What it is?
Atherosclerosis is a chronic disease that can be asymptomatic for a long time without bothering a person.
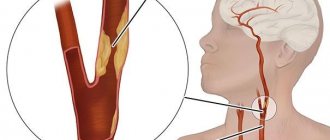
It is characterized by gradual damage to the arteries and various blood vessels of the body. With atherosclerosis, various low-density lipoproteins, cholesterol and other fatty deposits begin to accumulate on the walls of blood vessels in the form of plaques. Reference! The gradual increase in plaque on the walls of blood vessels leads to their dysfunction, loss of elasticity and, consequently, to narrowing.
Vasoconstriction causes deterioration in blood circulation and saturation of various organs with nutrients. Further blockage of blood vessels can lead to thrombosis and complete obstruction, ischemic damage to organs, even death. The main thing is to know well the risk factors, causes and consequences of the disease.
Screening differences
The methods presented will help you get tested safely and provide the doctor with information about the condition of the blood vessels.
Atherosclerosis of the extremities
External differential signs of obliterating blockage of blood vessels in the legs are: pain when walking, weakening of the pulse, pallor of the skin. The disease can be distinguished by raising the foot. When raised, the foot turns pale; when lowered, the pallor disappears.
- The ABI (ankle-brachial coefficient) is determined - the ratio of systolic pressure on the arteries of the shoulder and lower leg. The pressure on the brachial artery is higher, but if it’s the other way around, the patient is likely to have damage to the blood vessels in the legs.
- Duplex scanning of the vessels of the lower extremities will help determine the disease, based on the combination of two modes of an ultrasound machine: Doppler and B-mode. In the first case, the blood flow velocity is determined by designing a flow cartogram. B-mode is based on the construction of a two-dimensional model of the organ under study.
- Digital subtraction angiography is an invasive examination method that involves a puncture with the introduction of a catheter with a special substance. The method allows you to recognize places of blockage. Hagiography is performed more often on the eve of surgery and gives a complete picture of the sites of occlusion.
If the diagnosis is made late, the patient will be forced to take medications for life and undergo antiplatelet therapy. Contact your doctor promptly!
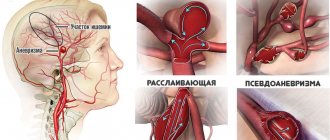
Atherosclerosis of the brain
For blockage of the brain, the clinical picture is: the patient complains of memory impairment, headache, spots before the eyes. The listed symptoms indicate a violation of cerebral circulation. A dangerous consequence can be oxygen starvation of the brain, vegetative-vascular dystonia, and stroke.
To screen for blockage of the great vessels of the brain, studies are carried out:
- duplex scanning;
- ultrasound of cerebral vessels;
- encephalography is a non-invasive method that gives an idea of the bioelectrical activity of the brain with decoding;
- angiography.
Modern high-precision methods make it possible to construct two-dimensional and three-dimensional images of organs and determine the degree of blockage in vascular atherosclerosis.
The first signs of atherosclerosis
The danger of atherosclerosis lies in the fact that the disease develops throughout life and can only manifest itself in old age or during a random examination by a doctor. In the initial stages, it is very difficult to recognize atherosclerosis; usually people do not pay attention to the first alarm bells of the body.
Plaque and plaques gradually grow inside the vessels and narrow the lumen; the first symptoms begin to appear only when the vessel is already half blocked, so it is important to periodically go for preventive examinations.
The initial signs of atherosclerosis include:
- With atherosclerosis of the heart vessels, the first signs are various pain sensations in the chest, abdomen or behind the sternum. A person feels discomfort, manifested by pressing or burning pain, suffers from shortness of breath, angina pectoris.
- With cerebral atherosclerosis, headaches and dizziness appear first. The patient feels constant fatigue, suffers from insomnia or, on the contrary, drowsiness. Tinnitus may be present.
- Atherosclerosis of the extremities can be recognized during prolonged walking or manual work.
- the skin becomes covered with goosebumps;
- limbs often become numb;
- the skin turns pale;
- calf muscles hurt;
- wounds or injuries received are difficult to heal;
- the person may begin to limp;
- limbs are constantly cold because blood circulation is impaired.
- With atherosclerosis of the renal arteries, hypertension begins to develop. Urine tests showed increased levels of protein and red blood cells.
Initial diagnostic methods
How to find out if there is vascular atherosclerosis?
The first suspicions should be prompted by the presence of the above factors. The disease develops asymptomatically; characteristic symptoms appear in cases where, under the influence of atherosclerosis, disturbances in the blood supply to organs and tissues occur in the body.
Depending on the degree of progression of the pathology in the body, various complications may develop that affect the functioning of different organs and their systems. For this reason, the appearance of characteristic symptoms depends on which organ is affected by atherosclerosis and how much the pathology progresses.
