Causes of the disease
Atherosclerosis occurs against the background of lipid metabolism disorders (dyslipidemia), in which the balance of lipoproteins of different densities changes, and they begin to be deposited in the vessel wall, gradually worsening blood flow. There are many factors that influence this process: from poor diet to congenital enzymopathies. The exact cause-and-effect chain of atherosclerosis still remains unknown.
Risk factors that cannot be controlled
Parameters that cannot be corrected by humans include:
- genetic predisposition;
- age;
- floor.
Modifiable risk factors
Elimination of the following processes and conditions will significantly reduce the risk of developing cerebrosclerosis:
- arterial hypertension;
- smoking;
- insulin resistance;
- diabetes;
- overweight;
- physical inactivity.
Disease prevention
Preventive measures must be maintained after illness throughout life, as well as for those who have a family history of atherosclerosis.
It is necessary to adhere to a healthy lifestyle, including:
- constant weight control;
- proper nutrition;
- increased physical activity;
- compliance with rest and work schedules;
- rejection of bad habits;
- reducing stress levels.
To reduce the risk of developing the disease, long walks in the fresh air, a positive emotional climate at work and at home, and long sleep are necessary. It is also recommended to undergo regular screening to detect early symptoms and to monitor cholesterol and low-density lipoprotein levels in the blood.
Atherosclerosis of the heart vessels is a dangerous disease, the wrong or untimely treatment of which can result in death from cardiac arrest or aortic rupture. Symptoms and treatment depend on the stage of the disease, the patient’s age and the presence of chronic diseases (hypertension, diabetes, renal failure, etc.). If the course of the disease is favorable, drug therapy in combination with diet and feasible physical activity is effective. In complex cases and with extensive damage, when there is a threat to life, surgical intervention is resorted to.
Symptoms and manifestations of cerebral atherosclerosis
There is no specific symptom that can indicate atherosclerosis. You need to understand that the manifestations directly depend on which vessel is affected and which area of the brain it supplies. Damage to a specific artery will give symptoms of dysfunction of the corresponding part of the organ that was supplied by it. The result can be a TIA (transient ischemic attack) or a stroke (it all depends on the degree of “starvation” of the nervous tissue). Frequent signs of pathology are:
- chronic or very intense headaches;
- periodic loss or deterioration of vision;
- noise in ears;
- periodic dizziness;
- feeling of numbness in the face or limbs;
- muscle weakness;
- emotional lability;
- panic attacks;
- speech disorder.
Doctors call symptoms of cerebral atherosclerosis by a general term: cerebral vascular syndromes in cerebrovascular diseases (ICD code - G46).
Features in the elderly
Atherosclerosis occurs much more often in old people than in young people. Old age is the most significant risk factor for the development of pathology. Moreover, it aggravates the course of diabetes and hypertension, which also affects the condition of the inner wall of the arteries. Treatment of cerebral atherosclerosis in older people is complicated by the blurring of symptoms, which can be confused with manifestations of concomitant pathologies. And this usually involves the loss of valuable time. In the case of an ischemic stroke, it is possible to remove the blockage of the vessel (thrombolysis) only in the next few hours.
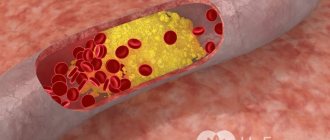
Mechanism of development of atherosclerotic plaque
There are 5 stages:
- Pre-lipid. Conditions are created for the formation of an atherosclerotic plaque: the vascular wall is injured. Changes in blood composition occur: the concentration of bad cholesterol increases. It ends when the body’s enzymes no longer have time to clear the artery wall of “plaque.”
- Lipoidosis. The second stage of atherosclerosis is the beginning of the formation of an atheromatous plaque. Cholesterol and low-density lipoproteins (LDL) begin to stick to the artery wall, forming fatty streaks and spots. The plaque is still so small that it does not impede blood flow.
- Liposclerosis. The site of deposition grows with connective tissue. The size of the atherosclerotic plaque increases.
- Atheromatosis. The destruction of fat deposits begins. The decay products form a dense mass that deforms the artery wall. At this point, the cholesterol plaque reaches a large size and interferes with the normal blood supply to the heart. Often the surface of the lesion begins to ulcerate, which provokes blood clots.
