Why does the separation occur?
To give an unambiguous answer to the question of why a blood clot breaks off, it is necessary to study a considerable amount of not always unambiguous medical literature.
But in general, the process can be described quite simply.
A blood clot forms in the body, waiting “in the wings.”
Why does a blood clot break off in a person?
- it does not completely block the lumen of the vessel;
- the blood flow is fast enough (to tear the clot away from the wall).
Consequently, in most cases, the clot breaks away from the artery wall.
Then the blood clot moves, perhaps to a fairly large distance. The clot can also divide into several particles, which leads to blockage of several vessels at once.
The symptoms that appear when a blood clot breaks off are determined by the affected area.
Answering the question why blood clots form, we can list several reasons:
- damage to the vessel wall;
- changes in blood quality (thickening);
- disturbance of blood flow speed (slowdown);
- increased coagulability.
The reasons for the formation of blood clots in blood vessels are different, but they are all associated with the presence of certain diseases that affect the blood itself and the condition of the blood vessels:
- vasculitis;
- atherosclerosis;
- malignant neoplasms.
Thrombosis – literally translated from Greek means a clot. Blood clots form inside the blood vessels, which impede the normal flow of blood throughout the circulatory system.
When a blood vessel is damaged, the body begins to release fibrin and platelets, which help form a blood clot to prevent blood loss. There are situations when the vessel is not damaged, but there is a clot, and it can circulate throughout the circulatory system. These clots are called emboli.
Thrombophlebitis is a thrombosis in which the walls of the veins become inflamed and blood clots form, interfering with the normal functioning of the circulatory system.
There are several types of thrombophlebitis:
- Thrombosis affecting superficial veins (varicose veins);
- It can damage the deep vein;
- Thrombophlebitis of the lower legs;
- A disease affecting the portal or vena cava.
Doctors regularly remind that a disease such as thrombosis must be detected in a timely manner, because a thrombus can block the vascular bed, and accordingly, blood circulation is impaired.
Moreover, the clot can break off in one moment and move to any place along with the bloodstream. The location of the blood clot has a direct bearing on symptoms. True, sometimes there are no signs.
The worst complication is the death of the patient.
Why do blood clots appear?
In everyday life, a person often hears the word blood clot, but rarely thinks about what it is, how serious it is and what consequences its formation can lead to.
What can serve as a factor for its formation and how to avoid it? A thrombus is a blood clot that forms on the walls of blood vessels and increases in size over time.
Such a clot interferes with normal blood flow by narrowing the lumen of the vessel or completely blocking it.
Sometimes it can break away from the vessel wall and move along the bloodstream; this condition is called a wandering thrombus.
This is very dangerous, because it is not always possible to diagnose and carry out the necessary treatment in a timely manner, and this can lead to death, death from a blood clot is instantaneous.
In the absence of pathologies on the part of the body, it has a positive protective function, for example, with a minor cut, the blood stops spontaneously due to the formation of a blood clot (thrombus).
Reasons for their formation
Such blood clots can form in all types of human blood vessels; the reasons for their formation are considered to be:
- vessel wall injuries;
- disturbances in blood clotting processes;
- decreased blood flow speed;
- atherosclerosis.
More details:
- Vessels can be damaged as a result of inflammatory processes, under the influence of harmful bacteria and viruses, or due to mechanical trauma (burn, bruise, cut).
- Blood clotting may be impaired by medications taken (chemotherapy). Most often, the cause of this disease is congenital pathologies. Bacteria and viruses can also cause problems.
- A slowdown in blood flow occurs with a violation of the condition of blood vessels (varicose veins, squeezing of a vessel, excessive blood thickness).
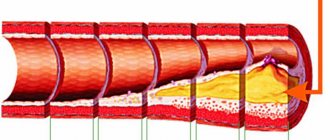
- Atherosclerosis is the accumulation of fats (cholesterol) on the walls of blood vessels, then these accumulations become overgrown with connective tissue and an atherosclerotic plaque is formed. And a blood clot forms on its surface (as a protective reaction of the body to remove the plaque).
People most susceptible to the disease
Persons most susceptible to thrombosis:
- people with excess body weight (obesity);
- women belonging to the age group of 50 years;
- men over 40 years old;
- pregnant women and women who have recently given birth;
- drinking alcohol in large quantities;
- persons leading a sedentary lifestyle;
- patients after surgery (abdominal surgery);
- coffee abusers;
- uncontrolled use of oral contraceptives;
- suffering from cancer.
Symptoms of blood clots
When localized in a vein, symptoms such as pain in the area of thrombosis, increased temperature in this area, hyperemia of the skin, and swelling may occur. If the superficial vein is affected, then it feels compacted to the touch, and palpation causes discomfort and pain.
A blood clot in the head causes symptoms such as loss of coordination, impaired swallowing reflex, paralysis of the limbs, and speech defects. When it is torn off, a stroke develops.
The veins supplying blood to the brain, when damaged, can exhibit clinical manifestations such as blurred vision, frequent headaches, and noise in the ears or head.
