Fluid in the lungs after CABG
Signs of fluid accumulation in the lungs.
- Coughing and coughing
, up to prolonged bouts of coughing without discharge. It is especially typical with prolonged horizontal position of the body, during and after sleep. - When a person is lying down, extraneous bubbling, gurgling sounds can be clearly heard in their breathing.
- Shortness of breath occurs when lying down.
- Breathing is noisy and rapid.
Why does fluid accumulate in the lungs after CABG?
How to avoid fluid accumulation in the lungs after bypass surgery.
Walking.
Breathing exercises.
How to inflate balloons correctly?
How fluid is removed from the lungs.
Consequences of fluid accumulation in the lungs.
Conclusion.
- Fluid in the lungs in the field of CABG is a typical, predictable phenomenon.
- It can be avoided by actively doing breathing exercises (inflating balloons) and walking. Decongestants are used.
- If fluid still accumulates in the lungs, it is pumped out through a puncture, but this is only a measure to make you feel better. It does not eliminate the need for independent exercise.
- The consequence of prolonged accumulation of fluid is the development of pneumonia.
Popular articles
Pericarditis
Pericarditis is one of the most common cardiac surgical complications. Postoperative pericarditis is a severe, but almost inevitable, complication of cardiac surgery, but the degree of its severity very much depends on the characteristics of the surgical intervention (duration, traumaticity, etc.).
A highly informative non-invasive method for diagnosing pericarditis is echocardiography, which allows not only to detect the presence of effusion in the pericardial cavity, but also to analyze the nature of the location of the epi- and pericardium in various parts of the heart.
V. B. Pyryev et al. (1994) showed that with a small volume of fluid in the pericardial cavity, the echo-free space, as a rule, is noted only in the region of the posterior wall of the left ventricle. With pronounced accumulation of fluid (more than 250 ml), the echo-free space is recorded in both the posterior and anterior parts of the pericardial sac.
Complications after CABG. Disadvantages of heart bypass surgery.
Continuing the topic Should I do CABG?
Now it’s the turn of the negative aspects that you need to know about in advance. Nothing goes unnoticed, and even though bypass surgery in general has already become an almost routine operation, it is an order of magnitude more complex than stenting. The operation carries a certain risk and a whole range of complications. Operational risks.
The operation itself takes a long time. Usually 4-6 hours. In addition, it is most often done when the heart has stopped completely and the patient is connected to an artificial circulatory system. Cardiac arrest in an out-of-hospital setting means a single fatal outcome for a person. You can imagine the level of stress to which the brain and the entire body are exposed when it realizes that it has died and its heart has stopped. The heart will stop beating within 40 minutes to an hour. Such powerful stress is already a risk. In addition, the very word “risk” suggests some kind of emergency situation, of which there can be many. Meanwhile, despite all the risks, the percentage of operative mortality in CABG is less than one percent...
Which valves to install (video)
Russian industry produces many different products of the highest quality, which have no analogues in the world. Unfortunately, the same cannot be said about artificial heart valves.
Today, Carbomedics Tophead is considered one of the best mechanical heart valves. There are other excellent foreign analogues. Unfortunately, this cannot be said about Russian products - they are not so reliable, and they break down quickly. Therefore, if we are talking about a young patient, then it is better to pay more and get a European implant.
True, there is hope that soon, on the market of medical products, mechanical heart valves will appear that are not inferior and even superior in quality to foreign ones.
Alla-Maria
Heart bypass surgery for type 2 diabetes
What you need to know before surgery
CABG for type 2 diabetes mellitus?
Did you know that the mortality rate for diabetics after bypass surgery is lower
compared to stenting? What are the features of shunting for second diabetes?
Diabetes and atherosclerosis are inseparable friends? In fact, they are. The saddest complication caused by diabetes is the effect on blood vessels. All blood vessels are affected. They are exposed to excess glucose in what one heart surgeon described as being like being sanded. Small scratches on the inner walls of the arteries left by abrasives ultimately lead to inflammation and thinning. Gradually, the affected areas begin to become covered with a layer of cholesterol. The body, as it were, is trying to patch up the damaged surface in order to avoid a big disaster - rupture of the vascular wall and internal bleeding. This is how atherosclerosis appears. A disease in which the walls of the arteries become covered with cholesterol plaques. Plaques tend to gradually calcify,…
Briefly about emergency operations for myocardial infarction
The use of percutaneous coronary intervention (PCI) as an emergency treatment for myocardial infarction is urgent. The goal of primary PCI is to open the artery as quickly as possible, preferably within 90 minutes.
Another type of emergency surgery for myocardial infarction is coronary artery bypass grafting (CABG), which is usually performed to simultaneously treat mechanical complications such as papillary muscle rupture or ventricular septal defect accompanied by cardiogenic shock.