The appearance of symptoms characterizing circulatory disorders requires special diagnostics in order to identify the pathology and the degree of its development.
Symptoms characteristic of vascular damage and circulatory disorders are:
- Frequent headaches, tinnitus, dizziness, unsteadiness of gait.
- Pale skin, especially extremities, frequent chills or chilliness.
- Low or high blood pressure.
- Heaviness in the legs, periodic difficulties when walking, tendency to swelling.
- Pain behind the sternum, interruptions in heart function, shortness of breath.
Fainting, decreased performance, apathy and constant fatigue may be a concern.
The clinical picture of atherosclerosis is very diverse and depends on the degree of development of the pathology and the location of vascular damage.
The most common “target organs” are:
- brain and carotid arteries;
- heart;
- kidneys;
- lower limbs;
- aorta;
- mesenteric vessels (in the abdominal cavity).
But remembering the asymptomatic onset of the disease, it is better not to wait for a detailed clinical picture to appear, but to conduct regular preventive examinations.
There is an easy way to conduct a starting diagnostic test at home. To do this, in a horizontal position, you need to measure blood pressure on the shoulder, as usual, and in the ankle area (even better, take several measurements and average the values).
The ankle-brachial index should then be calculated by dividing the systolic pressure at the ankle by that at the shoulder. If the result is within 0.9-1.45, there is no reason to worry, but if the index is below normal, you should not postpone your visit to the doctor.
Expert opinion
Guseva Yulia Alexandrova
Specialized endocrinologist
This method quite accurately allows you to determine the risks of developing cardiovascular diseases even in the absence of any complaints.
Symptoms of various types of disease
In order to consider the signs and symptoms, you need to know what types of atherosclerosis are divided into.
It happens:
- Atherosclerosis of the heart vessels.
- Cerebral atherosclerosis.
- Atherosclerosis of the renal arteries.
- Upper and lower extremities.
- Abdominal aorta.
Heart
One of the most common types of atherosclerosis is cardiac . It manifests itself with symptoms such as:
- Pain in the heart area of various types: pressing, dull or burning. The pain may radiate to the forearm, shoulder blade or arm.
- Instability of blood pressure causes angina attacks.
- Dyspnea.
- Weakness in arms and legs.
- Pain in the back or, conversely, in the ears, jaw and neck.
- Poor blood supply causes cold extremities.
- Sweating.
- Various heart rhythm disturbances.
- Goosebumps and chills.
- Various disorders of consciousness.
- Nausea.
- Increase in blood pressure.
- There may be problems swallowing food.
- Gray hair may appear.
Cerebral vessels of the brain
Signs of cerebral atherosclerosis include:
Pain of a bursting nature throughout the head, without clear localization.- Noise in ears.
- The patient suffers from insomnia or, conversely, increased sleepiness, especially during the daytime.
- The person becomes aggressive, irritable, and nervous.
- Feeling of constant anxiety.
- The function of eating is impaired, the patient chokes on food.
- Slurred speech.
- Fatigue and decreased performance.
- There may be loss of orientation in space.
Read here how to treat atherosclerosis of cerebral vessels, and also how to deal with the disease - follow the link. The article will tell you how to treat the disease.
Expert opinion
Zemlyanukhina Tatyana Vyacheslavovna
Ambulance and emergency paramedic at the Clinical Emergency Hospital #7 in Volgograd.
Ask an expert
Atherosclerosis may be accompanied by “vascular psychoses”. In the early stages of the disease, symptoms may be minor - headache, dizziness, memory impairment. In the future, personality changes may be observed - aggression, short temper, tearfulness, the patient becomes clumsy, productivity and mental adaptation decrease.
Renal arteries
The signs here are as follows:
- Hypertension.
- The appearance of protein in the urine.
- Pain in the abdomen or lower back, radiating to the groin area.
- Blood in urine.
- Low potassium levels in the blood.
- Kidney failure.
Upper and lower limbs
Signs of this type of atherosclerosis:
- Upper limbs:
- Rapid hand fatigue during physical activity.
- Cramps.
- Pain and aches in the hands.
- The skin turns pale, the vascular network is clearly visible.
- Numbness of fingers.
- Hands are constantly cold.
- Heaviness in the hands.
- The hairline is thinning.
- Thickening of the nail plate occurs.
- The pulse is difficult to palpate.
- Wounds do not heal well and can form ulcers.
- Lower limbs:
- The patient begins to limp.
- Legs go numb, extremities are cold.
- Chills and goosebumps.
- Various cramps.
- Pain, especially when walking or playing sports.
- Pale skin.
- Thrombosis.
- The hairline becomes thinner.
- The wounds heal poorly and ulcers form; in advanced stages, necrosis of the foot tissue is possible.
