Symptoms
The symptoms of diabetic polyneuropathy are directly dependent on the stage and form of its development, as well as the therapy used.
Sensory disorders
Characteristic manifestations of sensory pathology. They can be determined solely by diagnostic tests (subclinical form) or become patient complaints (clinical form). Patients suffer from pain. The pain can be burning, baking, shooting, throbbing. Its appearance can be triggered even by factors that do not cause discomfort in healthy people.
Important! Diabetic polyneuropathy of the lower extremities is characterized by similar manifestations on the feet and legs, since the endoneurial vessels are affected first.
The patient may complain of numbness, a feeling of goosebumps, a burning sensation, and increased sensitivity to cold, heat, and vibration. Physiological reflexes are preserved, but pathological ones may be absent.
As a rule, sensory disorders are symmetrical. When an asymmetric pathology appears, the pain syndrome begins in the pelvic area and goes down the thigh. This is accompanied by a decrease in the volume of the affected limb, a violation of its proportionality in relation to the rest of the body.
Impaired pain sensitivity is one of the striking symptoms of polyneuropathy
Combined pathology
The development of sensorimotor polyneuropathy in most cases has a chronic course. Diabetics complain of the following symptoms:
- feeling of numbness;
- pain of a different nature;
- impaired sensitivity up to complete absence;
- muscle weakness;
- absence of physiological and appearance of pathological reflexes;
- night cramps of the lower and upper extremities;
- lack of stability when walking.
A frequent complication of chronic processes in combination with mechanical damage is diabetic foot, a pathological condition in which the lesion affects all structures, including cartilage and bone elements. The result is deformation and gait disturbance.
An important point is to differentiate the diabetic sensorimotor form from alcoholic polyneuropathy.
Autonomous defeat
Nerve cells that are localized in internal organs can also be damaged. Symptoms depend on which organ or system is affected. Pathology of the heart and blood vessels is manifested by orthostatic hypertension, pulmonary edema, and impaired sensitivity to physical activity. Patients complain of irregular heart rhythm, increased blood pressure, shortness of breath, and cough. Lack of timely treatment can lead to death.
Heart rhythm disturbance is a possible symptom of autonomic pathology
Damage to the gastrointestinal tract is manifested by paresis, decreased tone of its parts, disruption of normal microflora, and reflux disease. Patients suffer from attacks of vomiting, heartburn, diarrhea, weight loss, and pain.
Polyneuropathy of the genitourinary system is accompanied by bladder atony, urine backflow, sexual dysfunction, and secondary infections are possible. Pain appears in the lower back and above the pubis, urination becomes frequent, accompanied by pain and burning, body temperature rises, and pathological discharge from the vagina and urethra appears.
Other lesions:
- disruption of sweating processes (increased or sharply reduced, even completely absent, work of the sweat glands);
- pathology of the visual analyzer (the pupil decreases in diameter, visual acuity sharply decreases, especially at dusk);
- Adrenal polyneuropathy has no symptomatic manifestations.
Glyceryl trinitrate
Glyceryl trinitrate, traditionally used as a vasodilator for angina, provides significant relief from pain associated with diabetic neuropathy. This was demonstrated in a double-blind, placebo-controlled study that assessed the effectiveness of glyceryl trinitrate spray in 48 patients with painful diabetic neuropathy [48]. Twenty-four patients in the study group used topical glyceryl trinitrate spray on their legs during sleep for four weeks, while the other 24 used a spray containing a placebo. Glyceryl trinitrate was well tolerated, and only one patient was withdrawn from the study due to adverse side effects. Researchers associate the positive effect with vasodilation, which occurs due to nitric oxide, a derivative of glyceryl trinitrate. Good results were obtained when using this spray in combination with valproic acid [49].
Treatment of diabetic neuropathy
The main directions of therapy are the impact on the main cause of polyneuropathy in diabetes mellitus - high blood sugar. Additionally, it is recommended to get rid of risk factors for the progression of neurological disorders - smoking, alcoholism, high cholesterol, high blood pressure.
