- headache,
noise in ears,
Pressure readings can reach critical numbers, and then we are talking about the possible development of a hypertensive crisis. Hyperglycemia can reach 25 mmol/l, in which case the risk of hyperglycemic coma is increased.
In diabetes, the functioning of the vascular system of the brain is impaired. Patients complain of chronic fatigue and lack of logical thinking.
High blood pressure in type 1 and type 2 diabetes: causes
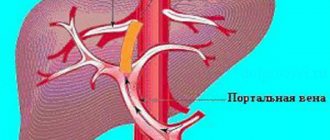
Diabetes mellitus type 1 and 2 is a common microangiopathy, that is, damage to the microvasculature. The longer diabetes lasts and the less diligently blood sugar is controlled, the more likely patients develop vascular damage. Diabetic foot is a common condition - microangiopathy of the lower extremities, accompanied by tissue death and requiring amputation.
One might think that high blood pressure in type 1 and type 2 diabetes will help maintain adequate blood supply to tissues and there will be no vascular disorders. Fluctuations in pressure aggravate vascular disorders in diabetes and lead to dangerous consequences, which will be discussed in the next section.
Arterial hypertension in type 1 and type 2 diabetes is due to various reasons. Type 2 diabetes mellitus is an acquired metabolic disorder that is common in people with excess body weight. And excess weight is always accompanied by arterial hypertension.
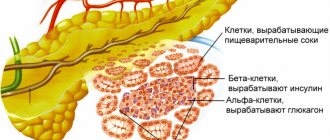
Why do patients with type 1 diabetes develop arterial hypertension? This is usually associated with kidney damage, namely the loss of protein in the urine due to glomerular microangiopathy. Renal dysfunction in patients with type 1 diabetes is characterized by three successive stages:
- Microalbuminuria, when molecules of a small molecular weight albumin protein appear in the urine, and the loss of protein through the kidneys itself is not expressed. The blood pressure remains normal, and timely identification of the condition and prescribing appropriate treatment will delay further kidney damage.
- Gradually, kidney damage due to type 1 diabetes worsens, and large proteins pass through the tubules along with albumin. This leads to a general increase in the loss of protein fractions in the urine and characterizes the stage of proteinuria. Here the pressure is already increased, and the amount of protein lost through the kidneys is directly proportional to the blood pressure numbers.
- The last stage of kidney damage in diabetes is chronic renal failure. The condition of a patient with type 1 diabetes is steadily deteriorating and there is a need for hemodialysis.
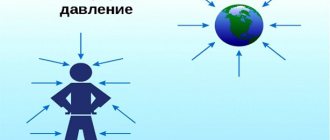
Blood pressure in diabetic patients may be elevated or become hypotensive. Impaired kidney function causes sodium to accumulate in the body. Sodium attracts water, which goes into the tissue. An increase in sodium and fluid accumulation leads to a persistent increase in pressure.
In 10% of patients, arterial hypertension is not associated with type 1 diabetes and develops as a concomitant disease, as evidenced by the preservation of kidney function. In elderly patients, systolic hypertension may appear when only the upper blood pressure is elevated. This situation is also not associated with diabetes, but hyperglycemia significantly aggravates the course of hypertension.
With type 2 diabetes, the kidneys will also suffer, which aggravates the existing hypertension in patients.
The likelihood of arterial hypertension in type 1 and type 2 diabetes is increased by the following unfavorable factors in the lives of patients:
- Stress, emotional and physical stress;
- Age after 45 years;
- Passive lifestyle;
- Abuse of fatty foods, fast food, alcohol;
- Increased body weight;
- Hereditary history – hypertension in blood relatives.
These factors lead to complications in patients with type 1 and type 2 diabetes with existing arterial hypertension.
Reasons for development
Diabetes and blood pressure are diseases that often complement each other. Moreover, the main cause of hypertension in T1DM is diabetic nephropathy, which is characterized by kidney damage and impaired functionality.
The causes of high blood pressure in this disease can also be:
- impaired patency of the kidney vessels;
- essential or isolated systolic hypertension;
- endocrine disorders.
As for endocrine disorders in the body that provoke the development of hypertension in diabetes, the most common among them are:
- Itsenko-Cushing syndrome;
- pheochromocytoma;
- hyperaldosteronism and others.
In addition, high blood pressure in T1DM and T2DM can be observed:
- with a lack of a chemical element such as magnesium in the body;
- psychological disorders that arise against the background of frequent stress, mental overstrain, depressive states, etc.;
- exposure to toxic substances (for example, mercury, lead or cadmium);
- atherosclerosis, causing narrowing of large arteries.
Symptoms of arterial hypertension in diabetes
Elevated blood pressure in type 1 and type 2 diabetes manifests itself in the same way as in patients with normal blood sugar. These are headaches, spots flashing before the eyes, dizziness, heaviness in the back of the head and others. Long-term hypertension leads to adaptation of the body, and the patient does not feel it.
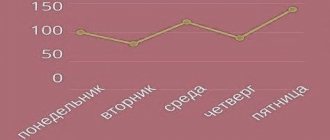
In a healthy person, blood pressure decreases by 10-20% at night. For patients with type 1 and type 2 diabetes, it is noteworthy that during the day the pressure numbers can remain normal, but at night they do not decrease, as in healthy people, and sometimes increase. This is associated with diabetic neuropathy, which alters the regulation of arterial tone. Violation of the correct fluctuation of the daily rhythm of blood pressure in diabetes increases the risk of myocardial infarction, even if the blood pressure numbers do not exceed the norm.