Blood clots and intestines
Arterial thrombosis of mesenteric vessels is not uncommon in patients with atherosclerosis. In this case, against the background of characteristic changes in the vascular wall in the form of fibrous plaques with rupture, atheromatosis, local hypercoagulation occurs, and the lumen of the vessel or the mouth is blocked by a thrombus. The first symptoms will be abdominal pain, vomiting, diarrhea, then, as necrosis of the intestinal wall develops, symptoms of intoxication will increase, and peritonitis is possible. Without timely surgery, such changes inevitably lead to death.
Separately, it is necessary to say about such a dangerous condition as thromboembolic syndrome. The source of thrombosis in this case can be the veins of the legs, pelvis, affected heart valves or parietal endocardium.
Symptoms of a blood clot rupture will be reduced to signs of damage to the organ in whose vessels the thromboembolism has stopped. This may be acute pulmonary heart failure with shortness of breath, cough, arrhythmias up to respiratory and circulatory arrest, signs of stroke, myocardial infarction, renal failure or intestinal necrosis.
Mechanism of blood clot formation
Blood clots - what are they? Understanding why blood clots form in blood vessels means preventing the development of such a dangerous disease as thrombosis and preventing serious consequences. The formation of blood clots is associated with damage to the inner surface of the vascular wall under the influence of various negative factors.
The result is an altered state of the endothelium, which gives a signal to the body, and large amounts of a substance that promotes the gluing of blood cells are released into the blood. This substance is interleukin.
Shows what contributes to the formation of blood clots, a diagram depicting the body's response to a violation of the integrity of large and small blood vessels. Platelets and fibrin contribute to the formation of a clot, which prevents blood from flowing freely through the vascular bed.
Without it, it is impossible to stop bleeding, but increased formation of blood clots leads to vascular thrombosis developing in the human body. This is a disease caused by intravital blood clotting in the lumen of veins, arteries or capillaries, as well as in the cardiac cavities.
When studying the features of the disease called thrombosis, the causes of its occurrence and the mechanism of development, attention should be paid to the process of blood clot formation, which looks like this:
- At the site of damage to the vascular wall, the production of substances that are responsible for normal blood clotting slows down.
- Platelets break down, and as a result of the release of thromboplastin and thrombin into the blood, the level of blood viscosity increases significantly.
- The result of the formation of prothrombinase is the transition of inactive prothrombin to active thrombin, from which a specific protein is formed - fibrin. Its fibers do not stick together, but intertwine to form a mesh, which serves as a kind of frame for the future blood clot.
- Cells settle on this mesh during the process of agglutination of blood proteins.
- Fibrin threads are pulled together by platelets, and the resulting clot is separated from the blood serum, becomes denser and reliably closes the damaged area of the vascular wall.
Considering the causes of thrombosis, we can say that during the pathological process, a growing dense clot partially or even completely blocks the bloodstream. Having established itself after its appearance in the area of the vascular valve, the thrombus gradually increases in size, preventing the free flow of blood.
If after some time an inflammatory process begins, leading to the appearance of adhesions between the thrombus body and the vessel wall, then the risk that a dense, non-absorbable clot may come off becomes minimal.
The absence of adhesions or inferiority causes the detached blood clot to completely block the lumen of the vessel, block it, and the person dies.
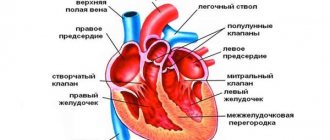
Blood clots in the heart and coronary arteries
The classic manifestation of coronary thrombosis against the background of atherosclerotic lesions is coronary heart disease. If the clot does not completely block the lumen of the artery, then chronic ischemic heart disease develops in the form of angina pectoris with heart pain and shortness of breath. If the lumen of the vessel is completely closed, a heart attack will develop: blood will not move through the affected artery and the area of the heart muscle will undergo necrosis (death).
The symptoms of myocardial infarction are familiar to many: intense pain in the heart area, shortness of breath, a feeling of fear of death, cyanosis, cardiac arrhythmias, and others.
A blood clot in the heart can be located both on the inner walls of its chambers and on the valve flaps. During various inflammatory processes (endocarditis), atherosclerotic lesions, damage occurs to the inner lining of the heart - the endocardium, which inevitably leads to activation of the blood coagulation system and thrombus formation. The presence of a foreign body in the form of an artificial valve also triggers such mechanisms.
Intracardiac thrombosis is dangerous not only by the development of acute or chronic heart failure, but also by the so-called thromboembolic syndrome, when detached clots rush into the systemic circulation, settling in the vessels of the brain, kidneys, spleen, intestines and causing necrotic changes in them.
Causes of blood clots
There are three main reasons why a blood clot forms and, in many cases, breaks off:
- Damage to the vessel wall (mechanical trauma, inflammatory processes, damage to the inner wall by bacteria, toxins, viruses);
- Improper functioning of the blood clotting function (activation of coagulants and provoking platelet aggregation - joining to each other). This process is mainly associated with congenital abnormalities in the development of platelets, although sometimes changes occur at the chemical level (after exposure to bacterial, viral cells, taking certain medications);
- Slowing of blood circulation (associated with compression of arteries and veins, varicose veins, increased blood density).