- Atherocalcinosis. Calcium salts are deposited in the thickness of the plaques. The density of the formation resembles stone. The risk of blood clots increases.
Classifications and variants of the course of cerebral atherosclerosis
Syndromes that are classified as cerebral vascular are divided depending on the vessel supplying a specific area of nervous tissue. When blood flow in one of the arteries of the head deteriorates, the corresponding sector of the brain completely or partially loses its function, which is determined by doctors when examining the patient. As a result, doctors begin to assume the localization of an atherosclerotic plaque. Main vasocerebral syndromes:
- middle cerebral artery syndrome;
- anterior cerebral artery syndrome;
- posterior cerebral artery syndrome;
- stem dysfunction syndrome;
- cerebellar stroke syndrome.
According to the clinical course:
- Preclinical period. Absolutely asymptomatic. It is very important at this stage to determine dyslipidemia (disorder of fat metabolism), which will prevent vascular damage.
- Latent period. Changes in the arteries can already be confirmed instrumentally, but the stability of the blood flow is still maintained - compensatory mechanisms are triggered.
- Nonspecific clinical manifestations. At this stage, headaches, impaired memory and cognitive function (the ability to concentrate and understand what is happening) and intermittent blindness appear. Emotional lability arises. Panic attacks, palpitations, lack of air, etc. are possible. Typically, such a patient is worried about exertional angina, arterial hypertension and other vascular pathologies.
- Severe atherosclerosis. This stage is characterized by serious ischemic disasters: TIA or stroke. The patient is advised to receive prompt medical attention, as a high degree of blockage of the vessel can be life-threatening.
Non-stenotic and stenotic type: what is the difference?
The difference between these two variants of the course of atherosclerosis is the degree of closure of the vessel by plaque. With the non-stenotic type it is up to 50%, with the stenotic type – more than half. This classification was introduced to determine the need for surgical intervention, but this does not mean at all that with a small blockage of the vessel the patient does not require treatment, or his life is not in danger. Even with a slight blockage of blood flow, a plaque can cause thrombosis, so any atherosclerotic narrowing of a cerebral artery requires constant treatment and monitoring by a doctor at least once every 6 months.
Progressive cerebral atherosclerosis
The term “progressive atherosclerosis” is usually used by doctors in cases of rapid worsening of arterial stenosis, which is often complicated by processes such as rupture, plaque fragmentation, and hemorrhage into it. The appearance of such a diagnosis indicates the transition of the disease from the stage of specific clinical manifestations to pronounced atherosclerosis.
Atherosclerosis of the main arteries of the head
The main central vessels of the brain are called “main”. Lipid damage to one of them causes deterioration or complete loss of many vital functions: sensitivity, movement, vision, hearing and others. Let's take a closer look at the syndromes (groups of symptoms) that are characteristic of each circulatory disorder in a specific artery.
Middle cerebral artery syndrome (ICD code G46.0):
- Hemiparesis is weakness of the muscles of one half of the body, for example, motor disturbances in the left arm and leg. In this case, the severity of the symptom in the upper limb is much stronger than in the leg.
- Hemihypesthesia is a violation of sensitivity in one of the halves of the body.
- Hemianopsia is bilateral blindness in one eye (loss of the right and left fields of vision).
- Brachiocephalic syndrome is paresis of facial muscles on the side of the affected artery.
- Prevost's syndrome is a contralateral gaze paresis (the eyes look in the opposite direction from the paralysis of the limbs).
- In case of damage to the dominant (leading in humans) hemisphere, aphasia (speech impairment) is possible.
Anterior cerebral artery syndrome (ICD code G46.1):
- Hemiparesis and hemihypesthesia are more pronounced in the leg.
- Problems with urination.
- Mental disorders, unreasonable aggression, memory impairment.
Posterior cerebral artery syndrome (G46.2):
- Homonymous (on the same side) complete or quadrant hemianopsia (vision loss in half of the visual field).
- Gerstmann-Schilder syndrome: agnosia (inability to perceive) fingers (your own and others): lack of distinction between left and right, acalculia (cannot count) and agraphia (write).
- Memory disorders.
