy. The lower limit of normal fetal heart rate is 110 beats per minute. If the fetal heart rate is less than 110 beats per minute, then we are talking about bradycardia. Typically, bradycardia indicates intrauterine hypoxia, cerebrovascular accidents, or some other pathology of the fetus. It is impossible to determine from bradycardia alone what kind of developmental disorders the fetus has, since additional detailed examination is necessary using ultrasound, Doppler, possibly genetic analysis, etc. Therefore, fetal bradycardia is a signal for subsequent examination, the purpose of which is to identify any abnormalities present in the fetus.
Currently, many pregnant women are concerned about fetal bradycardia in early pregnancy and ask many questions about this. However, you should know that the information value of measuring heart rate to assess the condition of the fetus occurs no earlier than 20–22 weeks of pregnancy. It is from this time that it makes sense to do CTG and calculate the fetal heart rate. Any measurement of the fetal heart rate earlier than 20–22 weeks of pregnancy is not informative. Until the 20th week of pregnancy, the only information that can be obtained about the fetal heartbeat is whether it is present or not. That is, to record whether the child is alive or dead. If there is a heartbeat, then the child is alive; if it is not heard, it means that the fetus died in utero. Its heart rate does not provide any information about the condition of the fetus until the 20th week of pregnancy. This means that women do not have to worry about fetal bradycardia at 5, 6, 7, 8 ... 19 weeks of pregnancy, since this does not mean anything other than stating the fact that the baby is alive, growing and developing.
Can you help yourself at home?
With mild and moderate bradycardia - quite. Both classical medicines and folk recipes will help normalize the condition.
The algorithm is as follows:
- Measure your blood pressure and heart rate. This is necessary for subsequent assessment of the effectiveness of first aid.
- Take a tablet or two of a tonic: Citramon, preferably pure caffeine, as well as Aspirin-Cardio (if it is not available, simple acetylsalicylic acid, but the dosage is less). Zelenin drops help well, but they must be used with caution, the drug significantly increases heart rate. Start with 20 drops.
- Drink tincture of eleutherococcus, ginseng or eat a couple of spoons of lemon with cinnamon and honey.
- Take a horizontal position and move as little as possible. Physical activity can lead to fatal complications.
If there is no effect, call an ambulance within 20-30 minutes.
The following activities are shown on site:
- Introduction of Dopamine.
- Atropine injection.
- As a last resort, adrenaline is used.
Then the issue of transporting the patient to a cardiology hospital for comprehensive diagnostics and treatment is decided.
Moderate sinus bradycardia allows for primary self-care. If there is no effect, an emergency call is indicated. Complications - heart attack, stroke, cardiac arrest, cardiogenic shock, death.
Are they allowed into the army with this diagnosis?
The decision whether to accept a conscript for military service if he has cardiac bradycardia is influenced by three factors:
- reasons for the formation of pathology;
- possible consequences of the disease;
- what type of bradycardia was detected in the young man.
If the slow heart rate is associated with a malfunction in the body, then the military commission can issue the conscript a deferment from the army . But before that he needs to undergo examination. A young man's fitness category for service is determined using four functional classes.
| Function class | Conscript status | Doctor's report |
| First | There is no discomfort and fatigue during physical activity. | Fit for service. Category “B” is assigned. |
| Second | Shortness of breath and fatigue appear when performing habitual exercises. | Limited fit for service. Category “B” is assigned. |
| Third | Severe fatigue is observed even when performing light loads. | Not fit for military service. Category “D” is assigned. |
| Fourth | Weakness occurs even in a state of complete rest. | Not fit for military service. Category “D” is assigned. |
If concomitant diseases with bradycardia have not been identified, then the young man can serve in the army. A moderate state of pathology does not require lifestyle adjustments and does not affect the activity of the conscript.
Now you know what the concept of sinus bradycardia means and what it looks like on an ECG, why it is dangerous for the heart of children and adults, in old age, and whether you are drafted into the army with this disease and whether treatment is always necessary. Bradycardia can be characterized both as a harmless phenomenon and as a serious disease that is life-threatening. Therefore, you cannot ignore it: you need to consult a doctor in time to take action as soon as possible.
Necessary examinations
Cardiologists are involved in the management of patients with a pathological process. Specialists of other profiles are involved if there is a suspicion of a non-cardiac etiology of the disease.
Diagnostic scheme:
- Interviewing the patient and collecting anamnesis. First of all. This moment cannot be underestimated. The vector of further activities is determined. The patient’s task is to tell about all his complaints.
- Measurement of blood pressure, heart rate.
- Determination of the functional activity of a muscle organ using an ECG.