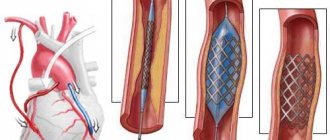
Bypass surgery and stenting of cardiac vessels, what is the difference?
Do you want to figure out what is better, what is the difference between bypass surgery and stenting? I experienced bypass surgery myself in 2014, and the more time passes, the more experience and practical knowledge accumulates, so get first-hand information! Stenting of cardiac vessels. The essence of the surgical procedure is to expand the problem area of the vessel (the one where the narrowing occurred due to plaque formation) by installing a special device - a stent.
Several stents can be installed, depending on the number of problem areas of the arteries that need dilation. Stents come from different materials, different sizes and different manufacturers. The stent is a durable mesh frame in the shape of a tube, the diameter of which can be increased after installation in a narrow place vessel. The operation is performed under local anesthesia. It only lasts a few minutes. Through an artery in the groin area or through an artery in the wrist area, surgical penetration occurs…
Pleural puncture
Oncologists use pleural puncture to diagnose and treat pleural cancer. It is intended for collecting pleural fluid for the purpose of cytological examination and reducing its content in the pleural cavity. Pleural puncture is performed if the following indications exist:
- Accumulations in the pleural cavity of inflammatory fluid (exudate and transudate), blood, lymphatic fluid;
- The presence of air in the pleural cavity;
- Formation of pus in the pleural cavity.
If bleeding is suspected in a patient, a Rouvilois-Gregoire test is performed during pleural puncture. If the blood obtained contains clots, it means that the bleeding has not stopped. After removing the contents, antitumor drugs are injected into the pleural cavity. To ensure the safety of the procedure, the puncture is performed under X-ray or ultrasound control.
Pleural fluid puncture is as safe as possible for the patient, provided that breathing is even and calm. Therefore, if the patient suffers from a cough or severe pain, before proceeding with the puncture, he is prescribed antitussives and painkillers in advance. Such measures significantly reduce the risk of complications during the procedure.
Make an appointment
How is the procedure performed?
This manipulation does not require the use of specific modern medical equipment. The puncture is carried out as follows:
- The patient is placed in a sitting position, facing the back of the chair, on which he rests with his hands. In the case of pneumothorax, the patient can also be placed in a lying position on the healthy side, with the upper arm pulled behind the head;
- The area of the upcoming puncture is covered with sterile diapers, and the skin is treated with antiseptics;
- An anesthetic solution is injected into the tissue. The doctor places a rubber tube about 10 cm long on the syringe, and not a special needle with a diameter of at least 1 mm. The needle is inserted above the upper edge of the rib and slowly advanced inward. As the needle is inserted into the tissue, an anesthetic is injected;
- After the needle falls into the pleural cavity, the doctor draws its contents into the syringe. In this case, primary diagnosis can be made already at the moment of fluid collection - by its color and nature. The liquid is pumped out using a syringe or electric suction (if a lot of liquid has accumulated);
- The liquid is collected in special sterile tubes for subsequent analysis;
- After pumping out the fluid, the patient’s pleural cavity is washed with an antiseptic solution and then an antibacterial drug is administered;
- The needle is removed, and the puncture site is treated with an iodine-containing preparation and sealed with a band-aid. After this, the patient is transported to the ward, where he must remain in a lying position for at least two hours.
To ensure that the procedure goes without complications, it must be performed by an experienced doctor. Leading Russian doctors practice at the Yusupov Hospital. All medical services in the hospital are provided at a high European level, each patient feels an individual and attentive approach to their problem.
Pulse after CABG
What happens to the pulse after bypass surgery? Probably after the operation, everyone who monitors his heart rate noticed his capricious behavior. The first week after surgery is particularly special in this regard.
I will share my personal experience. I also had to worry a little after the bypass surgery. It would seem that the operation was done so that the heart would feel better, so that its blood supply would return to normal, and accordingly, the pulse would return to normal, but it “jumps” up and down. True, the rest of the roommates had the same picture. This “collectivity” of the symptom somehow reassures you, you understand that since this is not only happening to you, then this is, if not normal, then at least a fairly common phenomenon. In fact, as the head of the cardiology department explained, the heart adapts to new blood supply conditions. The period of such adaptation was not announced, but from my own experience I can say that pulse jumps are becoming less and less frequent every day. I remember exactly that in...
Positive aspects, expected results
After a heart attack, not only bypass surgery can be used, but also stent surgery. Both methods are aimed at the same goal, but bypass surgery is considered the best.
The technique has the following advantages:
- high degree of efficiency;
- the ability to perform surgery with simultaneous damage to several vessels;
- minimum rehabilitation period;
- rare occurrence of serious complications;
- minimal list of contraindications.