Antioxidants, vitamins, and agents for improving tissue metabolism are highly effective. Neuropathic pain can be relieved with neurotropic medications. In the early stages and for prevention, physiotherapy is used.
We recommend reading the article on diagnosing diabetic neuropathy. From it you will learn about the primary diagnosis of diabetic neuropathy, diagnostic kits, as well as electrophysiological diagnostic methods and additional examination.
And here is more information about diabetic neuropathy of the lower extremities.
Medicines to compensate for diabetes
An increase in sugar levels triggers a whole chain of pathological reactions. They contribute to damage to nerve fibers at almost all levels. Therefore, the basis of all therapeutic measures is to reduce glucose levels.
This can be achieved with a diet low in simple carbohydrates, insulin therapy and pills to normalize carbohydrate metabolism. An intensified insulin administration regimen, which uses a combination of long- and short-acting drugs, helps reduce the likelihood of polyneuropathy by almost 60% compared to traditional administration.
For type 2 diabetes, Glucophage, Diabeton and Pioglar are very effective. If it is not possible to compensate for high blood sugar with the help of tablets, then insulin must be added to the treatment.
It is important that the level of glycated hemoglobin from the earliest stages of diabetes does not rise above 7%. This correction in most cases reduces pain, improves the general condition of patients and the functional characteristics of nerve fibers
Thioctic acid
Metabolic disorders in diabetes mellitus are accompanied by an increased level of formation of free radicals with a reduced level of antioxidant activity of the body's own systems. This is manifested by the destruction of nerve fibers and the inner lining of blood vessels.
Preparations based on alpha-lipoic acid prevent the deterioration of nerve nutrition, which reduces both patient complaints of pain and burning in the legs and helps to increase sensitivity according to electroneuromyography.
Electroneuromyography
The most common medications based on thioctic acid: Espa-Lipon, Berlition, Thiogamma. Their use is justified for:
- prevention of hemoglobin glycation and oxygen starvation of tissues;
- improving brain function;
- restoration of blood circulation in the lower extremities.
The advantage of alpha-lipoic acid is good tolerability, improvement in the quality of life of diabetics, carbohydrate metabolism, and reduction in the manifestations of fatty hepatosis.
The first manifestations of the therapeutic effect appear after a month of use. The minimum course is three months. After a month or three, the administration of thioctic acid must be repeated.
Vitamins
Vitamin deficiency is found in patients with diabetes in most cases. This makes nerve fibers more vulnerable to metabolic disorders. The introduction of vitamin preparations helps:
- improve the transmission of impulses between nerve cells and from nerves to muscles;
- slow down the destruction of neurons and the combination of proteins with glucose;
- activate enzymes that regulate the metabolism of proteins and fats;
- ensure the formation of neurotransmitters (serotonin, norepinephrine, dopamine);
- uptake glucose by neurons;
- stimulate hematopoiesis;
- restore the myelin sheath;
- reduce pain.
It has been proven that isolated administration of vitamins is less effective than the use of complex drugs. Usually, Neurobion or Milgamma injections are first used for two weeks, and then they switch to tablets for at least a month. Diabetics are prescribed 2 to 4 such courses per year.
Local anesthetics
Patches and gels containing 5% lidocaine are local anesthetic products. It is believed that the action of lidocaine is based on blocking the movement of sodium ions across the cell membrane of neurons. This stabilizes the cell membrane and prevents the propagation of action potentials and consequently reduces pain. The clinical effectiveness of lidocaine wafers has been demonstrated in several open-label studies [43–45]. Up to 4 plates can be applied to the area of pain at the same time. In the studies conducted, the duration of treatment was 4–5 weeks. Among the adverse reactions, burning and erythema at the application site are most often observed.