- Korsakov's syndrome.
Brainstem dysfunction syndrome (G46.3)
This includes many alternating syndromes (lesions on the left, and symptoms on the right, and vice versa), which are divided into 3 large groups depending on the level of localization of the pathological process.
Bulbar alternating syndromes:
- Jackson syndrome is a peripheral paralysis/paresis of the tongue muscles (accompanied by its deviation from the median axis and twitching, as well as hemiparesis/paralysis on the opposite side.
- Avelisse syndrome is a unilateral paralysis of the palate and vocal cord and hemiparesis/paralysis on the opposite side.
- Schmidt's syndrome - unilateral paralysis of the palate, pharynx and vocal cord, paresis/paralysis of the sternocleidomastoid and trapezius muscles (accompanied by forced rotation of the head), as well as central hemiparesis and/or hemihypesthesia on the opposite side.
- Wallenberg-Zakharchenko syndrome - damage to pain and temperature sensitivity on one half of the face, dysfunction of the muscles of the palate and pharynx, decreased general sensitivity of the body on the opposite side, Horner's syndrome (drooping eyelid, constriction of the pupil, deep-set eyeballs), ataxia (unsteadiness when walking , loss of normal coordination of movements), dizziness.
Pontine alternating symptoms:
- Millard-Gubler syndrome is a peripheral unilateral paralysis of the facial muscles (paresis of the VII pair of cranial nerves) and hemiparesis on the opposite side.
- Foville syndrome is a peripheral unilateral paresis of the facial muscles and abductor oculi muscle (inability to move one eye to the side), as well as hemiplegia/paresis on the opposite side.
- Raymond Sestan syndrome - gaze paresis and hemiataxia towards the lesion, hemiparesis on the opposite half and sensory disturbances of the hemitype.
- Brissot's syndrome is a unilateral spasm of the facial muscles and hemiparesis on the opposite side.
- Gasperini syndrome is a homolateral paresis of the facial and trigeminal nerves (indicated by muscle paralysis and loss of sensation on one side), homolateral hearing loss and hemihypesthesia on the opposite half.
Cerebellar stroke syndrome G46.4:
- imbalance;
- "chanted" speech;
- loss of coordination of movements;
- tremor (shaking);
- nystagmus;
Symptoms
Atherosclerosis of the coronary arteries leads to constant oxygen starvation of the heart muscle.
So, the main manifestations of atherosclerosis of the heart vessels are angina pectoris and ischemic disease, which can be complicated by myocardial infarction and cardiosclerosis.
Symptoms of a heart attack are similar to an attack of angina, but longer lasting, with severe pain and shortness of breath, which does not stop under the influence of nitroglycerin. With a heart attack, heart failure develops very quickly, so urgent hospitalization is required.
With cardiosclerosis, heart failure also occurs, but this occurs gradually and is accompanied by severe shortness of breath, swelling, and loss of consciousness.
Diagnostics: how to determine cerebral atherosclerosis
To make a diagnosis of cerebral atherosclerosis, laboratory and instrumental examination methods are used. The first is aimed at determining the level of dyslipidemia and subsequent monitoring of the success of drug therapy. Hardware methods are used to search for plaques and localize stenosis, which is important for deciding on surgical treatment.
Laboratory diagnosis of cerebral atherosclerosis
When determining pathology, doctors evaluate the following indicators (the range of norms is indicated in parentheses):
- triglycerides (0.41-1.8 mmol/l);
- cholesterol (3.2 – 5.6 mmol/l);
- HDL-cholesterol (HDL): male. (0.7 – 1.73 mmol/l) female (0.86 – 2.28 mmol/l)
- LDL cholesterol (LDL): male. (2.25 – 4.82 mmol/l), women. (1.92 – 4.51 mmol/l)
- Apolyprotein A1: male (1.05 – 1.75 mmol/l), women. (1.05 – 2.05 mmol/l)
- Apoliprotein B: male (0.66 – 1.33 g/l) female (0.6 – 1.17 g/l)
- Atherogenic coefficient (2.2 – 3.5)
Instrumental examinations
The high mortality rate and frequent disability of patients with cerebrovascular accidents stimulates medical science to constantly improve equipment. Let's talk about the modern approach to determining cerebral atherosclerosis.