Abdominal aorta
Pain in the abdomen or near the navel, worse after eating.- Various digestive disorders include symptoms:
- constipation;
- diarrhea;
- bloating.
- Anorexia.
- Lethargy and fatigue of the patient.
- Angina pectoris.
- Genital dysfunction in men.
- In some cases, malfunctions in the lower extremities and pelvis may occur.
- It is impossible to determine the pulse under the knee, or in the navel area.
- Thrombosis, which can lead to inflammation of the abdominal organs.
Abdominal
Characteristic symptoms manifest themselves as follows:
- severe and moderate pain in the abdominal cavity;
- pain when eating;
- intestinal dysfunction;
- weight loss.
Atherosclerosis: how to diagnose the problem
Many people do not even suspect that they have atherosclerosis in its early stages, since the symptoms of the pathology may be nonspecific or absent altogether. To identify the disease, a comprehensive diagnosis is required, including:
- identification of risk factors for the development of atherosclerosis;
- determination of specific symptoms of pathology;
- laboratory research;
- instrumental diagnostics.
An integrated approach makes it possible to identify atherosclerosis even in asymptomatic cases.
Risk factor analysis
Factors contributing to the development of atherosclerotic lesions have not been fully studied. The predominant ones are:
- chronic stress;
- abuse of foods rich in animal fat and refined carbohydrates;
- smoking;
- endocrine diseases (diabetes mellitus, hypothyroidism);
- uncontrolled arterial hypertension;
- obesity;
- hereditary predisposition to early atherosclerosis;
- physical inactivity;
- dyslipidemia (increased total cholesterol, low-density cholesterol and decreased high-density cholesterol).
Each of these factors, and their combination, accelerates the development of atherosclerotic lesions, regardless of the patient’s age. If one or more factors are detected, the patient should be referred for additional laboratory testing.
Analysis of the clinical picture
After determining the risk factors for the development of the disease, an analysis of the clinical picture of the disease is required to determine the most likely location of atherosclerosis. Symptoms of atherosclerosis may vary depending on the location of the vascular lesion and the severity of occlusion of the arterial bed. Since atherosclerosis is a generalized pathology, absolutely all arteries in the body can suffer.
Symptoms of atherosclerotic lesions depending on the location of the pathology:
- damage to the blood vessels of the brain is expressed by the appearance of symptoms such as memory impairment, hearing loss, and noise in the head;
- the main symptom of atherosclerosis of the lower extremities is the presence of intermittent claudication;
- atherosclerosis of the coronary vessels is clinically expressed by the phenomena of angina pectoris. The patient experiences pain during physical activity in the heart area, shortness of breath, and rapid heartbeat. The pain goes away after taking nitroglycerin or after a long period of rest;
- Damage to the renal arteries is manifested by a decrease in renal filtration and symptoms of impaired renal filtration capacity. Protein and red blood cells are detected in the urine, and the level of cylinders is increased. Using a phonendoscope, you can identify a specific noise over the area of narrowing of the renal artery. This type of atherosclerosis should be suspected in young people with persistent (refractory) arterial hypertension;
- for atherosclerosis of the carotid arteries, the appearance of dizziness and the same symptoms that are characteristic of damage to the vessels of the head are typical;
- atherosclerotic lesions of the aorta have a long latent period. A clear clinical picture appears only at the age of approximately 60 years. One of the most striking symptoms of aortic damage is an increase in systolic and pulse vascular pressure with a decreased diastolic;
- atherosclerosis of the mesenteric arteries is manifested by the appearance of symptoms of “abdominal toad” and disruption of the digestive processes. “Gastroenteric toad” is characterized by sharp, paroxysmal pain in the upper abdomen after a heavy meal. The pain can last for several hours and is relieved by taking nitroglycerin. The pain may be accompanied by bloating, belching, and constipation. As the disease progresses, profuse diarrhea with remnants of undigested fatty food occurs. Auscultation can reveal decreased peristalsis and systolic murmur in the vessels of the upper abdomen.
Have your blood vessels checked by specialists: which doctor should you contact?
It all depends on where the disease develops and which organs and systems of the body it affects.
- If the coronary arteries are damaged, coronary heart disease will develop, and here your treatment will be handled by a cardiologist. He is your ally even if you have aortic atherosclerosis.
- If the disease has affected the brain and the arteries that supply it, you need to consult a neurologist. If necessary, he will refer you to a consultation with an angiologist.
- When the disease reaches the lower extremities, obliterating endarteritis may develop. You need to see an angiosurgeon.
- Atherosclerosis of the arteries of the abdominal cavity, the so-called mesenteric arteries, will be treated by a surgeon.