Capsaicin is a local anesthetic that is obtained from the pods of red hot peppers or chili peppers. The mechanism of action of capsaicin is believed to be based on the depletion of substance P from the endings of peripheral sensory nerves. In some countries, the use of capsaicin is indicated for the treatment of neuralgia, such as postherpetic neuralgia or the painful form of diabetic neuropathy. Capsaicin is available over the counter in the form of a variety of lotions, creams, gels, and roll-ons containing the active ingredient at concentrations of 0.025%, 0.050%, or 0.075%. Typically applied four times daily to the entire painful area. In the treatment of pain in DPN, one study showed a 40% reduction in pain over 8 weeks of treatment [46]. It should be noted that pain often increases when capsaicin is first applied. Burning, redness, and tingling at the application site are the most common side effects of capsaicin.
How to treat lower extremity neuropathy
For effective treatment of the disease, it is important to follow a treatment system that will comprehensively affect all parts of the pathogenesis of the pathology. Neuropathy of the lower extremities has the following treatment features: . The concentration of sugar in the blood must be clearly regulated; it is necessary to maintain a value close to normal at a constant level, without sharp fluctuations
Antioxidants are used to reduce free radicals. This will reduce the extent of peripheral nerve damage. To restore already damaged nerve endings, vascular and metabolic agents should be used. You need quality pain relief. The use of non-drug (supportive) treatment is appropriate.
- The concentration of sugar in the blood must be clearly regulated; it is necessary to maintain a value close to normal at a constant level, without sharp fluctuations.
- Antioxidants are used to reduce free radicals. This will reduce the extent of peripheral nerve damage.
- To restore already damaged nerve endings, vascular and metabolic agents should be used.
- You need quality pain relief.
- The use of non-drug (supportive) treatment is appropriate.
Antioxidant therapy
In the presence of polyneuropathy, it is important to support the body with antioxidants, which have the following properties:
- Normalize metabolic processes in the body, preventing the release of toxins.
- Protect cells from the destructive effects of toxic substances.
- They slow down the aging process of cells and have regeneration properties at the cellular level.
The antioxidant preparations include alpha-lipoic acid. It is able to accumulate in tissues and affect nerve endings, preserving their integrity and ability to transmit nerve impulses.
The course of treatment is quite long and can last up to 6 months. The highest results from taking the drugs are observed when the following scheme is used: in the first 10-12 days of the course, antioxidants are administered intravenously by drip, dissolved in a large amount of sodium chloride. The course is then continued by taking 600 mg tablets orally, half an hour before the main meal.
The most effective drugs are:
- Thiogamma;
- Dialipon;
- Tio-Lipon;
- Espa-Lipon;
- Lipamide;
- Octolipen;
- Thioctacid;
- Lipothioxone.
Types of neuropathy
Since the peripheral nervous system is divided into somatic and autonomic (vegetative), two types of diabetic polyneuropathy are also called. The first gives rise to multiple non-healing trophic ulcers of the lower extremities, the second - problems with urination, impotence and cardiovascular accidents, often with fatal outcomes.
Another classification is based on the functions of the nervous system that are disrupted as a result of the development of pathology:
- sensory polyneuropathy associated with increased pain in the legs, or, conversely, loss of tactile sensitivity;
- motor polyneuropathy, which is characterized by muscular dystrophy and loss of the ability to move;
- sensorimotor polyneuropathy, combining the features of both of these complications.
A manifestation of the latter, mixed pathology is neuropathy of the peroneal nerve. Diabetics with this disease do not feel pain in certain places of the foot and lower leg. These same parts of the surfaces of the legs do not react to either cold or heat. In addition, patients lose the ability to control their feet. Patients are forced to walk, raising their legs unnaturally high ("rooster" gait).
Diabetic distal polyneuropathy
This is a pathology that causes the death of nerve fibers. The disease leads to a complete loss of tactile sensitivity and ulceration of the farthest part of the lower extremities - the feet. The typical condition for diabetics with distal DPN is a dull, aching pain, which is often so severe that the person cannot sleep. In addition, sometimes my shoulders begin to ache. Polyneuropathy progresses, and this leads to muscle atrophy, bone deformation, flat feet, and foot amputation.