About the types of blood pressure medications
The leading drugs are diuretics, that is, having a diuretic effect, as well as beta-type blockers, calcium antagonists, otherwise called calcium channel androgens. In addition, this category includes ACE inhibitors and angiotensin II receptors, which can block them.
The combination treatment includes additional types of drugs: rasilez (which is also a direct renin inhibitor), alpha adrenergic blockers, as well as agonists that provide a targeted effect on the nervous system. All these medications should be used only in accordance with medical recommendations. Otherwise, the negative impact can be very significant.
Thus, to lower blood pressure in both types of diabetes, drugs from the following groups are usually used:
- inhibitors: Enalapril, Captopril;
- diuretics: Diacarb, Furosemide;
- beta blockers: “Dilatrend”, “Trandat”, “Nebilet”;
- calcium antagonists: Verapamil, Diltiazem;
- alpha-blockers: Terazosin, Prazosin, Doxazosin;
- stimulants (agonists) of imidazoline receptors: Physiotens, Albarel.
Each group of drugs will be discussed in detail below.
Why is high blood pressure dangerous in diabetes?
Arterial hypertension is dangerous due to cardiovascular complications, and in combination with diabetes, these risks increase significantly. In patients with arterial hypertension and diabetes mellitus types 1 and 2, the following are more often observed:
- 20 times non-healing trophic ulcers and gangrene of the extremities requiring amputation;
- 25 times the development of renal failure;
- 5 times the development of myocardial infarction, which is more severe than in patients with normal blood sugar and leads to death;
- Strokes develop 4 times;
- A sharp decrease in vision is recorded 15 times.
Blood pressure is reduced in type 1 and type 2 diabetes by prescribing medication and lifestyle modifications. Staged treatment is used with a gradual increase in the dose of antihypertensive drugs. In the first month, the target is to achieve 140/90 mmHg. Next, doctors try to select treatment so that the pressure is in the range of 110/70 – 130/80.
There are categories of patients in whom it is not possible to reduce blood pressure to less than 140/90. These are persons with severe kidney damage, atherosclerosis, or older patients whose target organs are already damaged (decreased vision, hypertrophied myocardium).
Diuretics for patients with diabetes mellitus
Medicines such as diuretics remove excess fluid, thereby reducing vascular pressure.
There are four types of diuretics: potassium-sparing, loop, thiazide-like, thiazide.
Thiazide-like diuretics, which do not affect glucose levels, produce an excellent effect. Diabetes mellitus of both types requires the use of thiazide diuretics in quantities that do not exceed 12.5 milligrams. Both diuretic groups prevent the occurrence of renal complications and myocardium, but such drugs are prohibited for use in cases of renal failure.
Diuretic loop medications are rarely prescribed because the body loses potassium as a result. However, they are indicated for kidney failure, in which case additional medications with potassium are prescribed.
Potassium-sparing diuretics are also rarely used in diabetes, as they have a slight hypotensive effect.
How to lower blood pressure in diabetes: drug approaches
Drug treatment of arterial hypertension in type 1 and type 2 diabetes is carried out by several groups of drugs. This allows you to potentiate the beneficial effects of different groups, because in addition to lowering blood pressure, they also have other points of application. The requirements for antihypertensive drugs are as follows:
- Maintain normal blood pressure for 12-24 hours;
- Do not affect blood sugar, nor cause hypercholesterolemia;
- Protect internal organs, especially the kidneys, from the harmful effects of arterial hypertension and diabetes.
It is better when 1 tablet includes several antihypertensive drugs. There are fixed pharmaceutical combinations that give a greater hypotensive effect than if the patient takes these medications, only in different tablets: Noliprel, Bi-Prestarium, Equator, Fozid, Korenitek and others.
The following drugs are approved for the treatment of hypertension in diabetes:
- ACE inhibitors (angiotensin-converting enzyme);
- Calcium blockers;
- Some diuretic medications;
- Selective beta blockers;
- Sartans.
ACE inhibitors
The action of drugs for the treatment of hypertension is based on blocking the enzyme angiotensin 2, which constricts blood vessels and increases the production of aldosterone, a hormone that retains water and sodium. This is the first drug prescribed to a patient with diabetes and hypertension for reasons:
- The antihypertensive effect of ACE inhibitors is mild and gradual - a persistent decrease in blood pressure is observed after 2 weeks of taking the drug;
- Medicines protect the heart and kidneys from complications.
The protective effect of drugs in type 1 and type 2 diabetes is due to their effect on the renin-angiotensin-aldosterone system, which prevents early kidney damage. Also, ACE inhibitors prevent the development of atherosclerosis due to the protection of the inner lining of arterioles from the deposition of cholesterol plaques on it. ACE inhibitors have a positive effect on the metabolism of fats and blood sugar, reduce tissue insulin resistance, that is, reduce blood glucose.
Additional effects of hypertension drugs are not observed with all drugs containing inhibitors. Only original medicines protect the heart and affect lipid and carbohydrate metabolism. But generics (copies) do not have such effects. When asked what to buy, cheap enalapril or branded Prestarium, remember this feature.