Important! Atherosclerosis of the mesenteric arteries can lead to a serious complication - thrombosis with necrosis of a section of the intestine. - Atherosclerotic stenosis, or disease-related thrombosis of the renal arteries, is manifested by high and often drug-resistant arterial hypertension. In this case, treatment is carried out by a nephrologist together with a cardiologist.
Of course, if you have any symptoms, it’s still better to start by visiting a therapist or family doctor . He will collect anamnesis, prescribe the necessary tests and refer you to the right specialist.
Analysis of main risks
Everyone who is at risk needs to know how to check for vascular atherosclerosis. Predisposing factors to the development of the disease are as follows:
- hereditary disposition;
- smoking and alcohol addiction;
- arterial hypertension;
- prolonged stress;
- excess weight;
- insufficient physical activity;
- endocrine pathologies.
The likelihood of vascular pathologies increases significantly under the influence of a combination of several factors. Not everyone knows that atherosclerosis tends to appear at a young age. An unhealthy lifestyle contributes to this. Regular preventative visits to the doctor are necessary, even if the patient’s health is excellent.
The next stage of diagnosis is analysis of the clinical picture. It allows you to determine the local location and severity of vascular pathologies. Symptoms, depending on the nature of the disease, are as follows:
- When the renal veins are damaged, blood and protein are found in the urine.
- Atherosclerosis of the aorta manifests itself in increased pulsation of the damaged area.
- With pathological processes in the arteries of the lower extremities, intermittent claudication develops.
- Blockage of blood vessels in the brain is characterized by memory loss, hearing loss and periodic dizziness.
- With severe shortness of breath, heart pain and angina pectoris, tests will show the presence of coronary sclerosis.
Methods for diagnosing atherosclerosis
Differential . This type of diagnosis will help answer an important question: what are you sick with? Differential diagnosis in medicine is a way to check blood vessels for the presence of atherosclerosis, excluding diseases that are not suitable for any facts or symptoms that are possible in the patient, which ultimately helps to make the correct diagnosis. We can say that this is a kind of exclusion method, when from the symptoms you describe, the doctor puts together a picture that is characteristic only of a specific disease.- Laboratory . Since the leading factor in the mechanism of the disease is a disorder of lipoprotein metabolism, this type of diagnosis is aimed at identifying these disorders. As a rule, venous blood is taken, in which the following are determined: total cholesterol, lipoproteins, and serum triglycerides.
- Instrumental . This type of diagnosis uses the achievements of modern medicine. These are research methods such as ultrasound, MRI, computed tomoangiography, TCD, duplex scanning.
Instrumental studies
You can also check for atherosclerotic plaques using hardware. Dopplerography is used for this. It is a type of ultrasound examination.
Using transcranial Doppler sonography, the condition of the common, external and internal carotid arteries and vertebral vessels is examined. This method is classic in the cardiology clinic. They are also trying to penetrate the brain using rheoencephalography. It uses a radiopaque contrast agent to detect turbulent blood flow in the cerebral vessels. If the device notes the presence of atherosclerotic plaques, fibrin accumulations or sclerosis, this indicates a high severity of the process. The diagnosis of vascular atherosclerosis is often confirmed by computer or magnetic resonance imaging, which can clearly determine the degree of narrowing of the vascular lumen. If arms or legs are involved in the pathological process, rheovasography is used.
Tests - why are they prescribed and how do they work?
- Blood tests . A general blood test will not be informative for identifying atherosclerosis. Your doctor may order you to have a blood glucose test to determine if your carbohydrate metabolism is impaired. To do this, you will need venous or capillary blood taken on an empty stomach. Coagulogram – due to the risk of thrombosis, will be useful. Helps evaluate the blood coagulation system. Due to atherosclerosis, inflammation of the vessel wall may be present, and here SRB will come to the rescue. Liver tests and potassium are needed to assess the risk of myocardial infarction and ischemia as a complication. All these tests are taken from a vein, strictly on an empty stomach, and at least 8 hours must pass after dinner.
- Determination of fat metabolism . How to check for fatty deposits in blood vessels? It shows whether fat metabolism is disturbed and how much of it is in the plasma, because an excess will lead to them being deposited on the walls of blood vessels. You will need venous blood taken on an empty stomach. To determine lipid metabolism, you need to test cholesterol, lipoproteins and triglycerides. Based on the examination results, the doctor will be able to calculate the atherogenic index, which will show how high the risk of artery damage is.
- Ankle-brachial index (ABI) . Helps to identify whether there is atherosclerotic vascular damage. To make a diagnosis, pressure is measured in the ankle and arm, and the values are interpreted using a special index. Based on the results, the patency of the arteries can be assessed. Pressure measurement is carried out in a lying position; no additional preparation is required.