Blood clots can form in any part of the circulatory system - in veins, arteries and even in the heart. The above reasons are applicable in every case.
However, there are also specific factors that affect only a certain part of the circulatory system.
admin page » Blood clots 20753(64.17 out of 5)Loading…
What is a blood clot? What causes blood clots?
But sometimes a blood clot forms in the chambers of the heart or blood vessels, which gets stuck in one place, blocking the path to normal blood supply. We recommend that you learn more about blood clots in the left ventricle of the heart.
How does a blood clot form?
The heart is a powerful motor for pumping blood along 100 thousand km (2.5 times the length of the Earth’s equator!) of large and small human blood vessels. This clot is a thrombus. It can grow and completely block the blood path to individual organs and tissues.
And sometimes it breaks off (thromboembolus) and begins its journey through the body. And this is already completely dangerous: at any moment it can clog an important vessel and lead to death.
Let's look at why blood clots form and how to avoid it.
Types and mechanisms of blood clot formation
The classification of blood clots depends on its purpose.
According to their structure, blood clots are:
- white (platelet) blood clots form slowly in capillaries and arteries when blood flows quickly;
- red (blood fibrin) blood clots quickly form mainly in the veins with slow blood flow and an increased level of blood clotting;
- mixed (layered), red and white thrombi, formed in the cavity of the aortic and cardiac aneurysm or in the veins;
- hyaline blood clots form in small vessels of various organs (gastrointestinal tract, urinary system, brain, lungs, etc.) usually due to the fact that there is more plasma in the capillaries than whole blood.
Blood clots are classified according to size and type:
- parietal thrombus - “smeared” along the wall of the vessel (usually in chronic heart failure - on the heart valves, in atherosclerosis - on large arteries, in inflammation - on veins, in aneurysms - in the heart and blood vessels) and covering no more than 50% of its diameter;
- clogging thrombus - blocking the lumen of blood vessels (usually in veins and small arteries, less often in the aorta and large arteries) over 50%, seriously interfering with blood flow, usually as a result of the proliferation of wall thrombi;
- progressive thrombus - a rapidly growing thrombus along the bloodstream, capturing the walls of the veins and reaching the collecting venous vessels;
- spherical thrombus - a growing thrombus of the left atrium with a high risk of breaking away from the inner wall of the heart;
- a dilated thrombus can form in the cavity of an aneurysm (the vessel wall is stretched more than 2 times), so it grows to a large size and can break off, completely blocking the blood flow.
The symptoms that should alert you are specific to the different locations of the blood clots.
The formation of blood clots is a protective reaction of the body aimed at stopping bleeding.
Everyone knows that with small cuts, the blood stops quite quickly, and this happens due to the closure of damaged capillaries with small blood clots.
The cause of 40% of sudden deaths is a detached blood clot. And this is quite scary.
Probably every person has heard about blood clots and thrombosis, but not everyone understands how dangerous this can be.
It is the blood clot that is responsible for the development of such fatal diseases as myocardial infarction and ischemic stroke.
Also, due to the formation of blood clots, gangrene can develop, and if it comes off, pulmonary embolism can occur.
Thrombus, what is a thrombus
Very often in the media you can hear that it was a blood clot that caused the death of one or another popular artist or director.
At first glance, there is nothing scary about this word, but many people wonder why it could be dangerous. So what is a blood clot?
A thrombus is a blood clot that forms in a blood vessel or cavity of the heart. It consists of proteins, mainly fibrin, and can be parietal or occlusive, i.e.
completely closing the lumen of the vessel. Occlusion thrombi most often form in small vessels, while parietal thrombi form in large veins of the lower extremities and the cavity of the heart.
Education, treatment, causes, prevention of blood clots
The formation of blood clots is a protective reaction of the body aimed at stopping bleeding.
- Infections;
- Acquired or hereditary tendency of the blood flow to form clots;
- Slow blood flow;
- Reduced reactivity of the body;
- Due to violations of the vessel wall;
- Due to changes in blood composition;
- Due to surgery;
- Due to cancer;
- Due to kidney problems.
The detachment of a blood clot is a dangerous condition, fraught with numerous complications from the cardiovascular, central nervous system and even death of a person.
Normally, the rheological properties of blood and its clotting to stop bleeding are regulated by a number of factors.
These are the formed elements platelets, proteins, biologically active substances that are produced in the liver.
In a healthy person, the coagulation system is activated by any, even minor, damage to the vessel.
Stopping bleeding and blood clot formation occurs in several stages. At the beginning, platelet adhesion, in other words, their adherence to the vessel wall.
This mechanism is provided by substances that are released during injury. Then platelet aggregation, that is, the formation of a clot from the accumulation of a large number of these formed elements.
During the first phase, some cells are destroyed, releasing certain substances. Under their influence, the blood coagulation system is activated, that is, thin fibrin threads are attached to the clot.