Disadvantages of medications for the treatment of hypertension:
- ACE inhibitors somewhat slow down the excretion of potassium from the body, so periodic determination of potassium in the blood is necessary. Potassium slows the heart rate and, in excess, can cause life-threatening arrhythmias and cardiac arrest. Hyperkalemia in patients with type 1 and type 2 diabetes is a contraindication for the prescription of ACE inhibitors.
- ACE inhibitors cause a reflex cough in some patients. Unfortunately, this side effect cannot be eliminated and the medicine has to be replaced with sartans.
- High arterial hypertension is not regulated by these drugs, and in some patients the hypotensive effect may not appear at all. In such situations, doctors keep ACE inhibitors as medications to protect the heart and add other antihypertensive medications.
A contraindication for the treatment of hypertension with ACE inhibitors in type 1 and type 2 diabetes (as well as sartans) is bilateral renal artery stenosis. Also, medications are contraindicated in patients who have a history of angioedema (an immediate allergic reaction).
Calcium blockers
Calcium channel blockers or long-acting calcium antagonists reduce blood pressure in patients with type 1 and type 2 diabetes, but have their own contraindications. These drugs are divided into 2 groups: dihydroperidine and non-dihydroperidine. They differ in their mechanism of action.
The main difference is that dihydroperidine blockers increase heart rate, while non-dihydroperidine blockers decrease it. Therefore, dihydroperidines are not prescribed for high heart rates. But for patients with bradycardia, these medications are ideal.
Blockers of both groups are not used for the treatment of hypertension in the acute post-infarction period, in people with unstable angina (a temporary condition that can develop into a heart attack or stabilize) and in case of insufficient cardiac function.
Dihydroperidine blockers reduce the likelihood of developing myocardial infarction in diabetes, but not as pronounced as ACE inhibitors. Antagonists are ideal for treating patients with systolic hypertension and reduce the likelihood of stroke.
Non-dihydroperidine calcium channel blockers are suitable for the treatment of hypertension in patients with diabetic nephropathy. They protect the kidneys from the effects of high blood sugar. Dihydroperidine antagonists do not protect the kidney. All calcium channel blockers for diabetes are combined with ACE inhibitors and diuretics. Non-dihydroperidine blockers should absolutely not be combined with beta-receptor blockers.
Diuretics for patients with diabetes mellitus
To treat hypertension in diabetes, diuretics are always combined with additional drugs, for example, ACE inhibitors. Medicines have different mechanisms of action and are divided into groups. For hypertension, 4 main groups of diuretics are used:
- Loop: furosemide and torasemide;
- Potassium-sparing: veroshpiron;
- Thiazide: hydrochlorothiazide;
- Thiazide-like: indapamide.
Each group has its own characteristics. Thiazide and thiazide-like diuretics have proven themselves to be especially effective in drug combinations for the treatment of hypertension (often with inhibitors). Only the former in large doses can cause an increase in blood sugar, therefore, for hypertension and diabetes of the first and second types, they are prescribed with caution, and in a dose not exceeding 12.5 mg. Considering that the diuretic is combined with another medicine, this amount is sufficient. Thiazide-like diuretics do not affect blood glucose and are well tolerated by patients with hypertension.
Thiazide and thiazide-like diuretics protect blood vessels, preventing or delaying the development of complications from the heart and kidneys. If cardiac function is insufficient, medications are prohibited. These diuretics are not prescribed for the treatment of hypertension due to gout.
Loop diuretics are rarely used for long-term use because they remove potassium through the kidneys. Therefore, when prescribing furosemide and torsemide, potassium supplements must be prescribed. Only these diuretics are allowed for patients with low kidney function, so in cases of severe hypertension, doctors prescribe them for long-term use.
Potassium-sparing diuretics for diabetes fade into the background. They do not harm patients, but have a weak hypotensive effect and are not characterized by any other positive effects. They can be used, but it is better to replace them with other, more useful and effective groups that protect the kidneys and other organs.
Selective beta blockers
Beta-receptor blockers are fairly strong antihypertensive drugs that have a good effect on the heart. They are used in patients with rhythm disturbances and high heart rates. Beta-receptor blockers have been shown to reduce the likelihood of death from heart disease and are among the first-line medications for hypertension and diabetes.
There are 2 main groups of blockers: selective, selectively acting on receptors of the heart and blood vessels, and non-selective, affecting all tissues. The latter are characterized by the fact that they increase tissue insulin resistance, that is, they increase blood sugar. This is an undesirable effect for diabetic patients, so non-selective blockers are strictly contraindicated.
Selective or selective drugs are safe and useful for patients who have diabetes mellitus and hypertension combined with the following pathologies:
- Cardiac ischemia;
- Myocardial infarction (in the early post-infarction period, blockers reduce the likelihood of relapse and restore heart function, and in the late period they prevent the risk of recurrent myocardial infarction);
- Heart failure.
Selective blockers for diabetes combine well with diuretics. Less commonly used together with ACE inhibitors and calcium blockers.
Beta receptor blockers (selective and non-selective) are contraindicated for the treatment of hypertension in patients with bronchial asthma, as they can worsen the course of the disease.