- X-ray . Used to diagnose coronary vessels, aorta and pulmonary artery for the presence of atherosclerosis. Examine the chest. Having stripped to the waist and removed all jewelry, the health worker will put you in front of an X-ray machine, after which you need to take a deep breath and hold your breath. There is no need to prepare specially for the examination.
ECG . It will be necessary if the course of atherosclerosis is complicated by ischemic heart disease. Helps to see the work of the heart. The examination is quick, does not cause discomfort and does not require preparation. Using special sensors that are fixed on the wrists, ankles and in the area of the heart, its work is recorded, the result is recorded on a paper tape and requires interpretation by a specialist. An electrocardiogram is performed at rest, lying on the couch. If the patient has exertional angina, then a stress ECG will be needed. In this case, the patient will be asked to pedal a bicycle or run on a treadmill, and the devices will record the work of the heart.- Ultrasound . It is used to assess the patency of blood vessels and the sufficiency of blood flow. Helps to see if blood clots or atherosclerotic plaques have formed. Using a special gel applied to the examined area, visualization of the organ being examined is carried out, the image is displayed on a computer monitor and assessed by a sonologist. As a rule, if the gastrointestinal tract is not affected, no preparation is required.
- Tomography . Thanks to MRI or CT, it is possible to obtain images of the arteries, see the structure and function of large and small vessels. Before the examination, a contrast agent is injected into a vein.
Note: MRI is not always prescribed, as a rule, before surgery or in complex cases related to diagnosis.
What blood test is required?
To determine the presence and stage of development of atherosclerosis, it is necessary to check not only the condition of the blood vessels, but also the composition of the blood . To do this, several types of analyzes are carried out:
- Biochemical analysis - for atherosclerosis, this analysis shows the ratio of lipoproteins of different densities in the blood. It is calculated as follows: the total cholesterol index excluding HDL is divided by the HDL index. An indicator of 2 to 3 is considered normal. The level of triglycerides is also taken into account - no more than 0.14–1.82 mmol/l.
- Cholesterol blood test - this test shows the total cholesterol content, without dividing into “bad” and “good”. The normal content of total cholesterol is from 3.1 to 5.2 mmol/l.
- Coagulogram is a blood test for clotting. Obviously, the higher the coagulability index, the more actively lipid stains will turn into blood clots under the influence of thromboxane.
Sometimes doctors additionally check the erythrocyte sedimentation rate (ESR) - its increase indirectly indicates inflammatory processes in the body (with atherosclerosis - inflammation of the endothelium of the inner surface of blood vessels). With inflammation, the content of fibrinogen in the blood increases, a protein that triggers coagulation mechanisms. Under its influence, red blood cells literally stick together, forming dense lumps that quickly settle to the bottom of the test tube.- A urine cholesterol test can also be used to diagnose atherosclerosis.
Reference! What does urine have to do with blood? In fact, it's straightforward: to simplify slightly, we can say that urine is formed from water and impurities filtered from the blood. Therefore, based on the content of certain substances in the urine (for example, cholesterol), one can draw conclusions about their content in the blood.
Additional biochemical studies
To clarify the diagnosis, additional instrumental studies are used.
- Angiography is the study of blood vessels using x-rays. Since the vessels are not visible on x-ray, the patient is first given a contrast agent intravenously. The advantage of angiography is that it allows you to examine small vessels that are invisible using other methods.
- Ultrasound - Ultrasound is widely used to determine vascular dilation and wall deformation.
- Magnetic resonance imaging - today this method allows you to obtain the most accurate and detailed picture: it can be used to determine the width of the lumen of the vessel, as well as the location and shape of the plaque.
Biochemical basis of treatment
Based on the foregoing, the biochemical basis for the treatment of atherosclerosis is to stop inflammatory processes, remove excess cholesterol from tissues and prevent an increase in its level.
For this purpose, four groups of medications are used in modern medicine:
- Statins are drugs that inhibit the production of cholesterol in the liver and small intestine, thereby helping to reduce its concentration in the blood;
- Fibrates are drugs that accelerate the process of processing and uncoupling of fats;
- Fatty acid sequesters - prevent the absorption of fatty acids from the digestive tract;
- Vitamin PP , also known as nicotinic acid , has proven itself as a means of reducing cholesterol levels by accelerating its processing processes.
And, of course, an important component of treatment is the correction of eating habits (proper nutrition or diet) and physical exercise :
- to reduce the intake of cholesterol into the body, you need to reduce the consumption of animal fats - lard, butter, fatty sour cream, fatty meat (pork, beef);
- in order not to provoke the process of glycolysis of drugs, it is necessary to monitor the level of glucose in the blood - reduce the consumption of sweets, and for people with diabetes or a predisposition to it, regularly check the level of sugar in the blood;
- In order to provide the body with HDL, vegetable fats are needed - there are many of them in nuts and seeds.