Normally, with the restoration of the integrity of the vascular wall, the thrombus also dissolves. However, in the presence of certain predisposing factors, formed elements (erythrocytes and leukocytes) and other proteins settle on the resulting accumulation of platelets and fibrin.
A disorder of the hemostasis system, which leads to increased blood clotting, is called thrombophilia.
Experts call a disease accompanied by the formation of blood clots of various locations thrombosis, and the separation of a blood clot followed by complete or partial blockage of the lumen of a blood vessel is thromboembolism.
Thrombogenic risk factors can be permanent, genetically determined abnormalities or temporary causes, such as:
- age, the risk of formation and separation of a blood clot is high in men over 45-50 years of age and in women after the onset of menopause;
- hereditary predisposition;
- mutation of genes that determine the synthesis of blood coagulation factors; recently, such disorders and the possibility of their correction have been actively studied;
- pregnancy;
- forced physical inactivity associated with the consequences of severe injury, stroke or other pathologies;
- liver diseases;
- diabetes;
- hypertonic disease;
- slowing of blood flow due to arrhythmia and other pathologies of the cardiovascular system;
- disruption of the structure of the vascular wall due to varicose veins, aneurysms, inflammatory process (thrombophlebitis);
- atherosclerosis;
- smoking, alcoholism;
- obesity;
- taking certain medications that increase blood clotting (oral contraceptives, coagulants);
- abdominal operations, surgical interventions on the heart, coronary vessels.
What does it mean that a blood clot has broken off? Blood clots of this nature are tightly attached to the wall of veins or arteries. Symptoms specific to thrombosis appear due to their partial blocking of the lumen of blood vessels.
However, high blood flow speed, fever during infectious diseases, increased blood pressure, and physical stress become the reasons why a blood clot breaks off in a person.
This happens suddenly, and often the outcome of such a condition largely depends on the speed of providing medical care to the person.
https://www.youtube.com/watch?v=nv8d8s9RTxU
The most dangerous situation is complete blockage of a vessel by a clot. With such a pathology, an obstacle to normal blood circulation is created, which often leads to irreversible changes.
A detached wandering thrombus (it is also called a floating thrombus due to the fact that it moves freely along the bloodstream) can clog an artery, which then creates an obstacle to the supply of oxygen to cells, which causes their rapid death.
Vein thrombosis is accompanied by congestion.
One of the causes of sudden death is the occlusion of a coronary artery by a clot that formed in the venous system of the legs and broke off under the influence of external or internal factors.
A blood clot in an artery blocks blood flow, oxygen is not supplied to vital organs, and the person dies.
It is instant death that indicates the presence of blockage of blood vessels, so the most important questions will be whether it is possible to save a person when a blood clot breaks off, and what to do at the first signs of a deadly pathology.
Types of blood clot
Blood clots in the vessels of the lungs
As mentioned above, the most common cause of pulmonary vascular thrombosis is embolism from the deep veins of the lower extremities. Blocking the blood flow at the level of the pulmonary trunk inevitably leads to the death of the patient if the thrombus is not urgently removed. Most often, patients do not have time to receive timely help, since thromboembolism occurs suddenly outside a medical institution. Thrombosis of the lobar branches of the pulmonary artery leads to exclusion of the entire lobe from the breathing process. The mechanism of the pathological effect of massive thrombosis comes down to a reflex spasm of the coronary arteries, which leads to acute heart failure.
mechanism of pulmonary embolism and risk areas for thrombus formation with subsequent embolism
Symptoms of thromboembolism of the branches of the pulmonary artery consist of sudden acute pain in the chest, severe shortness of breath up to respiratory arrest, cyanosis, and cardiac dysfunction. Thrombosis of small vessels of the lungs can be chronic and recurrent, especially in patients suffering from atrial fibrillation, and their symptoms include shortness of breath, dry cough and chest pain.
Clinical picture depending on location
Symptoms and signs of a blood clot in the body will depend on its location.
Lower limbs
Stroke as a result of a blood clot in the head
Blood clots in the vessels of the brain have their own symptoms:
- loss of balance;
- paralysis of limbs;
- speech disorder;
- dizziness.
Obstruction of blood vessels in the brain can lead to a stroke.
Question of the heart
When do blood clots break off more often?
There are many conditions in which the risk of blood clot formation and rupture increases several times. One of them is atherosclerosis.
People suffering from this disease are at increased risk of heart attack, stroke and thrombosis of the lower extremities, which is complicated by gangrene. The main factor leading to such complications is atherosclerotic plaques that accumulate on the walls of blood vessels.
Sometimes it happens that atherosclerotic plaques rupture, releasing the lipids it contains. Platelets perceive these particles as something similar to a wound and stick to them. This is how large blood clots form, which, if they break off, pose a serious danger to life. To prevent disastrous consequences, patients with atherosclerosis are usually prescribed aspirin, which prevents platelets from sticking together and, consequently, the formation of blood clots.