Sartans
The mechanism of action of drugs is similar to ACE inhibitors. Sartans are rarely used in the complex of first-line drugs; they are prescribed when taking ACE inhibitors in a patient provokes a cough. These medications protect the kidneys, lower cholesterol and blood glucose, but to a lesser extent than ACE inhibitors. Sartans have a higher cost, and fewer fixed combinations with other antihypertensive drugs are known.
Sartans are one step above ACE inhibitors when it comes to treating patients with an enlarged left stomach. It has been proven that these drugs not only slow down hypertrophy, but also cause its reverse regression.
Like ACE inhibitors, sartans cause potassium accumulation, so hyperkalemia in type 1 and type 2 diabetes is a contraindication to the use of drugs. The drugs combine well with diuretics and will be effective as monotherapy. In combination with sartans, the effectiveness of calcium blockers improves (as when taking ACE inhibitors).
Additional groups of antihypertensive drugs - alpha blockers for diabetes
When taking the main medications to treat hypertension is not possible, or a combination of the two medications described above does not give the necessary antihypertensive effect, drugs from the reserve groups are added to treatment. There are quite a lot of them, so we will consider only alpha-receptor blockers that are approved for type 1 and type 2 diabetes.
The advantage of these drugs is that they reduce prostatic hyperplasia, so they can be used as the drugs of choice for treating patients with this problem and diabetes. At the same time, medications increase the risk of developing heart failure. This effect has not been definitively proven, but alpha-receptor blockers are not used in patients with existing heart failure.
Among other positive effects, we note their effect on blood glucose. Medicines increase tissue sensitivity to insulin and reduce blood sugar, which is necessary for diabetes.
What medications for arterial hypertension are contraindicated in diabetes?
Due to the high prevalence of hypertension, doctors have many groups of drugs that lower blood pressure in their arsenal. Some of them cause an increase in blood sugar and are strictly contraindicated for patients with diabetes. This is especially true for non-selective beta receptor blockers.
They are absolutely contraindicated in cases of impaired glucose tolerance (prediabetes). Also, medications are prescribed with caution to patients whose blood relatives have diabetes.
In diabetes, thiazide diuretics in doses greater than 12.5 mg are contraindicated. Their effect on insulin and blood glucose is not as pronounced as that of non-selective beta-receptor blockers and non-dihydroperidine calcium antagonists, but it is still present.
About therapeutic methods
One of the most effective ways to combat blood pressure in diabetes mellitus is strict adherence to the principles of a dietary diet. In this case, we are talking about a low-carbohydrate diet, and it is suitable only for those patients who do not yet have renal failure.
The presented nutritional features are completely safe and useful also at the stage of microalbuminuria. This is explained by the fact that when blood glucose decreases to normal values, the kidneys begin to work quite optimally.
Because of this, the proportion of albumin found in urine returns to normal, which also has a positive effect on high blood pressure.
Weight loss will improve the patient's overall condition.
Maintaining a healthy lifestyle and maintaining the correct daily routine, playing sports, and physical activity have a positive effect on blood vessels and reduce blood glucose levels.
When choosing specific pills and drugs, the doctor must take into account how exactly the patient controls the process of diabetes, and whether he has satellite diseases formed in addition to hypertension. In this regard, we can say with confidence that blood pressure medications must meet the following indicators:
- significantly reduce blood pressure, but so that along with this there is a minimum number of negative manifestations;
- do not affect the deterioration of blood glucose control and do not increase the proportion of “bad” cholesterol and triglycerides;
- create complete protection for the kidneys and heart from the harm that both diabetes and rapidly developing high blood pressure can cause them.
There are currently eight categories that include medications for hypertension. Five of them are basic, three are additional. Blood pressure medications for diabetes mellitus, which are considered additional, should be used primarily as a mixed treatment. It is important to follow all doctor's recommendations. In this case, blood pressure in diabetes mellitus will be effectively brought to normal levels.
Combating hypertensive crisis in diabetes
A hypertensive crisis requires an immediate reduction in blood pressure. All of the above medications used for long-term treatment of patients with diabetes are effective, but act slowly. Short-acting medications are used to urgently lower blood pressure.
Pressure figures during a hypertensive crisis will be different for each patient. What medicine should I take before the ambulance arrives and not make my diabetes worse? The most common is the angiotensin-converting enzyme inhibitor captopril. The drug is not contraindicated in diabetes and can quickly reduce blood pressure.
Sometimes it is not enough, then you can supplement the action with the diuretic furosemide. There is an available fixed combination of inhibitor and diuretic - captopres. This drug must be in the first aid kit of a diabetic patient.
A captopril or captopres tablet under the tongue for 10-15 minutes lowers blood pressure. Caution: if the blood pressure numbers are not high, then use half the tablet so as not to cause hypotension.
The fast-acting calcium antagonist nifedipine can also be used. During a hypertensive crisis, the pressure should decrease gradually. During the first hour, blood pressure should be lowered by 25%. Then the decline should be even softer.
Also do the following:
- Lie on the bed with your head elevated and legs down;
- Use a cold compress on your forehead;
- Try to calm down.
As soon as you see high blood pressure numbers, call an ambulance. Qualified specialists will provide further treatment and eliminate complications of the crisis.