Expected results:
- restoration of blood circulation, as a result of which the heart receives a sufficient amount of nutrients and oxygen;
- prevention of extensive and recurrent infarction;
- absence of angina pectoris;
- improvement of general well-being;
- restoration of performance;
- the ability to increase physical activity;
- reducing the risk of death;
- increasing the patient's life expectancy;
- abolition of drug therapy, after surgery only treatment with prophylactic drugs is used;
- return to normal lifestyle.
Safe exercise after CABG
The phrase “you can never have too much sports” actually has little to do with health. Just to improve the health of the body, moderate, but at the same time sufficient physical activity is needed. Where are the boundaries between “insufficient”, “excessive” (dangerous) and “moderate” load? Each person has their own boundaries, and you will have to find them yourself.
Let's divide this big question into several stages: Find a good cardiologist. Get examined and get recommendations. Start training. Constantly exercise personal monitoring of the state of the cardiovascular system. Periodically, at least once every six months, be examined by your doctor. 1. Find a good cardiologist. You need to find a specialist who has experience working with patients who have undergone CABG. It is in restoring health that doctors often have virtually no experience. Having provided emergency assistance, they let us go free. Meanwhile, consultations with a cardiologist...
Pulmonary edema after surgery
Causes of pulmonary edema
Disruption of normal gas exchange in the lungs and, as a result, accumulation of fluid can be caused by two main reasons: physiological and medicinal.
The physiological reason is as follows: performing an operation on an organ that affects the pulmonary circulation reduces the intensity of blood flow through it, stagnation of blood leads to the penetration of the liquid component of blood through the walls of blood vessels into the pulmonary alveoli.
Medication: During the postoperative period, medications are taken, some of which have a negative effect on the relationship between intrapulmonary pressure and hydrostatic pressure of the capillaries in the lungs.
There may be a violation of the norm of colloid-osmotic blood pressure due to the presence of medications in it. The result is impaired gas exchange and pulmonary edema.
Symptoms of pulmonary edema
Typically, symptoms of pulmonary edema after surgery appear suddenly. Difficulty breathing appears, the frequency of inhalations and heart contractions increases, and a dry, unproductive cough is characteristic.
Even in a half-sitting position, breathing does not become easier. Some time after the first manifestations of symptoms, a foamy mass is coughed up.
Treatment of postoperative pulmonary edema
Therapeutic measures are carried out in several directions:
- normalizing the pressure ratio in the gas environment of respirators and in small blood vessels;
- blocking processes leading to foaming and hypoxemia;
- suppression of the excited state and reduction of hyperactivity of the symptoadrenal system;
- reducing the load on the pulmonary circulation and lungs with fluid.
All these activities are carried out in a clinical setting and under the supervision of medical workers. To reduce foaming, inhalation of ethyl alcohol vapor through an inhaler is often used. The pressure ratio is equalized by an anesthesia machine under a certain pressure.
The excited state is relieved by intravenous administration of sedatives - midazolam, sibazone, droperidol or sodium hydroxybutyrate. The easiest way to reduce the load on the small circle is to apply venous tourniquets or pneumatic cuffs.
POSTOPERATIVE PULMONARY EDEMA
Pulmonary edema (PE) during and after surgery was until recently considered one of the most severe complications, a pulmonary manifestation of heart failure or hyperinfusion. Its occurrence is due to the transition of the liquid part of the blood from the pulmonary capillaries into the air spaces of the respirons due to a change in the normal relationships between the hydrostatic pressure in the capillaries and the oppositely acting intrapulmonary pressure, as well as colloid-osmotic blood pressure.
As a result of significant changes in these factors, the pressure gradient between the microvessels of the lungs and the gaseous environment of the diffusion zone of the lungs, which, in fact, represents the pulmonary interstitium, decreases.
An increase in the permeability of the alveolocapillary membrane under the influence of various humoral factors in complicated postoperative periods (BAS, other ETS), as well as the use of prolonged aspiration from the bronchial tree during its sanitation, contributes to the initial transition of intravascular fluid containing protein into the gaseous environment of the lungs. Water on the surface of the pulmonary diffusion membrane eliminates the surfactant properties of the lung surfactant (Johnson JWC et al. 1964), which sharply reduces lung compliance and increases energy expenditure for breathing.
The transition of significant amounts of surface-active phospholipid and protein into the liquid exuding into the lumen of the respirons contributes to the formation of persistent foam filling the air-bearing zone of the lungs, which is considered a manifestation of alveolar OJI (Luizada A.A. 1965). Filling the airways with foam further disrupts the distribution of gas in the lungs and extremely reduces the efficiency of pulmonary gas exchange with a significant increase in energy expenditure on breathing.
