What kind of pathology is this
The disease is accompanied by a slowdown in the speed of blood flow in the brain. Occurs due to outflow disturbances on the way to the heart.
Short-term impairment occurs in every person. For example, when coughing, physical activity, or sharply turning the head. This causes a dull headache.
Venous congestion of cerebral vessels is accompanied by severe disruption of blood flow from the brain through the central nervous system to the myocardium. Slow blood circulation leads to blood stagnation.
Against this background, various pathologies develop. In patients with this disease, venous congestion occurs in the head, and the general outflow is disrupted. The vessels are not saturated with oxygen and useful components.
This leads to their rapid defeat and decreased tone.
Classification of venous circulation
Venous discirculation is classified according to:
- duration of the process (acute and chronic);
- the presence of complications (complicated and uncomplicated);
- stages (first, second and third).
For reference. The first stage includes venous circulation without pronounced clinical manifestations. Such venous discirculations are also often called “silent”. At the first stage, venous discirculation can be detected during a random examination.
Venous dyscirculation of the second stage is manifested by a progressive decrease in working capacity and gradual loss of the ability to self-care, memory loss, and impaired coordination of movements. Restoring lost functions at this stage of the disease is still possible.
At the third stage, venous discirculation is accompanied by the appearance of severe gross neurological symptoms. Complete restoration of lost functions is no longer possible due to severe damage to brain tissue. Treatment is limited to partial recovery and prevention of complications.
Types and classification
It has three main subspecies:
- dyshemia of the central brain;
- vertebral plexuses;
- dyshemia of the ICA basin.
The classification of the disease has 3 stages of development.
- Latent. Not accompanied by severe symptoms. A person does not observe deviations and does not suspect the development of such a pathology.
- Cerebrovenous discirculation. Symptoms appear, but do not affect the person’s normal life.
- Venous encephalopathy. Clinical manifestations cause discomfort to the patient. It is at this stage that pathology is usually diagnosed.
In addition, the disease is determined by its form of development. The primary form is accompanied by circulatory disorders that arise due to changes in venous tone.
The stagnant form is accompanied by the following symptoms: problems with blood outflow from the brain of mechanical etiology. In this case, surgical intervention cannot be avoided.
Diagnostic problems
It is often quite difficult to make a diagnosis of cerebral venous dyshemia. Parents need to contact a neurologist, especially if the baby is nervous and constantly cries. After the examination, blood pressure is monitored for at least 5 consecutive days. Then an X-ray examination of the brain is prescribed. It may be necessary to perform a venography procedure, which will reveal the presence of malignant tumors or dropsy. This study makes it possible to assess the state of blood circulation. MRI gives the best results, as it even allows you to determine the cause of the pathology.
Even if the nature of the disease is established at the extracranial and intracranial levels, it is still difficult to correctly interpret the results obtained. Not a single textbook or scientific article gives a complete picture of the causes of the disease. Consequently, it is quite difficult to develop treatment tactics that will get rid of the pathology or at least eliminate the main symptoms.
In addition, sometimes it is very difficult to establish a diagnosis, since the pathology is a consequence of a disease.
Causes
Occurs for the following reasons:
- traumatic brain injuries, which are accompanied by internal hematomas and bone fractures;
- cerebral edema due to stroke;
- tumors;
- disruption of the development of the venous network;
- neoplasms in the cervical spine;
- congestion in the veins;
- injuries in the peritoneum or thoracic region;
- osteochondrosis, prolapsed discs.
Circulatory disorders are associated with direct and indirect causes.