Main features
Risk factors
Hypertension in type 2 diabetics generally occurs without specific symptoms. And such manifestations as emerging headaches, a feeling of dizziness, and blurred vision are characteristic of many diseases.
It is common for a person to experience pressure fluctuations throughout the day - a decrease in levels at night and in the morning by up to 20%. A diabetic's blood pressure may be higher at night than during the day. This happens due to an increase in blood glucose, so-called diabetic neuropathy develops.
The vessels lack the ability to respond to stress, to narrow and expand in time. Patients are forced to frequently measure their blood pressure throughout the day. It is important to determine with great accuracy the required amount and hours when it is best to use high blood pressure pills.
Diabetes is characterized by orthostatic hypotension - a sharp decrease in blood pressure due to a change in the person’s body position. If the patient gets up after lying on his back, with low blood pressure, circles appear before the eyes, dizziness, and fainting is possible.
How to eliminate arterial hypertension: general recommendations
If you have hypertension, you should reduce your salt intake, as it causes fluid retention and arterial hypertension. Patients with diabetes are more sensitive to sodium, so it is strongly recommended to reduce the amount of salt.
You should also limit your fluid intake to 1 liter per day (in hot weather you are allowed to drink about 1.5 liters). Liquid is not only water, but also juices, soups, vegetables, fruits.
Food should be salted less, gradually the taste buds will adapt, and it will not seem bland. A simple rule from European experts: “Take the salt shaker off the table” will help you start consuming less salt. This simple measure will eliminate the habit of adding salt to food and reduce salt consumption by about a quarter.
The following recommendations will help improve the quality of life with diabetes and hypertension and reduce the dose of antihypertensive drugs:
- Give up alcohol and cigarettes;
- Get enough sleep - sleeping at least 7 hours a day is the key to a good emotional state and equal blood pressure;
- Walking in the fresh air calms the nervous system and improves heart function;
- A low-carbohydrate diet, avoiding fatty and fried foods will reduce the negative impact on blood vessels, minimize the likelihood of developing atherosclerosis, and reduce the severity of hypertension;
- Excess weight always accompanies high blood pressure, so losing weight slowly will help reduce the symptoms of hypertension and improve the general condition of the body.
Antihypertensive drugs have a cumulative effect, so they should be taken regularly. Normalization of blood pressure means that the treatment is effective. Don't think that you have cured your hypertension and can quit the pills. This disease is incurable and requires lifelong treatment. And intermittent therapy will only worsen its course.
Preventive measures
Since diabetes already places an increased burden on the cardiovascular system, the development of hypertension can be prevented by following these recommendations:
- Strict diet and weight control, avoidance of harmful and cholesterol-containing foods.
- Increased physical activity, toning blood vessels.
- Rejection of bad habits.
- Timely intake of medications prescribed by the doctor.
It is important for a diabetic to know that hypertension is a frequent and insidious companion of hyperglycemia, which takes away years of life. It is impossible to completely get rid of the disease, but with the help of well-chosen treatment and diet, you can keep the situation under control. No medications will help if the patient continues to lead a sedentary lifestyle and eat whatever he wants.
Andrey Yurievich
Prevention of arterial hypertension in diabetes
It is important to prevent arterial hypertension in type 1 diabetes, because hypertension occurs as a consequence of hyperglycemia. Patients with type 2 diabetes should also maintain normal blood pressure, but due to the fact that hyperglycemia and hypertension develop as two independent diseases, this measure is somewhat difficult. For such patients, all the recommendations outlined in the previous section will serve as prevention of arterial hypertension.
Preventing the development of hypertension in type 1 diabetes means preventing kidney damage. ACE inhibitors, prescribed in low doses for normal blood pressure and in standard doses for hypertension, can cope with this task. Medicines well protect the microvasculature, in particular the glomeruli of the kidneys, which ensures their nephroprotective effect.
If a cough develops while taking them, inhibitors can be replaced with sartans, which also have a nephroprotective effect. However, in case of hyperkalemia, the drugs are contraindicated.
Prophylactic administration of ACE inhibitors is also applicable for patients with type 2 diabetes, especially if it is not combined with hypertension (which is extremely rare). Impaired renal function is dangerous due to the worsening of hypertension and renal failure. To promptly detect microalbuminuria, you should take a urine test every 3-6 months to determine protein.
A standard general urine test for hypertension will not detect small amounts of protein, so a test for microalbuminuria is prescribed.
Treatment
The upper limit of normal for a diabetic is 130/80 mmHg. Art., which is a so-called landmark. Usually, doctors, in addition to medications, prescribe a diet to the patient, which also helps to slightly reduce blood pressure.
The pressure must be reduced gradually so that a persistent hypotonic state does not develop. In addition, patients with diabetes can often suffer orthostatic collapse due to a sudden change in body position. It may be accompanied by fainting and severe dizziness. Collapses are treated symptomatically to prevent a persistent rise in pressure.
Low blood pressure in diabetes: causes and symptoms
Low blood pressure in diabetes is much less common than hypertension. This is due to the cascade of obligatory disorders that hyperglycemia leads to. Low blood pressure can occur either at the onset of diabetes mellitus, which has nothing to do with the disease and is a feature of this patient. Over time, such hypotension develops into normal pressure, and then into arterial hypertension due to impaired renal function.