Peripheral
With this type of disease, severe disorders of the sensorimotor functions of the legs occur. Diabetics suffer from pain and numbness not only in their feet, ankles, lower legs, but also in their hands. Peripheral polyneuropathy occurs mainly when doctors prescribe potent antiviral drugs with serious side effects: Stavudine, Didanosine, Saquinavir, Zalcitabine
It is important to diagnose this pathology in a timely manner in order to immediately discontinue the drug.
Sensory polyneuropathy
The main feature of the pathology is loss of sensation in the legs, the degree of which can vary significantly. From minor tingling to complete numbness, accompanied by the formation of ulcers and deformation of the feet. At the same time, the lack of sensitivity is paradoxically combined with unbearably severe pain that occurs spontaneously. The disease first affects one leg, then often moves to the second, rising higher and higher, affecting the fingers and hands, torso, and head.
Dysmetabolic
The occurrence of this type of complication is often provoked, in addition to diabetes, by diseases of the stomach, intestines, kidneys, and liver. Many nerve plexuses of the extremities may be affected. When the sciatic and femoral neurons are disturbed, pain, trophic ulcers, difficulties with movement appear, knee and tendon reflexes disappear. The ulnar, trigeminal, and optic nerves are often damaged. Dysmetabolic polyneuropathy can occur without pain.
Pathophysiology
Hyperglycemia caused by diabetes mellitus causes metabolic disorders such as intracellular accumulation of sorbitol, excessive protein glycation, and oxidative stress, which significantly impair the structure and function of neurons [3–7]. Oxidative stress promotes damage to endothelial cells underlying the membrane of endoneurial vessels, leading to microvascular dysfunction. The resulting hypoxia and ischemia further activate the processes of nerve damage. An essential mechanism for the formation of diabetic polyneuropathy is a deficiency of neurotrophic factors, which reduces the ability of the affected nerve to regenerate. Activation of protein kinase C and blocking of nitric oxide (NO), the main regulator of vascular wall relaxation, play a role in the pathogenesis of DPN, which contributes to the development of microangiopathy. The role of immune complexes and autoimmune disorders is also discussed.
The appearance of pain in DPN is caused by damage to the thin sensory fibers responsible for pain sensitivity. In this case, the leading mechanisms are peripheral and central sensitization, generation of impulses from ectopic foci of affected nerves, overexpression of sodium channels in peripheral neurons, etc. [1, 3, 8, 9].
Complications
Diabetic neuropathy is a disease with a number of possible complications. Poor healing of wounds, especially on the legs, and their infection can lead to gangrene, and therefore (as a result of a life-threatening infection that spreads throughout the body), to the need for amputation of a limb, sometimes the entire one.
If the bladder does not empty properly, some urine remains in the bladder, which creates an environment for bacteria to survive and multiply. Pathogens can spread to the kidneys, causing frequent urinary tract infections.
The great danger with damage to the autonomic nerves is the disappearance of symptoms of hypoglycemia. These symptoms (sweating, rapid heartbeat, tremors, drooling) are provided by this system. Not showing signs of high glucose levels can be fatal.
Loss of blood pressure control is also dangerous. Orthostatic hypotension can lead to loss of consciousness, falls, and head injury.
Other complications include inability to control changes in body temperature due to impaired sweating, digestive dysfunction, indigestion with vomiting, diarrhea, constipation, and sexual dysfunction.
Severe complications – pain, disability, loss of self-sufficiency, depression, social isolation.
Treatment
Elimination of diabetic neuropathy takes a long time and involves several stages. First of all, it is necessary to bring diabetes mellitus to the stage of compensation - for this, patients are prescribed insulin or antidiabetic drugs. In some cases, after such therapy, there is an increase in the intensity of the symptoms of diabetic neuropathy. The duration of this condition can reach two months, this indicates that reverse changes occur in the nerves, i.e. they are gradually restored.