Atrial fibrillation is a fairly common cardiovascular disease, which also increases the risk of becoming a victim of a severed blood clot. With atrial fibrillation, an irregular contraction of the ventricles of the heart is observed, which is why blood can stagnate in the atrium and blood clots form over time. Statistics indicate that the presence of atrial fibrillation increases the risk of stroke by almost 6 times. Therefore, people with such cardiac disorders are prescribed anticoagulant drugs (slow down blood clotting). Taking anticoagulants prevents the formation of protein threads (fibrin), which, in fact, bind platelets into huge blood clots.
The fact is that due to low physical activity, during sedentary work or when you have to stand in one place for a long time every day, stagnation of blood occurs in the veins. A similar effect is caused by varicose veins. In both cases, the risk of blood clot formation increases. If a clot breaks away from a vein, it will be carried directly into the lungs by the bloodstream, which, as already mentioned, causes a pulmonary embolism. Undesirable consequences can also be prevented by taking anticoagulants.
Types of clots
Depending on the location in the vessel:
- parietal (one end is attached to the wall, blood flow is maintained);
- extended (parietal type, but quite long);
- lining (lining almost the entire wall of the vessel, a small lumen is sufficient for blood flow);
- central (located, respectively, in the center, attached to the walls with cords, blood flow is limited);
- clogging (clogs the lumen in the vessel completely).
Depending on the formation mechanism:
- agglutination, white: formed from leukocytes, agglutinated platelets, fibrin strands. Forms slowly, in arteries with fast blood flow;
- coagulation, red: formed during hyperfunction of blood coagulation (a fibrin network captures red blood cells), localized in the veins;
- mixed type (mucous structure, formed by alternating processes of adhesion (sticking together) and agglutination (precipitation) of platelets); hyaline (consists of plasma proteins, platelets, hemolyzed erythrocytes).
Blood clots can also be divided into groups, depending on their location:
- venous (in deep and superficial veins);
- arterial (in deep and superficial arteries);
- wandering (a clot that has broken off from the wall of a vessel and moves through the bloodstream).
- blood clots in the vessels of the microcirculatory system.
Depending on the structure and external qualities, several types of blood clots are distinguished:
- White, most often formed inside the arteries and consisting of fibrin and leukocytes. They also contain platelets.
- Red blood cells consist mainly of platelets and fibrin, but they also include red blood cells - erythrocytes.
- Layered, or mixed, is the most common type. They have a very interesting and original structure. Their head, which is similar in composition to the white thrombus, the body, which is actually a mixed substance, and the tail or ending, the composition of which repeats the composition of the red thrombus. They are found in the veins and heart cavities. The head of such a lifetime clot is fixed on the inner surface of the riverbed.
Hyaline blood clots differ from those previously mentioned in that they do not contain fibrin. They consist of destroyed red blood cells, plasma proteins and platelets. Their presence in the body leads to the development of capillary (microcirculatory) thrombosis.
Depending on where the clots formed, they are distinguished as venous, arterial or microcirculatory.
Blood clots vary in their characteristics.
According to their structure, blood clots are:
- hyaline: formed in small vessels (lungs, gastrointestinal tract, brain, urinary system), reason for formation: the amount of plasma becomes much larger than whole blood;
- red: the reason for their formation is increased blood clotting, while the blood flow is very slow, such a clot forms in the veins;
- white: with fast blood flow, they form slowly in arteries and capillaries;
- mixed (layered): formed in the cavity of the heart and aortic aneurysm, in the veins.
The types and sizes of clots are also subject to appropriate classification; a thrombus can be:
- clogging: a consequence of the proliferation of parietal thrombi, significantly impedes the flow of blood, located on veins, small arteries, large arteries and the aorta, the vessel is blocked by more than 50%;
- parietal: covers up to 50% of the diameter of the vessel and seems to be smeared along its walls (on the heart valves, large arteries, veins, in the heart);
- progressive: grows very quickly along the bloodstream, on the walls of veins and collecting venous vessels;
- dilation: a dangerous phenomenon, since located in the cavity of the aneurysm it can reach enormous sizes and break off, completely clogging the vessel, which can lead to blocking the blood flow and death;
- globular: develops in the left atrium, there is a high risk of avulsion.
Prevention: how to avoid thrombosis?
The consequences of thrombosis are often unfavorable and are caused by impaired blood flow in organs and tissues. With arterial thrombosis, the development of gangrene or heart attack (heart, brain, intestines, limbs) is possible; with venous thrombosis, especially in the vessels of the legs and pelvis, there is a high probability of pulmonary embolism. On the part of the blood clot itself, it may become inflamed with involvement of the vein wall (thrombophlebitis), fragmentation, or secondary infection.
To avoid thrombosis and its complications, you need to follow simple rules for preventing this dangerous condition:
- To give up smoking;
- It is necessary to avoid staying in one position for a long time, taking breaks, raising your legs and warming up with simple exercises;
- Walking on steps is helpful;
- In case of varicose veins, it is necessary to wear compression garments;
- Foot massage and walking are effective;
- After operations, patients need to get up early and become more active;
- If there is a high risk of thrombosis, effective drug prophylaxis should be carried out.