It happens that arterial hypertension develops into hypotension. This condition is dangerous. For a diabetic patient, even a blood pressure of 110/60 can become very severe and lead to fainting. Therefore, patients should monitor their blood sugar and measure their blood pressure daily.
Causes of hypotension in diabetes:
- Disruption of the autonomic nervous system due to increased fatigue, stress and vitamin deficiency. Lifestyle correction in most cases allows you to correct this situation if it is not running.
- Heart failure due to damage to the heart and coronary arteries. This condition is very dangerous and develops in advanced cases. Patients with heart failure and diabetes require mandatory hospitalization and specific treatment.
- Overdose of medications that lower blood pressure. If hypertension in diabetes suddenly turns into hypotension, the patient did not follow the doctor’s recommendations correctly. This is not a reason to quit taking pills and wait for your blood pressure to rise, because sudden changes can lead to life-threatening conditions. You should consult a doctor so that he can review the prescribed treatment and normalize the blood pressure.
It is difficult to say what kind of blood pressure in diabetes will be considered low. Therefore, it is important to focus on the tonometer readings and your well-being. Low blood pressure manifests itself with the following symptoms:
- Dizziness;
- Pale skin;
- Cold sweat;
- Frequent but weak pulse;
- Flashing of flies before the eyes (may accompany hypertension and hypotension).
This is a manifestation of a sharp drop in pressure. When it is constantly reduced, symptoms will not be expressed. In hypotensive patients, a constant feeling of fatigue, drowsiness, and coldness in the fingers and toes comes to the fore.
Diabetic neuropathy leads to orthostatic collapse - a sharp drop in blood pressure when moving from a lying position to a standing position. This is manifested by darkening of the eyes, sometimes short-term fainting. To detect hypotension, blood pressure in diabetes should be measured in the supine and standing positions.
Diet
If previously hypertension aggravated by diabetes mellitus was treated only with antihypertensive drugs, now one of the main interventions is diet therapy. To stabilize blood sugar, it is necessary to limit the consumption of foods with easily digestible carbohydrates. Fatty, fried, smoked and spicy foods should be excluded from the diet. In addition, eating such food can cause gastritis.
The development of hypertension is also associated with the fact that people gradually increase the amount of table salt in their food. It should be remembered that some products already contain hidden salt, so diabetics are prohibited from adding salt to their food. A diet for hypertension should fill the body with microelements and vitamins. The menu contains vegetables and fruits, fish, and vegetable oil in sufficient quantities. It is advisable to eat at least five times a day; portions should be small.
Nutrition for hypotension should be strictly controlled by a nutritionist. On the one hand, a hypotensive person needs high-calorie, filling food, and on the other hand, such foods can increase the blood glucose level in a diabetic.
Why is low blood pressure dangerous in diabetes?
Low blood pressure in diabetes is sometimes more dangerous than high blood pressure. Under normal conditions, a decrease in pressure causes a compensatory spasm, which helps maintain blood supply to the tissues. Due to microangiopathy caused by diabetes, the vessels of the kidneys and microvasculature cannot contract, so the blood supply to all tissues suffers.
Constant oxygen starvation leads to the development and worsening of diabetic encephalopathy, impairs vision and contributes to the formation of trophic ulcers on the extremities. The condition of the kidneys worsens and renal failure develops.
A sharp decrease in blood pressure in type 1 and type 2 diabetes can lead to cardiogenic shock - an urgent condition that requires emergency medical intervention. If signs of low blood pressure appear suddenly, you should call an ambulance to prevent acute renal failure and cardiogenic shock.
Clinical manifestations
The presence of high blood pressure can be determined not only by the tonometer readings, but also by external manifestations:
- Severe, throbbing and squeezing migraine-type headache. It intensifies when the head is tilted down, sometimes there is an acute reaction to light.
- Rapid heartbeat, unstable pulse felt in the ears.
- Increased sweating, release of cold, sticky sweat, causing general chills.
- Decreased vision, dizziness, fainting.
- Nausea, accompanied by bouts of vomiting, which does not bring relief.
- Swelling throughout the body, causing discomfort.
- Numbness of the limbs, tingling sensation in the fingers.
- Chronic fatigue, lack of appetite.
If these symptoms appear more than 3 times a week, it makes sense to get examined, since in 95% of cases they indicate the development of arterial hypertension.
How to increase blood pressure with diabetes?
Do not try to increase your blood pressure on your own without consulting a specialist. Get tested to determine the cause of low blood pressure. If you temporarily cannot get to a doctor, try gentle ways to increase your blood pressure:
- Take 1 tablet of ascorbic acid and 2 tablets of green tea extract;
- Measure 30 drops of ginseng root into a glass of water for a single dose;
- A cup of strong green tea.
Essential oils will help increase blood pressure: bergamot, clove, orange, eucalyptus, lemon, spruce. Add a few drops to an aroma lamp or take a bath with 7-10 drops of ether. Do not use other medications without consulting a doctor. They may be contraindicated in diabetes.
If you suddenly feel weak and dizzy, lie down in bed and raise your legs up. The flow of blood from the lower extremities will increase venous return to the heart and increase blood pressure. Acupressure will help normalize the condition: massage your earlobes with gentle movements for several minutes. The reflex point is the area above the upper lip.