Laboratory and instrumental diagnostics of atherosclerosis
Laboratory diagnostics are prescribed to all patients with existing risk factors for the development of the disease, regardless of the presence or absence of symptoms of atherosclerosis. Laboratory diagnostic methods make it possible to draw a conclusion about the general condition of the arterial bed and determine the likelihood of developing atherosclerotic lesions in a particular patient. The most significant laboratory studies are:
- total cholesterol level (TC) - normal 3.1-5.2 mmol/l;
- HDL, or “good cholesterol”, or - the norm is from 1.42 in women and from 1.58 in men;
- LDL, or “bad cholesterol” – the norm is up to 3.9 mmol/l;
- triglycerides – normal 0.14 -1.82 mol/l;
- atherogenic index (ratio of HDL to LDL) – the norm is up to 3.
Also, the determination of the following indicators is diagnostically significant:
- C-reactive protein;
- renal filtration rate;
- creatinine level.
The diagnosis is confirmed instrumentally. The most commonly used:
- Ultrasound of vessels of any location with Doppler determination of blood flow;
- X-ray contrast angiography;
- MRI;
- Ultrasound determination of the thickness of the intima (inner layer) of the vascular wall.
How is it determined?
How to determine cerebral vascular disease atherosclerosis? The difficulty of diagnosis is that it is impossible to make a diagnosis using only one blood test, so the peculiarity of this type of diagnosis is that it requires expensive examinations.
In addition, vascular problems may not have pronounced symptoms, especially at an early stage, or have an atypical development of the disease. The formations are fibrous in nature. So how to diagnose the presence of atherosclerosis in the vessels of the brain? The most commonly used methods involve ultrasound . Your doctor may refer you for a duplex scan, TCD, angiography, MRI or CT scan. Usually they prescribe blood tests for cholesterol and, if it is elevated, a lipid profile.
Arms and lower limbs
Symptoms of upper and lower extremity lesions may be similar to other diseases, making differential diagnosis difficult.
Here, high-tech methods of examining hands will come to the rescue to make an accurate diagnosis. First, the doctor performs a physical examination :
- squeezes the hand to assess the strength of the forearm muscles;
- pressure on the brachial plexus reveals the absence or presence of pain and numbness;
- palpates the subclavian fossa;
- Ultrasound and x-rays are the most informative in this case.
For examination of diseases of the lower extremities, it is prescribed:
- MSCT or MR angiography;
- arteriography;
- Doppler ultrasound;
- ABI study.
The doctor can also feel the pulse in the legs to determine blockage of blood vessels. There are no special tests. As usual, total cholesterol, triglycerides, and lipoproteins are prescribed.
Aorta of the heart
How to identify a disease such as atherosclerosis of the aorta of the heart? It is quite difficult to recognize the disease based only on the patient’s complaints, because at the very beginning the disease can be asymptomatic . To clarify the diagnosis, in addition to the usual laboratory tests, standard for the diagnosis and detection of atherosclerosis, which were described above, the following may be prescribed:
- ECG, ECHO-CG;
- angiography and coronography;
- duplex scanning;
- MRI.
Abdominal aorta
This species masquerades as gastrointestinal diseases, which complicates the correct diagnosis. The following examinations may be prescribed :
- Doppler ultrasound;
- FGDS;
- Ultrasound of the abdominal cavity;
- aortoangiography;
- lipid profile;
- coagulogram.
Manifestations
When contacting a specialist, first of all, the doctor collects anamnesis and interviews the patient. After this, the clinical manifestations of the disease begin to be determined. The pathology is complicated by the fact that at the initial stage even the patient himself does not know that pathological changes have begun in the body. However, there are preclinical manifestations of the disease that indicate dysfunction of organs and systems. The patient notes:
- Pain in the temples, back of the head, stomach and heart. As a rule, such pain occurs due to stressful situations, during strong physical exertion. The patient is not bothered by the condition at all, as it occurs in rare cases and goes away without medication.
- Feeling hot.
- Numbness or redness of the skin of the face.
- Increased sweating during sleep.
- Feeling of goosebumps on the skin.
All preclinical manifestations are not associated with organs or tissues.
Important! To diagnose vascular atherosclerosis, doctors determine the clinical manifestations in a particular organ. Signs depend on which part of the vessel or artery is affected by atherosclerotic plaques.
Brain
Impaired blood circulation in the brain occurs due to blockage of the carotid artery or other large vessels that supply the brain with nutrients and vitamins necessary for life and normal functioning, and this disease is called cerebral atherosclerosis. If the brain does not receive enough substances, the patient is concerned about clinical manifestations:
- Memory declines sharply, the patient cannot remember recent events.
- Migraine that does not go away with painkillers. With the slightest physical exertion, the headache increases.