Thrombosis is a rather dangerous phenomenon, but following simple rules of work and rest, a healthy lifestyle, and timely preventive measures will help to avoid it.
What causes a blood clot to form?
Virchow's triad explains the reasons for the formation of blood clots:
- Slowing blood flow. Most often, this cause occurs in people who lead a sedentary lifestyle, are obese, have been on bed rest for a long time, or as a result of heart failure. Blood clots in the veins of the legs are formed due to disruption of the venous valves due to varicose veins and pregnancy.
- Increased blood clotting. This problem is extremely rarely hereditary, so its main cause is diseases that occur accompanied by high temperature, alcohol abuse, dehydration, dieting (the body dries out, deprived of moisture - this is how weight loss is achieved), uncontrolled use of diuretics medications, long-term use of Viagra, oral contraceptives, hormonal drugs. In order to have healthy blood vessels, it is necessary to avoid stressful situations that lead to a powerful release of adrenaline in the body, which leads to the release of active components into the blood, leading to increased blood clotting.
- Damage to blood vessels (internal tissues). Vessels are damaged as a result of operations and injuries. The lower extremities are especially susceptible to them. In addition, inflammatory diseases, toxic poisoning, and oncology pose a threat to healthy blood vessels. Poor nutrition (atherosclerotic plaques are formed under the influence of excess cholesterol) and smoking also play a negative role.
Thrombosis system in the body
Blood in a liquid state exists only within a vessel. As soon as the integrity of the capillary is disrupted, platelet activity increases sharply. They rush towards the damage, and a blood clot begins to form. This is a system of primary hemostasis and it works only when a small vessel is damaged. The result will be a so-called “white blood clot”.
If a vein is damaged, the secondary hemostasis system is activated. This is a system of cascade reactions that start and go on their own. The process involves 13 specific substances – blood factors. The result of this complex mechanism will be a “red blood clot”.
The formation of blood clots is schematically as follows:
Diagnostics
Timely detection of a blood clot is an opportunity to avoid surgery and even save your life.
Symptoms of thrombosis cannot always be called pronounced.
- A coagulogram, clinical blood test, and D-dimer are done.
- A study is carried out using x-rays of the venous bed. A special contrast agent is first injected into the body, which stains the inside of the vessels, and then an x-ray is taken. Science does not stand still; modern research is now being done, such as duplex angioscanning.
- Either magnetic resonance imaging or computed tomography is performed. This is done if the ultrasound did not show anything.
- Diagnostics using ultrasound.
Hemocoagulation (blood clot reaction) – Doctor's Library
Hemostasis is a system that maintains the fluid state of the blood and prevents the development of bleeding. Blood carries out vital functions in the human body, so significant loss of blood threatens to disrupt the functioning of all organs and systems.
The blood coagulation system includes three components:
- The coagulation system itself directly carries out blood coagulation.
- Anticoagulant system - the action is aimed at preventing blood clotting (pathological thrombus formation).
- The fibrinolytic system ensures the breakdown of formed blood clots.
Blood coagulation is a physiological process that prevents the exit of plasma and blood cells from the bloodstream by maintaining the integrity of the vascular wall.
The doctrine of blood clotting was formed by A. Schmidt back in the last century. When bleeding occurs, structures such as the endothelium, coagulation factors, formed elements, and mostly platelets are activated and participate in stopping it. To carry out blood coagulation, substances such as calcium, prothrombin, and fibrinogen are needed.
Blood clotting
Stages of primary hemostasis (vascular-platelet)
The process of blood coagulation begins with the inclusion of the vascular-platelet stage. There are four stages:
- There is a short-term spasm in the vascular bed, which lasts about 1 minute. The lumen diameter narrows by 30% under the influence of thromboxane and serotonin, which are released from activated platelets.
- Platelet adhesion - platelets begin to accumulate near the damaged area, they change - they change shape and form processes, and are able to attach to the vascular wall.
- Platelet aggregation is the process of platelets sticking together. A loose thrombus is formed that can allow plasma to pass through, and as a result, more and more platelets are layered on top of the newly formed thrombus. Then it thickens and the plasma does not pass through the dense clot - irreversible platelet aggregation occurs.
- Thrombus retraction is the continued compaction of a thrombotic clot.
The vascular-platelet method of stopping bleeding is primary hemostasis; there is a more complex mechanism of blood clotting - this is secondary hemostasis, which occurs with the help of enzymatic and non-enzymatic substances.
Stages of secondary hemostasis
There are 3 phases of blood coagulation at the stage of secondary hemostasis:
- Activation phase - enzymes are activated, everything ends with the formation of prothrombinase and the production of thrombin from prothrombin;
- coagulation phase – formation of fibrin threads from fibrinogen;
- retraction phase – a dense thrombus is formed.
Mechanism of primary thrombus formation
First phase of blood clotting
Plasma blood coagulation factors are a set of inactive enzymes and non-enzymatic compounds that live in the plasma part of the blood and blood platelets. Blood clotting requires, among other things, Ca(IV) ions and vitamin K.