Additional drug treatment for diabetic neuropathy involves taking medications aimed at eliminating pain and restoring normal nerve function. To do this, patients need to take:
- preparations containing thioctic acid;
- non-steroidal anti-inflammatory drugs;
- neurotropic drugs;
- antidepressants;
- anticonvulsants;
- antiarrhythmic drugs;
- anesthetics.
Classification
Autonomic and peripheral diabetic neuropathy
There are several types of this disorder, each of which is characterized by its own symptoms and damage to certain nerves:
- generalized symmetrical polyneuropathy;
- autonomic neuropathy;
- focal or multifocal diabetic neuropathy.
Each of these forms has its own classification. Thus, the generalized variety is divided into:
- sensory neuropathy - the nerves responsible for sensitivity are damaged. This may be expressed in a person’s inability to distinguish hot from cold, pain and other tactile sensations;
- motor – there is a disruption in the functioning of the nerves responsible for the movement of the limbs. In the clinical picture, this will be expressed in muscle weakness, decreased reflexes of the arms and legs;
- sensorimotor or combined neuropathy;
- hyperglycemic neuropathy.
In turn, autonomic neuropathy occurs:
- cardiovascular, i.e. the normal functioning of the nerves of the cardiovascular system is disrupted;
- gastrointestinal – associated with damage to the nerves responsible for the functioning of the gastrointestinal tract;
- urogenital - characterized by the involvement in the pathological process of nerves that regulate the functioning of the genitourinary system;
- respiratory;
- associated with the work of the pupil;
- adrenal medulla;
- endocrine;
- associated with the function of sweat glands and thermoregulation;
- diabetic cachexia.
The focal type of this disorder also has several types:
- cranial and tunnel neuropathy;
- amyotrophy;
- plexopathy;
- chronic demyelinating polyneuropathy of an inflammatory nature.
In addition, there are several stages that the disease goes through and differ in the intensity of symptoms:
- subclinical neuropathy;
- clinical, which can be chronic, acute or distal, with complete loss of sensation;
- stage of late complications.
Stages of diabetic neuropathy
Diabetic neuropathy treatment
The treatment of diabetic neuropathy is mainly carried out by an endocrinologist. If necessary, he refers the patient to a neurologist, as well as to a diabetic foot specialist (podiatrist, not to be confused with a pediatrician). The participation of an infectious disease specialist and a urologist may be necessary, as well as a specialist who will help a diabetic quit smoking.
Most patients are looking for miracle ways to treat diabetes complications that could replace dieting and insulin injections. Such methods do not yet exist. Without achieving and maintaining normal blood glucose levels, diabetic neuropathy cannot be cured. Read and use the step-by-step type 2 diabetes treatment plan or type 1 diabetes management program. Let us repeat that damage to nerve fibers is a reversible complication. You can completely get rid of it if you keep your sugar at a stable, normal level, following a daily regimen.
Diet options depending on diagnosis:
Diabetes type 2 Diabetes type 1 Diet table No. 9 Menu for the week: sample
Some websites of domestic and foreign clinics make charlatan promises of a quick and easy cure for diabetic neuropathy. Other reputable medical resources say that this complication is incurable, you can only slow down its development. The truth is in the middle. Without achieving and maintaining normal blood sugar levels like healthy people, diabetic nerve damage is truly incurable. However, it is entirely within your power to bring your glucose levels back to normal using Dr. Bernstein's approach. First of all, you need to switch to a filling and tasty low-carb diet.
Can you recommend pills for diabetic neuropathy?
No pill will help with the numbness and loss of sensation caused by diabetic neuropathy. Nothing helps with these problems at all, except for normalizing blood sugar. When it comes to pain, there are medications that are widely used that can help relieve it. These are anticonvulsants, antidepressants and opioid analgesics. They are described in detail in the article “Pain in Diabetes.”
Among dietary supplements, many diabetics take alpha-lipoic acid, as well as B vitamins. The effectiveness of these drugs is questionable, the results of studies are both positive and negative. Neither alpha lipoic acid nor B vitamins can replace following a low-carbohydrate diet and insulin injections to maintain normal blood sugar.