- Decreased visual acuity, the patient feels stars, flickering in the eyes.
- Insomnia.
- Decreased hearing acuity.
- Loss of consciousness.
- Coordination of movements is impaired.
When the arteries and veins that supply the heart are damaged, the patient is disturbed by the work of the heart and the rhythm is frequent. In addition, ischemia appears, which manifests itself in the following manifestations:
- Feeling of pain and burning in the sternum area.
- Feeling of heaviness.
- The patient has difficulty breathing.
- Angina pectoris.
- Heart rate increases.
Important! Clinical manifestations of damage to the coronary arteries arise not only due to the development and course of the pathology, but also due to an incorrect lifestyle. Atherosclerosis of cerebral vessels leads to stroke, which threatens the patient’s life.
Lower limbs
With pathology of the vessels that deliver blood to the lower extremities, the patient feels unwell. If there is insufficient blood circulation, the patient is concerned about the symptoms described below:
- Pain in the legs, which bothers you not only when moving, but also at rest.
- Numbness.
- Tissue regeneration does not occur at the proper level.
- The local temperature has dropped.
- The pulse in the legs is weak.
Important! With atherosclerosis of the lower extremities, the patient experiences pain in the muscles. Diagnosis of leg lesions involves the use of hardware methods that make it possible to differentiate the disease from other pathologies that have a similar clinical picture.
Biochemistry of atherosclerosis
We need to start with the fact that cholesterol, or more precisely, cholesterol, is a steroid of animal origin, vital for humans .
Steroid hormones (such as testosterone, estrogens, cortisol) are synthesized on the basis of cholesterol; it is part of cell membranes. For the body's needs, cholesterol is synthesized in the liver, small intestine and adrenal cortex in an amount of approximately 1 g; another 300-500 grams come from outside with food. This is quite enough to maintain the normal functioning of the body.
Cholesterol is a substance insoluble in water, and therefore functions in the internal environment consisting of liquids - blood, lymph, etc. it can only in combination with special proteins - lipoproteins, which serve as its “packaging”. Depending on the ratio of cholesterol to protein, lipoproteins are of high, low and very low density (HDL, LDL and VLDL).
Reference! LDL and VLDL deliver cholesterol to tissues, and HDL, on the contrary, absorbs excess cholesterol from tissues. The higher the content of HDL in the blood, the lower the risk of developing atherosclerosis. The level of these substances can be increased by taking estrogen drugs in small doses, or simply by eating a lot of vegetable fats.
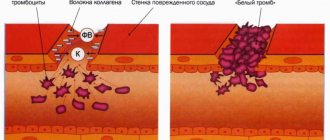
The biochemistry of the development of atherosclerosis looks like this:
- The process begins with weakening of blood vessels, damage and inflammation of the endothelium. It is the inflamed areas of the vascular walls that become the localization sites for future plaques.
- LDL and VLDL accumulate in inflamed areas. There they are modified - they change their structure through glycolysis or oxidation. Glycolization occurs when the level of glucose in the blood increases, oxidation occurs under the influence of so-called inflammatory mediators produced by damaged endothelium.
- Proteins with an altered structure are perceived by the body as foreign, harmful objects, and accordingly, antibodies begin to be produced against them.
Monocytes (a type of leukocyte, cells that absorb foreign particles) begin to actively absorb modified lipoproteins. This process is uncontrollable, and after some time the amount of cholesterol accumulated in the monocyte exceeds its processing capabilities. Monocytes become overfilled with cholesterol and turn into so-called foam cells. These cells settle in the intima (the cellular layer under the endothelium) and accumulate, forming spots and creating a lipid metabolism disorder.- The accumulation of foam cells injures the endothelium. This activates platelets, the cells “responsible” for wound healing. They begin to secrete a special substance - thromboxane, which promotes platelet adhesion. Under normal conditions, such a platelet “plug” closes the wound and prevents blood loss and infection, but inside the vessel it becomes the basis for a fibrous plaque.
- Platelets also secrete a so-called “growth factor” that promotes the proliferation (reproduction) of smooth muscle cells. This mechanism usually helps restore damaged tissue under the clot, but in this situation, the newly formed tissue grows inside the plaque, making it larger and denser.
- Finally, calcification occurs - the plaque is impregnated with calcium salts. The plaque becomes dense and hard, firmly “adhering” to the vascular wall and causing its deformation. At this stage, the plaque has already reached a size sufficient to block most of the lumen of the vessel or completely block it.
To detect the disease in time, learn the symptoms and risk factors, as well as the consequences of atherosclerosis.