Dopplerography of head vessels
This examination refers to ultrasound techniques. It will show the speed and symmetry of blood flow in the main arteries of the brain. This is not the most accurate diagnostic method, but it is quite simple, fast and safe. An error can be caused by a simple displacement of the sensor, so two reports from different doctors on the same day can present different data, which will undermine a person’s adherence to treatment.
CT angiography of cerebral vessels
This method is much more informative than the previous one. But, unfortunately, it is more expensive and has risks: it uses x-rays, which involves some exposure to radiation, and the contrast used can cause an allergic reaction. Also, you will not be given this examination until you bring a blood test for creatinine clearance. The risk of “side effects” is not great: the dose of radiation exposure is minimal and cannot cause negative consequences once, and allergic reactions are extremely rare and can be successfully controlled with medications.
What examination should I undergo to reliably determine the problem? The choice is up to the doctor who assessed your clinical picture. Routine use of CT angiography is often not justified. If a person has no neurological complaints and is within the normal range during tests, then there will be no need for a CT scan. But if it is necessary to determine the lesion against the background of vivid symptoms, this examination becomes the diagnostic standard.
MRI angiography of cerebral vessels
The method is based on the influence of a magnetic field. The technique involves the use of contrast, but the negative impact of x-rays is no longer present. Claustrophobia can be a problem - the patient needs to lie without moving in a closed space for 20 minutes. An obstacle to performing an MRI will be the presence of metal prostheses, plates and electronics. The indications for the examination are the same as for CT angiography.
Doctor's advice: preventive check-up
Let's imagine a middle-aged person (up to 45 years old) without risk factors (they were discussed above). According to standards, it does not require special examination in the absence of symptoms. If unfavorable circumstances arise/identify, doctors will advise him to take a lipid profile once every two years. A confirmed diagnosis of cerebral atherosclerosis requires determination of blood fats every 3 months.
Diagnostics
Methods for diagnosing atherosclerosis of the aorta of the heart and other vessels include:
- anamnesis;
- laboratory research;
- non-invasive studies;
- invasive studies.
An important role in diagnosis is played by the study of family history, as well as the identification of the main risk factors: smoking, alcohol consumption, level of daily physical activity, nutrition, etc.
Laboratory methods
The first test is to determine the level of total cholesterol in the blood. For healthy people it is normal:
- total cholesterol: less than 5.0 mmol/l;
- low density lipoproteins: less than 3.0 mmol/l.
Then tests are prescribed to determine:
- high density lipoprotein levels;
- triglyceride levels;
- atherogenic index.
When diagnosing non-lipid risk factors, tests are prescribed to determine the level of:
- glucose;
- glycosylated hemoglobin;
- C-reactive protein in the blood;
- homocysteine;
- fibrinogen;
- apolyprotein A1 and B.
Additionally, blood pressure and body volume are measured to determine obesity or the amount of excess weight.
Non-invasive diagnostics
Non-invasive diagnostic methods include:
- electrocardiography;
- electrocardiography with stress test;
- echocardiography;
- MRI and CT;
- two-dimensional echocardiography;
- Doppler ultrasound of heart vessels;
- impedance plethysmography;
- radionuclide angiography.
These methods make it possible to determine the condition of the arteries and blood flow, the presence of thrombosis even in deep veins, the speed of blood flow, the size of atherosclerotic plaques and the condition of the heart muscle even after a recent heart attack.
Invasive methods
Invasive diagnostics of atherosclerosis of the aorta and other heart vessels includes:
- intravascular ultrasonography;
- angiography;
- intravascular magnetic resonance imaging;
- angioscopy;
- plaque thermography;
- optical coherence tomography;
- elastography.
Using invasive diagnostic methods, it is possible to assess the structure of the walls of the coronary arteries, visualize the types of atherosclerotic plaques, identify the sites of stenosis and clarify the nature of damage to the vessel walls. Additionally, you can obtain data on morphological changes in tissues, identify unstable plaques and plaques with a high content of lipoproteins.
Treatment: how to deal with the disease
Let's see what treatment methods modern standards offer. They are based on the principles of evidence-based medicine.