Hypotension requires serious medical prescriptions only if it is a manifestation of heart failure. Then the patient is hospitalized and is given lifelong therapy from combinations of several drugs. Discharge is carried out when the condition is restored and the threat to life goes away.
If hypotension is recorded while taking medications that lower blood pressure, the doctor adjusts the dose of the drugs, but does not cancel them. For hypotension against the background of vegetative-vascular dystonia, tonic drugs (Eleutherococcus) and sedatives are used: Adaptol, Afobazol, Glycine and others. Multivitamin preparations may be prescribed in a course.
The following tips will help increase blood pressure in diabetes of any type:
- Normalize your sleep and wakefulness patterns. Sleep at least 7 hours a day and rest after work. Accustom yourself to a certain schedule: get up and go to bed at the same time.
- Spend enough time walking. This is useful both for lowering blood sugar and for increasing body tone. Accustom yourself to morning exercises - physical activity trains blood vessels and is useful for any pathology.
- Drink enough water.
- Do light exercises with your fingers and toes, massage your limbs to eliminate blood stagnation and normalize blood circulation.
- Take a contrast shower every morning.
- Avoid stuffy rooms and sudden temperature changes.
- Eat well, in small portions, but often. This is important both for maintaining normal blood sugar and for normalizing blood pressure.
Low pressure
It is just as important to increase low blood pressure as it is to lower high blood pressure. When a diabetic's blood pressure drops, the blood supply to the cells slows down, and if the blood vessels are damaged, it may be absent in some parts of the body. This causes serious complications that can lead to disability. You should monitor your blood pressure as often as you should test your blood sugar.
Why does the pressure drop?
If a person experiences chronic fatigue, hypotension develops. In the same way, the level of pressure is influenced by the mental state. Blood pressure is lowered by prolonged depression and frequent stressful situations. In addition, hypotension against the background of diabetes develops due to the following factors:
- avitaminosis;
- sleep disturbance;
- inflammation of the pancreas;
- VSD;
- congenital pathologies of the nervous system;
- prolonged use of potent drugs;
- heart disease;
- weak vascular tone;
- acute phase of gastric ulcer;
- climate change, sudden change in weather conditions. Here is the Online Casino Champion, the best Runet casino in 2020. This is where the biggest winnings await you. And an exciting game. If you love the game of chance, run to the Casino Champion!
Hypotension against the background of diabetes develops as a result of an incorrect lifestyle, so it will not be possible to eliminate the pathology only with the help of medications.
Manifestations
Low blood pressure, as well as hypertension, develops without pronounced symptoms. In this case, the patient may notice the following signs of pathology:
- rare pulse;
- general weakness, drowsiness;
- hard breath;
- hypothermia of the extremities;
- increased sweating;
- changes in well-being depending on weather conditions.
Return to contents
How to increase?
Treatment of low blood pressure should be under the supervision of an endocrinologist. To normalize the condition, first of all, you should adjust your lifestyle; you should not rush to take pills that lower blood pressure without a doctor’s prescription. Medicines for hypotension can increase blood pressure for a short time. To do this, use an infusion of eleutherococcus or ginseng root. In general, changes in pressure levels depend on the general condition of the body. For hypotension due to diabetes, it is recommended:
- have a good rest;
- eat a balanced diet;
- take vitamins;
- drink plenty of fluids;
- take a contrast shower in the morning;
- do a professional massage of the limbs and the entire torso.
Return to contents
Diagnosis of hypotension and hypertension
The diagnosis of hypertension or hypotension is made if incorrect pressure numbers were recorded three times within 2-3 weeks at approximately the same time of day. This rule applies to everyone.
Considering the danger of arterial hypertension in diabetes mellitus types 1 and 2, doctors resort to a more reliable diagnostic method - daily blood pressure monitoring. The method makes it possible to identify incipient hypertension and hypotension and determine disturbances in the daily rhythm of blood pressure fluctuations.
A special device is attached to the patient’s body with which he goes about his usual activities throughout the day. The pressure is measured approximately every hour, and some devices are equipped with sensitivity sensors that record changes in numbers. The doctor receives reliable information and has the opportunity to detect hypertension early, prescribe antihypertensive treatment, and determine the correct time to take medications.
Beta blockers
These drugs block beta-adrenergic receptors, preventing catecholamines from affecting cardiac activity. As a result, the number of myocardial contractions decreases. Prescribed to the patient for increased heart contractions and cardiac arrhythmias.
There are two groups:
- non-selective - affects all tissues in the body;
- selective - affect exclusively the receptors of the heart and blood vessels.
Non-selective beta blockers are contraindicated for diabetics as they increase blood sugar levels. Selective drugs are prescribed if high blood pressure and diabetes mellitus are combined with other diseases: heart failure, heart attack, ischemia.
Such drugs are often used along with diuretics. Blockers cannot be used to treat high blood pressure in patients with asthma.
Antihypertensive drugs for diabetes mellitus should be selected by a doctor.
Prevention of pressure changes in diabetes
A diagnosis of type 1 or type 2 diabetes is not a death sentence. People live with these pathologies for many years, the main thing is to take control of the condition and take a comprehensive approach to health. The first and most important thing is constant hypoglycemic therapy. The goal of treatment is to normalize blood sugar. Her achievement indicates that the doctor has selected the optimal dose of the glucose-lowering drug, which should continue to be taken.