Causes of venous discirculation
Cerebral venous discirculation can develop against the background of:
- arterial hypertension (especially against the background of chronic uncontrolled hypertension);
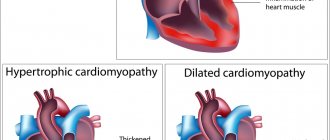
- heart failure;
- tumors of the brain and neck, compressing cerebral vessels;
- severe osteochondrosis of the cervical spine;
- severe endocrine disorders (hyperfunction of the adrenal cortex, hyperproduction of thyroid hormones, disruption of the hypothalamic-pituitary system, decompensated diabetes mellitus, severe estrogen deficiency in women);
- traumatic brain injuries (especially against the background of the formation of large hematomas);
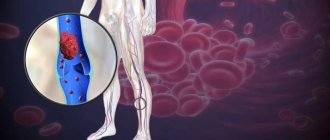
- blood diseases accompanied by an increase in blood viscosity and an increased tendency to thrombus formation;
- genetic diseases accompanied by blood clotting disorders (mutations of the prothrombin gene, deficiency of clotting proteins);
- hyperhomocysteinemia.
Risk factors for the development of venous discirculation
Risk factors that increase the likelihood of a patient developing venous discirculation are:
- smoking;
- alcohol abuse;
- sedentary lifestyle;
- drug use;
- presence of obesity;
- chronic sleep deficiency;
- constant stress;
- abuse of drugs and drinks containing caffeine.
Important! You should pay attention to possible sources of nervous tension. Any excitement can affect the state of the vascular system. With constant unrest, it is easy to get a persistent defect in the venous outflow.
The mechanism of development of venous discirculation
The development of venous discirculation is based on a decrease in the rate of outflow of venous blood, the development of blood stagnation and the appearance of symptoms of chronic (less often acute) cerebral hypoxia.
For reference. In most cases, on average, 3-5 years pass from the appearance of venous discirculation to the development of ischemic stroke or severe vascular dementia .
In the presence of concomitant pathologies that aggravate the course of venous discirculation, and in the absence of treatment, the disease can progress rapidly (complications develop over several months).
Mechanism of disease development and localization
The difficulty may be due to the influence of physiological factors:
- when straining;
- chronic cough;
- singing;
- playing wind musical instruments;
- tilting the head during exercise;
- incorrect position of the head and neck during sleep.
The mechanism of development of the disorder is associated with a violation of the outflow of blood from the brain when the main, extracranial, and intracranial pathways are damaged. Also if stagnation occurs in the small circulation. The pathology is localized in any part of the brain.
Diagnosis of venous discirculation
To identify violations of venous outflow and determine the cause of the disease, the following is carried out:
- measuring blood pressure twice a day with keeping a diary of associated symptoms;
- duplex scanning of cervical and cerebral vessels;
- MRI and CT of the brain;
- rheoencephalography;
- ECG and ultrasound of the heart;
- Ultrasound of the thyroid gland;
- phlebography;
- general blood tests, coagulogram, lipid profile analysis, blood biochemistry, hormonal profile study.
ECHOEG (echoencephalography) can also be used to examine newborns and older children. CSF and venous circulation is assessed.
A mild form of dyshemia when examining a child using echocardiography will show signs of hypertensive-hydrocephalic syndrome (increased intracranial pressure values) and asymmetry of blood flow in the area of the cerebral arteries.
Possible complications
The presence of such a pathology negatively affects the health and condition of the body as a whole. This is associated with a constant risk of complications. The main ones include:
- stroke;
- cerebral infarction;
- encephalopathy.
Any of these conditions can cause irreparable consequences. The disease also often leads to the development of thrombosis.
Treatment of venous discirculation
Treatment is aimed at normalizing the rate of outflow of venous blood, maintaining the tone of the veins, and normalizing the rheological properties of blood.
For reference. If a mechanical obstruction (tumor, hematoma) is detected that prevents the normal outflow of blood, treatment is aimed at eliminating this obstruction and restoring a full outflow of blood.
Drug therapy includes the appointment of:
- nootropic drugs;
- neuroprotectors;
- antioxidants;
- drugs that improve blood rheology;
- phlebotonics;
- means that strengthen the walls of blood vessels.
Additionally, moderate physical activity, massage, and taking vitamin supplements are recommended.
Manifestations
Signs of venous discirculation can be varied. Initially, a mild headache appears, which intensifies over time. Then it becomes stable.
Discomfort appears in a certain area - the temples, the crown of the head, the back of the head. Such manifestations require immediate medical attention.