Non-drug treatments
The pre-medicinal stage consists of changing lifestyle to eliminate risk factors, and more precisely in:
- quitting smoking;
- moderate alcohol consumption;
- physical activity;
- proper nutrition (Mediterranean diet);
- combating stress;
- the fight against excess weight.
Drugs for cerebral atherosclerosis
For effective treatment of cerebral atherosclerosis, it is necessary not only to correct lipid metabolism, but also to eliminate all possible diseases that damage the vessel wall. Most often, pathology originates in vulnerable places: bifurcations (bifurcations of arteries), bends. For many, it is combined with hypertension and diabetes, which aggravates the development of the disease. These pathologies cause disturbances in vascular tone and metabolism, which impairs the susceptibility of dyslipidemia to treatment. What do doctors prescribe for cerebral atherosclerosis according to the protocols, and what medications are our patients waiting for?
Interfering with cholesterol absorption
Angio-exchange resins. The class includes drugs that adsorb cholesterol. These include Cholestyramine and Gemfibrozil. The effect appears after a month of use and persists for several more weeks after discontinuation of the medication.
Plant sorbents. These drugs block the absorption of exogenous cholesterol in the intestine. They require large amounts of fluid and sometimes cause dyspepsia. The representative of the group is the drug Guarem.
An Ac-CoA transferase blocker is a substance that is under development. There are high hopes for him in medical circles. The mechanism of action is to prevent the uptake of cholesterol from the intestines.
We must remember that 2/3 of cholesterol is produced by our body and the problem is not always its excessive supply from the outside.
Reduced synthesis of endogenous cholesterol and triglycerides
This class of drugs includes HMG-CoA reductase inhibitors or the well-known statins. Their main representatives: Simvastatin, Lovastatin, Rosuvastatin, Atorvastatin. These drugs are very effective, but at the same time they cannot be widely used. They are prohibited for children, pregnant and lactating women, and people with liver damage. Among the most unpleasant side effects: rhabdomyolysis, myopathy, alopecia, impotence and liver failure. This category of drugs is included in the treatment protocols of most countries, being in the first line of recommendations.
Fibric acid derivatives are better known as fibrates: Taikor, Lipanor, Bezalip. Now it is recommended to use a new generation product - Fenofibrate - or fenofibric acid derivatives. Often used for concomitant type II diabetes mellitus.
For severe dyslipidemia, a combination of a statin and a fibrate may be used.
Unsaturated fatty acids
This group includes substances that increase the breakdown of atherogenic lipids. Representatives: Omacor, Eikonol, thioctic acid preparations. The FDA (the main American drug certification body in the USA) classifies these products as dietary supplements.
Endotheliotropic drugs
Manufacturers of these products claim that they reduce the amount of cholesterol in the intima (inner lining of the vessel). The series includes: Parmidine, Misoprostol, Polycosanosis, vitamins A, E, C.
Science does not stand still - scientists are working to find new drugs for the treatment of atherosclerosis. Cyclodextrin is considered promising because it dissolved cholesterol crystals in experiments. Also making a lot of noise is AEM-28, a peptide that can not only amazingly quickly reduce the level of atherogenic lipoproteins and triglycerides, but also have an anti-inflammatory effect. Perhaps the solution will be drugs that inhibit the translation of apolipoprotein mRNA - the stakes for them are very high.
Restoring memory and cognitive abilities
No existing drugs have been shown to be highly effective in treating vascular dementia, which is responsible for loss of cognitive function and memory. The person and his relatives must understand that such a diagnosis means the death of part of the brain. This entails the patient’s irrevocable limitation in something. The main task is the care and prevention of ischemia - taking blood pressure pills and blood thinners. As for help: here time is the best healer. Neuroplasticity has not been canceled, although in old age the processes of neuronal restoration are not so active, but every day new connections are created in the brain. And only full-fledged stable rehabilitation can speed up this process.
In the medical community, the use of Memantine and cholinesterase inhibitors is very popular, but, I repeat, studies prove their low effectiveness and economic inexpediency. These drugs are indicated for the combination of vascular dementia with Alzheimer's disease.