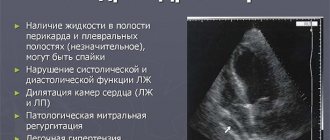
- Echocardiography. Visual technique for assessing the condition of heart structures.
- Angiography.
- MRI.
Activities of a different profile: blood tests, urine tests, examination of neurological status, scintigraphy of the adrenal glands, liver, thyroid gland.
Systematicity is a guarantee of quick diagnosis and verification. If necessary, the list is expanded. For moderate and severe bradycardia, inpatient examination is recommended. There is always a danger of complications.
Tests and diagnostics
For diagnostic purposes, patients with a rare pulse undergo a special examination:
- listening to heart sounds using a phonendoscope and stethoscope;
- ECG film analysis at rest and after exercise;
- carrying out bicycle ergometry ;
- conducting daily Holter ECG monitoring ;
- conducting echocardiography ;
- analysis of biochemical parameters of urine and blood;
- analysis for toxins if poisoning or intoxication of the body is suspected;
- transesophageal electrophysiological study of the cardiac conduction system (used only if the ECG fails to detect certain changes or blockages);
- carrying out bacteriological analysis of urine and blood if infection is suspected.
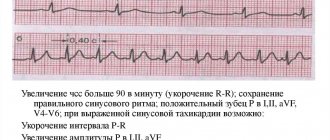
Specific signs of a problem on the ECG
It won't say much to the average patient. To tell you a secret, not every doctor understands the issue; deep knowledge is required.
Among the characteristic features:
- Increasing the RR interval (0.21-0.22 sec), TP.
- Increase int. QT.
- Teeth: T1,T2 - +. T3 - low, also positive, TV1 - negative.
All changes are relatively mild; it is impossible to diagnose the factor in the development of the disease using electrocardiography alone. It’s quite enough to state a fact.
Sinus node dysfunction
The cause of dysfunction of the sinus node can be either direct damage to its structure (ischemia, myocardial infarction, hemochromatosis, rheumatoid arthritis), or indirect through the influence of drugs, water-electrolyte imbalance, in hypothyroidism, hypoglycemia, hypoxia (obstructive apnea syndrome), increased intracranial pressure.
Most often, damage to the sinus node occurs as a result of the development of atherosclerosis and, as a consequence, coronary heart disease . Chronic ischemia develops, with possible death of sinus node cells. In addition, with ulceration of atherosclerotic plaques and thrombosis of the arteries supplying the sinus node (right coronary artery or left coronary artery), myocardial infarction and damage to the structures of the main pacemaker develop.
During myocardial infarction, the development of sinus bradycardia is most often observed at its lower localization.
Treatment methods
Surgical, medicinal and folk. Often in combination.
Drugs
Toning. Among the groups:
- Cardiac glycosides. Normalize the functional activity of the organ. They have a cardiotonic effect. Lily of the valley tincture, other medicines.
- Citramon, Aspirin-Cardio, Caffeine, Zelenina (with caution). Helps speed up the rhythm.
- Sedatives of plant origin. Motherwort and valerian.
It is better to stay away from beta and alpha blockers, ACE inhibitors and calcium channel blockers, as well as tranquilizers. They have exactly the opposite effect. If hypertension occurs, a strictly adjusted dosage is selected.
Surgical methods
The main method is the installation of an artificial pacemaker (pacemaker). Severe sinus bradycardia is treated surgically in 80% of cases. Urgent care is indicated after the patient has been brought out of critical condition.
Traditional methods
- Eleutherococcus tincture (2-3 spoons 3 times a day).
- Alcohol preparation of ginseng (30 drops 1-2 times a day).
- Lemon with cinnamon and honey (3 l. 2 r.d.).
- Decoction of nettle, chamomile (1:1, 300 ml of water per 100 grams of raw materials).
- Hawthorn (15-20 drops).
Lifestyle changes also make a difference. Among the methods:
- Quitting smoking and alcohol.
- Normalization of physical activity (several hours of absenteeism per day, exercise therapy).
- Drinking regimen - 2 liters.
- Salt - 12 grams.
- Rations - treatment tables No. 3, No. 10.
Can:
- Fruits, vegetables (especially apples, bananas, pears, kiwis, potatoes).
- Kissels, berry decoctions and others.
- Porridge.
- Dietary meat, protein, soups based on these varieties.
- Fermented milk products.
- Butter.
- Eggs.
- Honey, dried fruits.
- Coffee.
- Tea.
- Chocolate.
It is forbidden:
- Fast food.
- Fat meat.
- Baked goods, fried pies.
- Canned food, semi-finished products.