Heaviness in the head leads to a decrease in the clarity of speech, the ability to think and learn is impaired. This often disrupts orientation in space.
If the disease is ignored in the initial stage, the symptoms will appear more pronounced and severe. Headaches will become constant, especially in the morning. With a sharp turn of the head or prolonged physical activity, the pain may intensify.
Characteristic symptoms of venous stagnation in the head:
- severe headache when blood pressure changes;
- increased body temperature;
- increased or onset of pain when turning the head sharply;
- chills;
- nausea;
- numbness in the limbs;
- dizziness;
- vomit.
If the disease is severe, nerve cells are quickly damaged. The patient may be diagnosed with neurological and psychological disorders.
In childhood, symptoms are the same as in adults.
The main manifestations of a severe form of pathology:
- paralysis;
- paresis;
- disorders of the musculoskeletal system;
- decreased sensitivity;
- pain in some parts of the body;
- convulsions;
- speech disorder;
- loss of ability to read, write;
- the occurrence of epilepsy attacks;
- impaired coordination and orientation in space.
Any signs may appear in varying degrees of severity. It all depends on dysfunction of the brain due to a lack of oxygen and nutrients.
Every patient who suffers from this disease is faced with the occurrence of aggression and excessive irritability. You can observe a change in habits and preferences. Interest in hobbies is often lost.
Patients with such disorders generally deteriorate. The condition is accompanied by processes that lead to the gradual death of brain cells. They are usually involved and responsible for vital processes.
How is venous dyshemia treated?
Treatment methods for such a pathological condition as venous blood circulation largely depend on the severity of the existing manifestations. With a mild form, it is quite possible to cope with the problem using conservative methods. First of all, the patient needs to give up his existing bad habits, including smoking and alcohol abuse. In addition, it is recommended to switch to a healthy diet and avoid overeating. Consumption of large amounts of junk food leads not only to obesity, which negatively affects the functioning of the entire cardiovascular system, but also becomes an impetus for slowing metabolism, which leads to a more pronounced manifestation of venous dyshemia. Drug treatment may also be required.
If a patient has a violation of the venous outflow of the brain with severe symptoms, medications are prescribed to help improve the saturation of brain tissue with oxygen and nutrients. First of all, treatment involves the inclusion of venotonics, which strengthen the walls of blood vessels, increase their elasticity, and also eliminate inflammatory processes. In addition, these drugs allow you to restore vascular tone to the walls of veins and arteries. The drugs most often used for such a pathological condition as a violation of the venous outflow of the brain include:
- Ginkor;
- Aescusan;
- Herbion-esculus;
- Antistax;
- Dr. Theiss;
- Venen-gel;
- Venoplant;
- Antistax;
- Getralex.
Any medicine must be taken according to a clear schedule prescribed by the doctor. In addition to drug therapy, it is necessary, if possible, to normalize the work and rest schedule. Long walks in the fresh air and contrast showers, which can improve blood flow, will be useful. To improve blood circulation, it is also recommended to perform at least a minimum set of physical exercises daily. In addition, a course of massage that improves cerebral blood flow and sanatorium treatment can bring significant benefits. Improved blood flow will eliminate existing manifestations of impaired venous outflow of the brain.
Diagnostics
It is very difficult to detect difficulty in the venous outflow of the brain in the initial stage. Diagnosis in most cases is accidental, during routine or preventive examinations. Signs of the severe stage are similar to other pathologies.
To establish a diagnosis, the following methods are used:
- MRI;
- triplex scanning;
- Doppler ultrasound.
The doctor must examine the patient's medical history to rule out disorders that could lead to the development of this disease.
Etiology of venous dyshemia
The causes of obstruction of the venous outflow of the brain are extremely varied. There are a lot of pathological conditions that can provoke the development of venous dysgemia.