We invite you to watch a video that clearly and easily explains the mechanism of atherosclerotic plaque formation:
Methods for checking blood vessels for atherosclerosis
Before determining vascular atherosclerosis of any location, generally accepted studies are prescribed: general analysis, coagulogram, rheumatological blood tests. But to definitively clarify the diagnosis, specific laboratory diagnostics and serious instrumental examination for atherosclerosis are necessary.
Lipidogram
It is an analysis of blood plasma for the content of cholesterol-containing substances, their relationship with each other, as well as the determination of the so-called atherogenic coefficient. It is calculated by the ratio of total cholesterol to “bad” cholesterol - that which is able to penetrate the vascular wall and be deposited in it (low-density lipoprotein). The study most objectively reflects the state of metabolism, primarily fat.
To avoid getting false results, proper preparation for the study is required:
- last meal - no later than 8 hours before blood donation;
- the subject needs to protect himself from nervous and physical stress for 3-4 days, and not radically change his diet;
- Smokers are advised to wait at least 30 minutes without a cigarette before the procedure.
Analysis of lipid metabolism is the first stage in diagnosing vascular problems.
And now a little about the results of a lipid profile of venous blood: the risk of developing atherosclerotic disease increases with increased levels of total cholesterol, low- and very low-density lipoproteins, and triglycerides. The situation is complicated by a decrease in the level of “good” cholesterol compounds that can be excreted from the body - high-density lipoproteins.
What to do if detected?
Atherosclerosis develops over a fairly long period of life, so the main recommendation is prevention and monitoring of blood cholesterol levels. If atherosclerosis is detected at the initial or mild stage, the main thing will be to follow a diet.
- It is necessary to exclude fatty and high-calorie foods from the diet.
- You should avoid alcohol in large quantities, as it causes irreparable harm to the body. You can drink a little wine, it is good for the heart.
- To combat the layering of fatty deposits on the walls of blood vessels, flaxseed and olive oil, or fish oil are well suited.
- You should increase your consumption of cabbage, grains, peppers, apples, carrots and other high-fiber foods. Fiber speeds up the process of ridding the body of cholesterol.
- Fermented milk products that improve the functioning of the digestive system are good.
- Based on your age, you need adequate physical activity, morning exercises or sports, and completely stop smoking.
- It is recommended to reduce body weight if it is excess.
Reference! In more severe stages, drug treatment cannot be avoided. Drugs used in the fight are divided into those that slow down the body's production of cholesterol and those that allow you to quickly remove excess cholesterol.
Use:
- Statins.
- Fibrates.
- Nicotinates.
- Herbal medicines.
- Bile acid sequestrants.
“Surgical treatment is prescribed when the risk of developing disabling complications without surgery exceeds the development of such complications after surgery.” reports the Clinic of High Medical Technologies named after. N.I. Pirogov.
Diagnostic tests for atherosclerosis - CK-MB test
CK-MB is a form of creatine kinase, an enzyme that is found primarily in myocardial cells. It is released into the blood when the heart is damaged. CK-MB is performed when acute coronary syndrome is suspected. Enzyme activity usually increases 3-4 hours after the onset of chest pain. CK-MB values normalize after three days.
The CK-MB study is also used to evaluate the effectiveness of heart attack treatments, as there is a rapid increase and then decrease in CK-MB activity after drug administration. This activity also sometimes increases after intense exercise, in cases of kidney failure, alcohol abuse, and severe skeletal muscle damage.
How the disease develops
In the development of atherosclerosis, two main factors are involved: lipid and vascular.
The development of atherosclerosis occurs gradually and depends on many factors. The following are considered the main ones:
- lipid metabolism disorder – dyslipidemia;
- increased pressure, which contributes to the stratification of the epithelium of the walls of blood vessels, where lipids penetrate;
- obesity;
- diabetes;
- smoking.
These 5 reasons are recognized by the World Health Organization as the main factors contributing to the development of atherosclerosis.
With atherosclerosis, the inner surfaces of blood vessels become coated with cholesterol. Plaques form at the sites of layering, narrowing the bloodstream. The further the process develops, the worse it gets. The layers may come off or rupture, allowing blood clots to form.
In the development of atherosclerosis, two main factors are involved: lipid and vascular.
Doctors consider the beginning of the development of the disease to be an increase in lipid levels in the body. This applies to triglycerides and low-density lipids - LDL. They penetrate the walls of blood vessels and form cholesterol plaques.
The vascular or endothelial theory considers damage to the inner layer of blood vessels as a trigger for the occurrence of atherosclerosis. The formation of cholesterol plaques occurs in places where the vascular walls are damaged.
These two theories have the right to exist, because they complement each other, and do not exclude. What they have in common is the formation of a fatty clot, which slowly increases without showing its presence in the first stages. In total, the plaque has 4 stages of development. On any of them, the clot can be damaged under the influence of increased pressure, come off or burst. Which is fraught with fatal consequences.