The specific genesis of early postoperative AL is complex. Hyperactivation of the sympathoadrenal system, especially with insufficient analgesia, an increase in the level of so-called traumatic mediators and MSM, an acute decrease in blood COP under the influence of excessive infusion of saline solutions against the background of plasma albumin deficiency, the direct effect of hypoxia and venous hypoxemia, acidosis, hyperenzyme on the permeability of pulmonary capillaries in combination with a decrease in cardiac performance - can be combined in each specific case of OL after surgery in various combinations.
Nowadays, most resuscitators are inclined to believe that the hemodynamic causes of early acute acute illness play a significant role only in patients with initial toxic or metabolic damage to the myocardium, concomitant valvular heart disease, or direct trauma to the myocardium during cardiac surgery.
Often, acute hypertension of the pulmonary circulation develops secondarily and can be associated with direct damage by factors of acute respiratory failure (hypoxemia, hypercapnia, acidosis) of the disabled heart muscle. This disorder clearly manifests itself against the background of increased systemic vascular resistance due to low BCC or, conversely, high blood pressure in the systemic circulation, which can be realistic in the immediate postoperative period. Early clinical observations of pulmonary surgeons A.D. Yarushevich (1955), I.S. Kolesnikova (1960) emphasize that the development of OA usually coincided with the period of greatest instability of pulmonary gas exchange in such patients: after lung resection, it occurred in the first hours and no later than the first day after the intervention.
Later postoperative OJI develops not only against the background of hemodynamic disorders (with a significant decrease in IOC), which is accompanied by other postoperative complications, such as bilateral pneumonia or pneumonia of a single lung, acute myocardial infarction.
OJI often result in severe protein deficiency with extreme hypoproteinemia, infectious-inflammatory endotoxicosis, or decompensation of concomitant hypertension due to cerebrovascular accident. Such OJIs develop slowly through a stage of interstitial edema with fluid retention in the peribronchial tissue. The intensity of water accumulation in the lungs largely depends on the magnitude of systemic blood pressure (hypertensive crisis) due to an increase in the rate of filtration of tissue fluid from the bronchial vascular system (Simbirtsev S.A. Serikov V.B. 1985).
Diagnosis of heart failure
If you have symptoms of heart failure, your doctor will ask you to describe them in detail and then examine you. Most likely, the doctor will suggest that you additionally take an ECG and measure the vital capacity of the lungs using a device called a spirometer (this will definitely tell whether shortness of breath is caused by CHF or some other lung disease).
Blood tests can help determine if your symptoms are caused by another condition, such as anemia, diabetes, thyroid disease, kidney disease, or liver disease. High blood cholesterol is often associated with coronary heart disease, which can lead to heart failure.
Your blood will also be tested for substances called natriuretic hormones. If the heart is under too much stress, it will release them into the blood. The analysis will reveal their elevated levels in the blood.
An echocardiogram (EchoCG) is a test that allows you to look at the structure of your heart in detail. Harmless, high-frequency sound waves are passed through the chest wall, which bounce off the heart and form an image of it (similar to how a doctor examines a fetus during an ultrasound during pregnancy).
During the examination, you will lie on your left side with your left hand behind your head. A special gel will be applied to the breast and an ultrasound probe (recording device) will be applied to it at various points between the ribs.
An echocardiogram provides a lot of useful information about the heart:
- how the heart valves work, are there any abnormalities in their structure;
- how the heart pumps blood (when the heart contracts, it forces blood to circulate throughout the body - this is called systolic function);
- how the heart relaxes between contractions (during this period the heart fills with blood - this is called diastolic function);
- are there any holes in the walls between the chambers of the heart through which blood can flow from one half of the heart to the other.
The most important thing that can be learned from an echocardiogram is how well one of the heart chambers, the left ventricle, pumps blood. It is thanks to its work that oxygenated blood is distributed throughout the body during a heartbeat.
A measure called left ventricular ejection fraction (LVEF) measures how much blood filling the left ventricle is pushed into the aorta when the heart muscle contracts. Thus, in a healthy person, during a heartbeat, about 60% of the blood filling the left ventricle is pumped out. If LVEF is below 40%, the heart is clearly working abnormally.
Sometimes your doctor may order special types of echocardiograms. They are described below.
Stress echocardiography allows you to see how well the heart works under additional stress. For example, you may run on a treadmill, exercise on a stationary bike, or you may be given a special substance that increases your heart rate.
Some patients with suspected heart failure are given a test called transesophageal echocardiography.
Ultrasound does not travel well through the lungs, which can make it difficult to visualize the heart through the chest wall. However, the heart is located just in front of the esophagus. A thin tube with an ultrasound probe at the end can be inserted through the mouth to examine the structure of the heart in much more detail.
You may be asked to have a chest X-ray to check for an enlarged heart and fluid in the lungs, which could indicate heart failure. X-rays will also help identify lung diseases that may cause shortness of breath.