If you want to try it, order alpha lipoic acid and B vitamins from the USA here. It will be several times cheaper than Berlition, Thiogamma, Thioctacid, Milgamma, Benfotiamine and other tablets that are sold in pharmacies. You can choose high-quality supplements that have dozens or hundreds of real positive reviews.
Patients often experience retention of residual urine in the bladder. You need to be tested for urinary tract infections. Take antibiotics if necessary to combat them. The problem of urinary incontinence has several solutions, which you can easily find on specialized websites. If you have problems with the gastrointestinal tract, read the article “Diabetic Gastroparesis” and do what it says. To prevent orthostatic hypotension from leading to fainting, you need to learn to slowly get up from a sitting or lying position.
What are some good folk remedies?
No folk remedies for diabetic neuropathy help. Including burdock, calendula, elecampane, rosemary, cloves and other plants, as well as blue clay and turpentine. Some foods that traditional medicine recommends increase blood sugar and worsen diabetes. These are Jerusalem artichoke, dates, honey, lemon, goat's milk. Traditional treatment for neuropathy and other complications of diabetes does not help, but leads to the grave of underdeveloped, lazy and gullible patients. You will get more benefits from drinking pure water than from using these remedies.
Diagnostics
The diagnostic algorithm depends on the form of diabetic neuropathy. At the initial consultation, the medical history and complaints about changes in the cardiovascular, digestive, respiratory, genitourinary, and visual systems are carefully analyzed. In patients with diabetic neuropathy, it is necessary to determine the level of glucose, insulin, C-peptide, and glycosylated hemoglobin in the blood; study of pulsation in peripheral arteries, blood pressure measurement; conducting an examination of the lower extremities for the presence of deformities, fungal infections, corns and calluses.
Depending on the manifestations, in addition to the endocrinologist and diabetologist, other specialists may participate in the diagnosis of diabetic neuropathy - a cardiologist, gastroenterologist, neurologist, ophthalmologist, podologist. The primary examination of the cardiovascular system consists of conducting an ECG, cardiovascular tests (Valsalva maneuver, orthostatic test, etc.), echocardiography; determination of cholesterol and lipoprotein levels.
Neurological examination for diabetic neuropathy includes electrophysiological studies: electromyography, electroneurography, evoked potentials. Reflexes and various types of sensory sensitivity are assessed: tactile using monofilament; vibration - using a tuning fork; temperature - by touching a cold or warm object; painful - by tingling the skin with the blunt side of a needle; proprioceptive - using a stability test in the Romberg position. Sural nerve biopsy and skin biopsy are used for atypical forms of diabetic neuropathy.
Gastroenterological examination for diabetic neuropathy involves ultrasound of the abdominal organs, endoscopy, radiography of the stomach, examination of the passage of barium through the small intestine, and tests for Helicobacter. In case of complaints from the urinary system, a general urinalysis is examined, ultrasound of the kidneys, bladder (including ultrasound with determination of residual urine), cystoscopy, intravenous urography, electromyography of the bladder muscles, etc. are performed.
Preventive measures
To prevent the development of DN, diabetics need to build their lives according to certain guidelines. It consists of:
- maintaining acceptable glucose concentrations. To do this, you need to follow a special diet, engage in adequate physical activity, take insulin and sugar-lowering tablets;
- daily inspection of the NK’s feet for the presence of wounds and cracks;
- protecting feet from damage;
- complete cessation of nicotine and alcohol products;
- systematic use of natural cosmetics to soften the skin;
- regular examination by a specialist;
- body weight control.
Important! Diabetics should not walk barefoot or wear uncomfortable shoes.
Representatives of diabetology believe that one of the significant causes of DN is a deficiency of essential substances in the daily diet of a diabetic. This condition negatively affects internal organs and reduces the activity of drugs that are required to regulate sugar. To prevent this from happening, the patient needs to eat permitted fruits and vegetables in acceptable quantities every day.