Relief of symptoms
Headaches are relieved with non-steroidal anti-inflammatory drugs. The most popular of them: Aspirin, Ibuprofen, Paracetamol. If intracranial pressure increases (which is not uncommon in vascular dementia), Diacarb can be used.
To eliminate dizziness, you can use Betaserc or Dimenhydrinate. If the condition worsens, we recommend that you immediately consult a doctor for a consultation - this symptom can be life-threatening.
For ringing in the ears (tinnitus), doctors often use Phenibut, which eliminates anxiety and dizziness. Sometimes persistent extraneous sounds in the ears can be a sign of an aneurysm.
Continuous tablets
Drugs are used on a stable basis for the permanent treatment of cerebral atherosclerosis:
- for correction of lipid metabolism;
- to lower blood pressure - see the list of medications here;
- for the treatment of diabetes mellitus.
The list of drugs may be supplemented depending on the presence of concomitant diseases. A person with cerebral atherosclerosis must be compensated. This means that he needs to receive pills for all chronic conditions in order to remain stable.
Is there surgical treatment?
Endovascular operations are used to treat cerebral atherosclerosis. They involve inflating the narrowing site with a special balloon and placing a stent (spring) that will prevent the vessel from narrowing. Stents vary in composition and cost. Cheap designs carry a risk of re-clogging. The technique is relevant for:
- severe stenosis, when more than half of the lumen of the vessel is covered with plaque;
- failure to improve the patient's quality of life with medications;
- no contraindications.
How can the patient’s quality of life be improved, and what is the prognosis?
A team of specialists should work on the social and physical recovery of the patient: a rehabilitation specialist, a therapist, a neurologist. Modification of the patient's lifestyle is mandatory: proper nutrition and daily activity are of enormous importance, along with the constant intake of the right medications.
The course of atherosclerosis and its prognosis are influenced by many factors. This pathology is a kind of bomb, which, when it explodes, leaves some vital organ without power (heart attack, stroke). In certain cases, a person can live for years with severe dementia. And sometimes a sudden heart attack knocks down a young, able-bodied man. It is important to understand that only a healthy lifestyle is the only way to happily meet old age, and if an illness overtakes you, treat it correctly.
Diet for atherosclerosis
Treatment and prevention of atherosclerosis involves a constant diet that limits the intake of animal fats. It is important not only to count the daily number of calories, but also to create a menu so that:
- the amount of proteins did not exceed 15%;
- the amount of fat did not exceed 30%;
- the amount of carbohydrates did not exceed 55%.
When creating a menu, it is necessary to replace fatty meats with fish, poultry or legumes. Only low-fat milk and dairy products are allowed. Be sure to include in your diet foods containing polyunsaturated and monounsaturated fatty acids (seafood, vegetable oils). Patients with atherosclerosis are recommended to include dishes made from fatty sea fish (tuna, salmon) twice a week.
It is necessary to exclude strong and carbonated drinks, canned foods, fast food, flour and sausages from the diet. An important place in the diet should be given to fresh vegetables (except potatoes) and fruits, legumes, cereals (except rice), as well as nuts and durum wheat bread.
Stages of development
The development of atherosclerosis is divided into three main stages
The onset of the disease is not sudden. The development of atherosclerosis is slow due to the accumulation of lipids on the internal surfaces of blood vessels. The process is divided into three main stages:
- the first - in which there is a gradual decrease in blood flow. The vascular walls are covered with microcracks. Fat cells actively accumulate in them. Over time, the cracks get larger. Cholesterol clots grow along with them;
- the second is called liposclerosis. The rate of growth of adipose tissue increases significantly. In this phase, the pathology is well treated. Fat clots can be dissolved. The possibility of thrombosis increases significantly, which can lead to blockage of the artery and death of the patient;
- the third is atherocalcinosis. Plaques in the heart vessels begin to thicken. This leads to calcium deposits, narrowing of the lumen occurs, and the size of the blood clot actively increases, which leads to deformation of the vessel walls. The risk of developing occlusion and necrosis increases significantly. Gangrene sometimes begins to develop in these areas.
Therapy largely depends on the degree of development of atherosclerosis. Treatment in later stages is complex and lengthy, but this does not always lead to a positive result. For this reason, efforts should be made to identify the disease at an earlier stage of development.