Cooking method: boiling, steaming and baking. Small meals, overeating and eating at night are unacceptable.
Prognosis and possible complications
The probability of consequences without treatment is 25% within 2-3 years. Under the condition of complex therapy - 10% or less. In 95% of cases, drug supervision has a positive effect. The remaining 5% requires the installation of a pacemaker.
Possible complications include:
- Heart attack. Acute malnutrition of the heart muscle with its subsequent death and replacement by scar tissue.
- Stroke (ischemic). Transient attacks.
- IHD and organ dysfunction.
- Heart failure.
- Cardiogenic shock.
- Death.
Causes and risk groups
Elderly people are primarily at risk for the development of pathological sinus bradycardia. The aging of the body is accompanied by a slowdown in metabolism, the development of atherosclerosis and other chronic diseases. Hereditary factors and congenital diseases also play a role. Long-term malnutrition, including prolonged dieting for the purpose of losing weight, can provoke bradyarrhythmia. The risk group also includes people who work with organophosphorus substances, abuse alcohol, and smokers.
If we consider the causes of bradycardia, we can traditionally distinguish external and internal provoking factors. However, such a discriminating approach would be wrong, since sometimes there is a close relationship between both groups. It is precisely the accurate clarification of the possible causes of bradyarrhythmia that allows you to correctly select a method of treating the disease.
External (extracardiac)
Highlight:
- Heredity.
- Physiological – old age, hypothermia, starvation.
- Hormonal defects – hyperaldosteronism, hypothyroidism.
- Alcohol and other toxic effects.
- Nervous diseases and disorders, including strokes, central nervous system infections, neuritis, VSD.
- Uncontrolled use of medications.
- Metabolic electrolyte disturbances.
- Hypoxia of various origins, including those associated with anemia, bronchitis, asthma.
Internal (cardiac)
Among heart diseases, the following are important for the occurrence of bradycardia:
- IHD – angina pectoris, heart attack.
- Vices.
- Myocarditis, pericarditis.
- Arterial hypertension.
- Dysfunction and degeneration of the sinus node.
- Atrial fibrillation.
- Atherosclerosis.
Important: Separate consideration should be given to ventricular repolarization syndrome, which was previously considered an ECG phenomenon characteristic of trained young men. The syndrome does not manifest itself clinically, but if it is present on the electrocardiogram, a person is considered to have a higher risk of sudden death. In recent years, cardiologists have suggested that the presence of repolarization syndrome precedes myocardial hypertrophy.
Prevention
Rejection of bad habits.
- Diet food.
- Proper drinking regime.
- Optimal physical activity (2-3 hours of absenteeism per day).
- A full night's rest (daytime does not cover it, the body works to exhaustion when “turning” circadian rhythms).
Sinus bradycardia of the heart is a decrease in heart rate of less than 60 beats per minute when the functional activity of a special accumulation of cells of a muscle organ is disrupted. Poses a significant danger to health and life. Treatment in a hospital setting, using several techniques. The risks are high, but with timely therapy they are much lower.
Folk remedies
Folk remedies can help with bradycardia with a heart rate of at least 40 beats per minute.
Most recipes use medicinal plants that lower the tone of the parasympathetic nervous system, increase myocardial contractions, or maintain blood pressure. They partly restore normal heart rhythm and partly prevent the development of complications. In case of hemodynamically significant bradycardia, it is not recommended to resort to traditional methods of treatment until a final diagnosis is made. Also, you should not take medicinal plants in parallel with drug treatment, as this increases the likelihood of unpredictable side effects.
The following recipes are used in the treatment of bradycardia with folk remedies:
- Yarrow decoction for bradycardia. You need to take 50 g of dry yarrow and fill it with half a liter of water. Boil for 10–15 minutes, and then leave for exactly an hour. You need to take a tablespoon of the decoction three times a day;
- Ginseng root. Take 15 g of dry root, grind, pour in 0.5 liters of vodka, leave for 20-30 days, shake every 1-2 days. Take 30–40 drops per day. The maximum duration of treatment is 1.5 months. Then take a month break.
- Natural grape juice has an excellent strengthening effect on the heart. The daily dose is 400 milliliters.
- Place a glass of boiling water with two tbsp in a water bath for 15 minutes. l. yarrow, then leave for another hour. Take the finished decoction three times, two tbsp. l. daily.
- Prepare the following composition - a collection of 30 g. calamus with rowan leaves, 50 gr. dandelion roots, currant leaves and hawthorn inflorescences. Place a tablespoon of the prepared mixture in 200 ml of boiling water, leave for half an hour, filter. The medicine should be taken twice a day.