DN will not go away on its own. This disease requires serious diagnosis and comprehensive treatment, so at the slightest sign the patient should seek qualified help.
Incidence of the main complication of diabetes mellitus
One of the main complications of diabetes mellitus is neuropathy, and it can develop in both the first and second types.
During the course of the disease, nerve fibers of various calibers are affected, which regulate the conduction of impulses of the autonomic and somatic nervous systems.
Thus, diabetes mellitus provokes the appearance of diabetic neuropathy. The complication develops in 15-65 percent of diabetes cases.
For example, if a person has been suffering from diabetes for 5 years, then polyneuropathy is determined in approximately 15 percent of cases. If you have had diabetes for many years, for example, 30 years, then it is not surprising that neuropathy has appeared, since in this case it is registered in 75 percent of cases.
The formation of the disease is triggered by a key condition - the presence of a huge amount of glucose in the blood. The body is trying with all its might to “eliminate” glucose, while it activates two pathways for the utilization of carbohydrates.
For this reason, the structure of neurons undergoes changes and the intensity and speed of impulse transmission in them decreases.
Due to an increase in the level of glycated hemoglobin, oxygen begins to flow very poorly to the tissues. This is how diabetic polyneuropathy develops.
Causes
The main culprit in diabetic neuropathy is high blood sugar. In diabetes, we are talking specifically about polyneuropathy, because the disease affects almost all nerves. Both the somatic nervous system, responsible for motor activity, and the autonomic nervous system , which controls the functioning of internal organs, suffer.
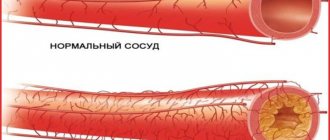
The mechanism of disease development is as follows:
- When blood sugar levels are constantly high, metabolic disorders occur.
- Tissues and cells are in a edematous state.
- Blood pressure increases.
- Blood cannot penetrate into vessels compressed due to edema.
- Small capillaries die first, then larger vessels.
- Due to poor blood supply, the functioning of internal organs is disrupted.
Provided that glucose levels are constantly monitored, neuropathy does not occur. Provoking factors for the development of the disease in diabetics:
- Old age of the patient . Neuropathy usually develops after age 50.
- Duration of the disease. The first signs of the disease appear 5-10 years after the onset of diabetes.
- Constant increase in blood pressure . Swelling of the capillaries is aggravated by increased pressure, and vasospasm occurs.
- Excess body weight.
- Non-compliance with the diet, leading to constant spikes in sugar.
- Consistently high levels of “bad” cholesterol.
- Bad habits of the patient (alcohol, smoking).
- Heredity . The likelihood of neuropathy increases to 30% if close relatives have suffered from the disease. It is believed that some people carry an altered gene in which neurons become much more sensitive to the effects of sugar, they are destroyed and become unable to transmit a signal.
- Limb injuries in which nerve endings are affected. In diabetes, regeneration processes are very poor, so damaged nerves are practically not restored.
- Type of diabetes . In patients with type 2 diabetes, neuropathy develops 2.5 times more often than in diabetics with type 1.
Diagnosis of pathology
Diabetic neuropathy has many branches, each of which has its own symptom. To diagnose diabetic neuropathy, the doctor first takes the patient's medical history.
To obtain the most complete clinical picture, a special scale and questionnaires are used. For example, a scale of neuralgic symptoms, a general scale of symptoms, and others are used.
During a visual examination, the doctor examines the joints, looking at the condition of the foot, foot and palms, the deformation of which indicates neuropathy. Determines whether there are redness, dryness and other manifestations of the disease on the skin.
During an objective examination of the patient, such an important symptom as exhaustion and other secondary signs are revealed. Diabetic cachexia can be extreme when the patient has no subcutaneous fat or fat deposits in the abdominal area.