The body changes and diabetes can progress under the influence of endogenous and exogenous factors. Regular monitoring by an endocrinologist, taking tests, and independently measuring blood sugar are mandatory measures for diabetes, which can be life-threatening if ignored.
The next stage is following a diet. Excluding easily digestible carbohydrates is the most important step, without which hypoglycemic treatment will not be effective. The doctor and the patient participate in the development of dietary nutrition. Do not be afraid to carefully ask your endocrinologist about the prohibitions for type 1 and type 2 diabetes. Ask your doctor to tell you in detail what you can eat if you have this disease without fear of increasing your blood sugar.
The third fundamental point is regular physical activity. Muscle work requires glucose and allows you to lower blood sugar and reduce the dose of medications. Physical activity during diabetes trains blood vessels and improves their elasticity.
Reduced blood pressure is not a contraindication for prescribing small doses of ACE inhibitors to prevent kidney damage in microalbuminuria. A quarter of a tablet of enalapril per day will not lead to collapse, but the kidneys will already be protected from diabetes. Do not start taking ACE inhibitors on your own - consult your doctor.
By following your doctor's prescriptions, you will achieve normal blood sugar and delay the onset of the usual complications of diabetes for a long time. Hypotension and hypertension in type 1 and type 2 diabetes occur very often, and their complications are equally life-threatening. Therefore, measuring blood pressure should become a habit of a diabetic patient.
Prevention and recommendations
A passive lifestyle, bad habits and poor nutrition provoke the development of hypertension and type 2 diabetes (type 1 is hereditary). To prevent excess body weight, it is necessary to perform exercises, engage in workload and follow a diet.
The effect of high blood pressure and hyperglycemia has long been studied and adequate treatment has been found. Doctors are confident that by taking medications, limiting diet and using traditional medicine, the manifestation of the disease and its consequences can be reduced to zero.
Why does the body need sugar and its blood levels?
Maintaining vital functions requires the presence of sugar in the food system, and in a certain amount. The product, when consumed in moderation, reduces the likelihood of atherosclerosis, thrombosis and arthritis, and stimulates the functions of the spleen and liver.
Sugar in the body is present in the form of a monosaccharide - glucose, which participates in all metabolic processes, playing the role of an energy supplier. Sugar levels, or more correctly, indicators of glucose concentration in the blood, are called glycemia. Accordingly, an excess of the normal level is hyperglycemia, a decrease in concentration below the norm is hypoglycemia.
A temporary drop in blood sugar can be caused by:
- diseases in acute and chronic form;
- physical or nervous stress;
- food low in carbohydrates;
- significant dietary disturbances.
As a result of hypoglycemia, a deterioration in well-being occurs, including loss of consciousness and coma. Constant relapses indicate a disruption in the functioning of the kidneys, adrenal glands, hypothalamus, and pancreas.
A one-time excess of sugar levels (hyperglycemia) may be associated with increased stress, including emotional stress, abuse of sweets and be temporary. To a mild degree, such deviations are not dangerous and pass quickly. Repeated diagnosis of excess glucose concentration in the blood indicates the presence of an endocrine disease:
- diabetes;
- hyperfunction of the thyroid gland;
- hypothalamic dysfunction;
- malfunction of the liver and pituitary gland.
In this case, hyperglycemia leads to metabolic disorders, decreased immunity, damage to blood vessels and tissues, internal organs, and death.
A blood test is performed to determine the concentration of glucose in the blood. The result is expressed in units: mol/l. The standards depend on the method of blood sampling, are determined by the patient’s age, and are also related to food intake. When taking material on an empty stomach from a finger (capillary blood) in an adult, the norm is considered to be an interval from 3.2 to 5.5 (mmol/l). If an analysis is taken from a vein, the upper limit moves to 6.2 mmol/l.
For elderly and elderly patients, the norm of the lower and upper limits is slightly higher (by about 1 mmol/l).
For newborn babies in the first month of life, the standard is: 2.8-4.4 mmol/l, and for children under 14 years of age it ranges from 3.3 to 5.6 mmol/l.
If the test result taken on an empty stomach is more than 7 mmol/l, the sample is repeated the next day. If high blood sugar levels are confirmed, the patient is at risk for diabetes. He is prescribed a test for glycated (glycosylated) hemoglobin to clarify the diagnosis.
Complications
Complications from the combination of diabetes and hypertension increase the risk of disability and death in 80% of patients. Such complications are mainly caused by disturbances in the functioning of the vascular system. To reduce the risk of developing pathology, the attending physician’s task is not only to stabilize metabolism, but also to constantly monitor blood pressure.
Among the complications, diabetic kidney damage is the most common. This is a pathology of the vessels supplying these organs. Diffuse or nodular atherosclerotic changes appear, which leads to severe renal failure.
In diabetes, hyperkalemia causes disturbances in the functioning of the neuromuscular system and the peripheral circulatory system. Muscle weakness, paresthesia, flaccid paralysis of the arms and legs, diabetic foot, and gangrene occur.
The risk of atherosclerosis, coronary disease, heart failure increases, and heart attack and stroke develop 3 times more often. Damage to the blood vessels of the brain and retina leads to deterioration of vision and absolute blindness.