When tissues are damaged, blood vessels rupture, hemolysis of blood cells occurs, and a series of reactions with enzyme activation occurs. The onset of activation is due to the interaction of plasma coagulation factors with destroyed tissues (external type of coagulation activation), parts of the endothelium and formed elements (internal type of coagulation activation).
External mechanism
From the shell of destroyed cells, a specific protein, thromboplastin (factor III), enters the bloodstream.
It activates factor VII by attaching a calcium molecule, this newly formed substance affects factor X for subsequent activation.
After X factor combines with tissue phospholipids and V factor. The formed complex converts a fraction of prothrombin into thrombin in a couple of seconds.
Internal mechanism
Under the influence of destroyed endothelium or formed elements, factor XII is activated, which, after exposure to plasma kininogen, activates factor XI.
XI acts on factor IX, which, after entering the active phase, forms a complex: “coagulation factor (IX) + Antihemophilic factor B (VIII) + platelet phospholipid + Ca (IV) ions.” It activates the Stewart-Prower factor (X).
Activated X, together with V and Ca ions, act on the phospholipid membrane of the cell and form a new formation - blood prothrombinase, which ensures the transition of prothrombin to thrombin.
Plasma coagulation factors include non-enzymatic proteins - accelerators (V, VII). They are needed for efficient and rapid blood sedimentation, because they accelerate coagulation thousands of times.
The external blood clotting mechanism lasts approximately 15 seconds, the internal one takes from 2 to 10 minutes. This coagulation phase ends with the formation of thrombin from prothrombin.
Prothrombin is synthesized in the liver; for synthesis to take place, vitamin K is needed, which comes with food and accumulates in the liver tissue. Thus, with liver damage or vitamin K deficiency, the blood coagulation system does not function normally, and uncontrolled blood flow from the vascular bed often occurs.
Table of blood clotting factors
Clotting factors
| Factors | Properties |
| I – fibrinogen | Thrombin initiates the conversion of the first factor to fibrin |
| II – prothrombin | Synthesis in the liver only together with vitamin K |
| III – thromboplastin | With its participation, prothrombin is converted into thrombin |
| IV – calcium ions | Needed to activate clotting factors |
| V – proaccelerin | Stimulates the transition of prothrombin to thrombin |
| VI – whey accelerator | Initiates the transition of prothrombin to thrombin |
| VII – proconvertin | Acts on the third factor (activation) |
| VIII – antihemophilic factor A | X factor cofactor |
| IX – antihemophilic factor B (Christmas) | Activates factors VIII and IV |
| X – Stewart-Prower factor | Prothrombinase stimulation |
| XI – thromboplastin precursor | Activates factors VIII and IX |
| XII – Hageman factor | Takes part in the conversion of prekallikrein to kallikrein |
| XIII – fibrin-stabilizing factor | Stabilization of the formed fibrin mass |
Second phase of blood coagulation
Blood coagulation is associated with the transition of factor I into an insoluble substance - fibrin. Fibrinogen is a glycoprotein that, when exposed to thrombin, breaks down into a low molecular weight substance - fibrin monomers.
The next step is the formation of a loose mass - fibrin gel, from which a fibrin network (white thrombus), an unstable substance, is formed. To stabilize it, fibrin-stabilizing factor (XIII) is turned on and the blood clot is fixed in the damaged area. The formed fibrin network traps blood cells - the clot turns red.
Third phase of blood coagulation
Retraction of a blood clot occurs with the participation of the protein thrombostenin, Ca, fibrin filaments, actin, myosin, which provide compression of the formed thrombus, thereby preventing complete blockage of the vessel. After the retraction phase, blood flow through the damaged vessel is restored, and the thrombus fits tightly and is fixed to the wall.
To prevent further blood clotting, the body's anticoagulant system is activated. Its main components: fibrin threads, antithrombin III, heparin.
Blood platelets do not adhere to intact vessels; this is facilitated by vascular factors: endothelium, heparin compounds, smoothness of the internal lining of blood vessels, etc. Thus, balance is maintained in the hemostatic system and the functioning of the body is not disturbed.
Blood coagulation diagram
Diagnosis and treatment of thrombosis
The first step towards a cure is timely identification of the problem.
Treatment of thrombosis is carried out exclusively under the supervision of a physician, in a hospital setting.
For diagnosis, you need to consult a phlebologist or cardiologist.
He will evaluate the blood clot, the possibility of its rupture, formulate a diagnosis, and select a treatment method.
Treatment of thrombophlebitis will depend on the type of thrombosis.
Cuperosis is a very unpleasant cosmetic defect, which manifests itself in the form of red plexuses of capillaries visible through the sensitive skin of the face. Naturally, people who are faced with such a problem try in every possible way to find an effective remedy that will help remove spider veins.
At the pharmacy you can find dozens of drugs with their pros and cons. In this article we will analyze the most popular form of the drug - cream for rosacea on the face.
We will compare different drugs and find out which cream, judging by people’s reviews, is the most effective...