After the examination, vibration sensitivity examinations are carried out. Using a special vibration device, which the doctor applies to the big toe or other areas. This study is carried out three times. If the patient does not feel the vibration frequency of 128 Hz, then this indicates a decrease in susceptibility.
To determine the type of pathology and find out how to treat it further, the following diagnostic measures are carried out to determine diabetic neuropathy:
- Tactile sensitivity is determined.
- Temperature sensitivity is determined.
- Pain sensitivity is determined.
- Reflexes are assessed.
Diabetic neuropathy is characterized by a varied course, therefore, in the vast majority of cases, all diagnostic measures are carried out without exception.
Treatment of neuropathy is a rather complex, time-consuming and expensive process. But with timely initiation of therapy, the prognosis is favorable.
Botulism toxin
A recent pilot double-blind crossover study demonstrated the effectiveness of botulinum toxin type A in the treatment of pain in 18 patients with DPN [47]. Pain decreased significantly starting from the first week after injection throughout 12 weeks of observation. In 44% of patients, pain reduction on the visual analogue scale (VAS) was more than 3 points. There was also an improvement in sleep starting 4 weeks after the injection. The anti-pain effect of botulinum toxin is associated with the ability of the drug to inhibit afferent nociceptive activity in peripheral sensory nerve fibers.
Treatment
Treatment of diabetic polyneuropathy is complex, and causal therapy is unknown. Therapy is based on slowing the progression of the disease, treating pain and other unpleasant sensations (tingling, burning).
The basis of drug treatment is stabilization and maintenance of an acceptable level of glycemia. This helps delay the development of the disease into a severe stage, and sometimes relieves already present symptoms. For these purposes, oral antidiabetic drugs are used; if there is a lack of insulin, it is administered in the form of injections. In some people, intensive glycemic control and glucose regulation can reduce the risk of developing neuropathy by more than 60%.
It is important to take medications whose action is aimed at tissue regeneration and improvement of tissue metabolism (Actovegin gel).
Pain in diabetic neuropathy of the lower extremities, the treatment of which is complex and individual, is cured with the help of antiepileptic medications and antidepressants. Ointments containing capsaicin are also recommended.
In addition to synthetic drugs and pain relief pills, alternative medicine methods are recommended - acupuncture, relaxation.
An effective medical approach involves the use of substances that promote regeneration and nutrition of nerves (α-lipoic, linoleic acid). It is recommended to take vitamins B and E.
When treating mental disorders in patients with diabetes, caution is important when taking the drug Glutalite - the disease increases the risk of lithium intoxication!
Self-help methods
We must adhere to the principles of prevention. Taking care of your feet, keeping your blood glucose and blood pressure levels in the normal range, eating a healthy diet, and exercising regularly are important. Quitting smoking and alcohol plays a role in preventing and accelerating the treatment of neuropathy and neuritis.
You can try treatment (as an auxiliary therapy) at home using traditional methods. For example, using herbs that help improve diabetes:
- blueberry – blueberry leaves contain myrtilin;
- calamus - calamus root treats all diseases of the pancreas, therefore, helps with diabetes;
- mistletoe - the plant also has a good effect on the pancreas.
Prevention
Diabetic polyneuropathy of the lower extremities (treatment, drugs are prescribed by an endocrinologist, taking into account the person’s condition) more often occurs against the background of diabetes mellitus.
To reduce the risk of its development, patients are advised to follow simple preventive rules:
- give up bad habits (abuse of alcohol, drugs, tobacco products, caffeine);
- monitor blood pressure indicators;
- engage in physical activity;
- monitor blood glucose levels;
- maintain a work-rest regime (a weakened body after stress, lack of sleep and fatigue cannot resist pathological processes);
- control body weight, get rid of extra pounds;
- constantly undergo preventive examinations and examinations by a doctor in order to promptly determine the development of concomitant diseases and begin treatment;
It is important to adhere to a healthy lifestyle, eat right and exercise, and walk more in the fresh air. Drink vitamin complexes and coordinate therapeutic actions with your doctor.