One of the main predisposing factors is cerebral atherosclerosis. As a rule, an increase in the number of cholesterol plaques leads to a mechanical slowdown in blood flow. Almost all people who, due to atherosclerosis, have narrowed vascular lumens by more than 50%, have venous dyshemia. Other factors that can cause a slowdown in the outflow of blood from the vessels in the brain include:
- traumatic brain injuries;
- malignant and benign tumors;
- anomalies in the development of the venous network;
- strokes accompanied by cerebral edema;
- blockage of blood vessels by blood clots;
- abdominal and chest injuries;
- hypertension;
- diseases of the endocrine system;
- osteochondrosis;
- protrusions and intervertebral hernias of any etiology.
Venous outflow may be impaired due to severe intoxication of the body. Such disruption of the vascular system is not uncommon in people who have a long history of smoking. In persons who suffer from alcohol and drug addiction, this pathological condition is observed in almost 95% of cases. Disruption of the venous outflow of the brain due to intoxication is associated with damage and stenosis of the walls of blood vessels caused by the negative influence of certain active substances.
Among other things, some people have a hereditary predisposition to the development of such a pathological condition as venous dyshemia. As a rule, in such cases, in representatives of the same family related by blood, the first manifestations of a slowdown in the outflow of blood from the vessels of the brain are observed at approximately the same age. For example, if the first signs of pathology in the older generation of family members appeared at the age of 40, then in children there is a high probability that the onset of an increase in symptoms of cerebral venous circulation will be observed at the same age. Genes have not yet been identified that can be inherited in a dominant or recessive way, and then provoke a similar disruption of the circulatory system of the brain in the next generation.
Classification
In medicine, this condition is divided into stages and subtypes. To make the correct diagnosis and correctly select effective therapy, it is necessary to establish the stage of the pathological condition.
There are three stages:
- Latent. It practically does not manifest itself with any symptoms, so a person who has such a pathological condition at this stage of development does not know about its existence. Even if minor symptoms appear, everything is attributed to fatigue. The patient does not experience severe headaches.
- Venous cerebral dyshemia. At this stage, the symptoms are quite vivid, however, they do not cause much discomfort for the person, because they occur periodically, and their nature is smoothed out.
- Encephalopathic is the most severe form of this condition. All the symptoms that appear greatly disturb the person, which prevents him from living a normal life. If the disease is not diagnosed at this stage and timely therapy is not started, then the condition may become irreversible.
What to do if symptoms of venous outflow disturbance are detected?
To explain it in accessible language, venous discirculation is impaired blood circulation in the human brain.
This disease is quite common, and there are many reasons for its occurrence. As for short-term blood flow disturbances, a person encounters them regularly: this is a common cough, daily sneezing, excessive physical activity, sudden turns of the head. If we consider permanent violations, they are due to more serious reasons.
”alt=””>
Modern man is not immune from such a phenomenon as cerebral venous discirculation. Experts note that short-term disturbances occur during normal physiological processes: coughing, singing, defecation, turning the head, physical activity. Therefore, we have all encountered, albeit for a short time, this phenomenon, without even knowing what happened.
Experts have been studying this disease for a long time and have identified three main stages:
- Latent stage. At this stage, clinical symptoms do not appear, and the person lives a normal life, without any special complaints;
- Cerebral venous dystonia, in which a typical picture of paraclinical changes is observed. The person exhibits some symptoms but can continue to lead a normal life.
- Venous encephalopathy with the development of stable organic microsymptoms. Here you will need the help of a specialist, otherwise the person’s normal life will be at risk.
If you have symptoms of the disease, do not panic. In the early stages, you can easily correct the functioning of the blood vessels in the brain. Moreover, sometimes it is enough to change the lifestyle that leads to a deterioration of the general condition in order to get rid of the disease. In any case, there is no need to delay, but if possible, turn to specialists. With their help, the necessary examinations will be carried out and a course of treatment will be prescribed.
It is hardly worth self-medicating and injecting medications every season, which, by the way, many doctors do to themselves. They believe that this is all due to bad weather or age (meaning non-specialized doctors who, by their specifications, do not come into contact with this disease in practice). This is partly true, but the “root of evil” is buried deeper and must be eradicated by taking a professional approach to the treatment process.