How to recognize blood clots
Vein blockage can be recognized by the following manifestations: symptoms of outflow disturbance (heaviness, swelling, distension), pain. The severity of symptoms depends on the degree of damage to the vessel. Blockage of deep vessels causes the blood flow to be redirected to the superficial veins, they bulge and become visible. Arterial thrombosis manifests itself as slowly increasing signs of ischemia.
You can find out whether pathological thrombus formation is occurring and identify its location thanks to specific symptoms:
- when the pulmonary artery is damaged, chest pain occurs, the skin turns pale or blue, the veins in the neck are swollen, and wheezing occurs;
- portal vein thrombosis is associated with chest pain, bloating, indigestion, vomiting, change in stool color;
- blood clots in the veins of the legs are manifested by swelling, pain while walking, unpleasant sensations on the inner surface of the thigh and foot, and cramps;
- blockage of blood vessels in the upper extremities has symptoms in the form of swelling, pain, blue discoloration;
- damage to the blood vessels of the brain is manifested by headache and dizziness, loss of consciousness, convulsions, nausea, vomiting, hearing and vision impairment;
- blockage of the mesenteric vessels is indicated by dull pain in the body, bloating, increased body temperature, nausea, vomiting, and deterioration of the patient’s condition.
Every patient should understand how to know if thrombosis has occurred. Especially people at risk. If you detect the first signs of pathology, you should consult a doctor who will confirm or refute the diagnosis and prescribe treatment.
Fibrinolytics: drugs, indications for use
Fibrinolysis is the process of dissolving blood clots. Accordingly, fibrinolytics are substances that promote the dissolution of blood clots by destroying the fibrin threads that form the structure of blood clots.
Fibrinolytic drugs are used only to dissolve already formed blood clots, but do not prevent their reappearance. Moreover, the use of these drugs may lead to increased platelet aggregation and an increased risk of the formation of new blood clots.
Therefore, they are prescribed only in extreme cases.
Indications for use
1. Massive thromboembolism of the pulmonary arteries.
In this condition, blood clots block the lumen of the branches of these vessels. Despite the name (artery), it is not arterial, but venous blood that flows in them.
It rushes to the lungs to give off carbon dioxide and receive oxygen. If the vessels are blocked by blood clots, gas exchange is disrupted.
To avoid death or disability of the patient, he is prescribed fibrinolytics.
2. Myocardial infarction with ST segment elevation on ECG.
This disease develops when the heart muscle no longer receives enough oxygen. As a result, tissue death begins. Oxygen is not supplied because the blood vessels are partially blocked by blood clots. Fibrinolytic therapy is used to dissolve them.
3. Severe proximal deep vein thrombosis of the legs.
Significantly increases the risk of pulmonary embolism, which often ends in the death of the patient. The word “proximal” means that the blood clotted vessels are located closer to the thigh than to the foot.
Proximal thrombosis is observed in the popliteal or femoral vein. It is accompanied by swelling of the limb and severe pain.
4. Thrombosis of the central retinal artery. Fibrinolysis with appropriate drugs is performed to preserve vision.
Blood clots in the vessels of the legs
blocking of the vein lumen by a thrombus
Vascular thrombosis of the lower extremities is often associated with vein pathology, when varicose veins, blood stagnation, and changes in hemostasis contribute to thrombus formation. An arterial thrombus in the leg or arm can form due to injuries, atherosclerotic lesions, or inflammation in the arteries.
Symptoms of thrombosis of the blood vessels of the legs are reduced to intense pain, swelling, blueness of the skin, changes in skin temperature with massive damage. Closure of one of the veins is accompanied by swelling and minor pain in the calf muscles, while the general condition of the patients is satisfactory. When the bundle is localized in the superficial veins, it is possible to palpate the dense contents in a certain area of the vessel.
Elderly people, patients suffering from diabetes mellitus, and those who are overweight are highly susceptible to thrombosis of the deep veins of the lower extremities. The risk group includes people who have undergone long-term surgical interventions, as well as pregnant women.
The danger of venous thrombosis of the legs lies not only in local circulatory disorders, but also in the possibility of a blood clot breaking off and impairing blood flow in the lungs. Migrating from the veins of the lower extremities to the inferior cava, then through the right half of the heart, blood clots rush into the pulmonary trunk and its branches, blocking blood flow in the pulmonary circulation. This condition is called pulmonary embolism.
First aid
When the first signs of separation appear, the patient should immediately take a horizontal position (comfortable). You should immediately call an ambulance with a cardiology team.
Under no circumstances should you heat the area when a blood clot breaks off: it is better to apply a cold compress. It would not be superfluous to take an antispasmodic or analgesic.
It is better to find out in advance about your predisposition to developing blood clots. It is worth undergoing diagnostics and, if their presence is determined, immediately ask your doctor what to do in the event of a tear, as this can happen at any time.
Treatment will consist of taking antiplatelet agents exclusively as prescribed by the attending physician. Surgical intervention in the form of blood clot removal (thrombectomy) completely prevents serious consequences.