Pacemaker - what is it?
A pacemaker is a device that regulates the heart rate. If the heartbeat is abnormal, it normalizes cardiac activity by generating electrical impulses.
It is a device consisting of:
- The battery is housed in a sealed case with titanium coating. It is sewn under the skin at the top of the chest. Its dimensions are 5-10 cm, weight no more than 50 g. Titanium alloy reduces the risk of device rejection to a minimum.
- A chip , also built into the body, which is responsible for analyzing and monitoring heartbeats.
- Electrodes (electro-catheters) placed in the chambers of the heart and connected to a battery. They conduct electrical discharges to specific areas of the heart. The number of electrodes varies from 1 to 3 depending on the type of device.
The battery life is designed to last from 5 to 15 years. Planned replacement of the housing occurs within a period of 3 to 12 years, depending on the period for which the device is intended to be used. The operation is performed under local anesthesia. The procedure lasts 15-20 minutes, the patient is discharged after a maximum of 2 days.
The diagram shows a pacemaker device.
Electrodes placed in the chambers of the heart usually do not require replacement and are connected to a new housing. Control visits to the doctor to determine the person’s health status and the quality of the device’s operation are carried out once every 2-12 months. The frequency of visits depends on the type of pacemaker model, battery capacity and time elapsed since surgery.
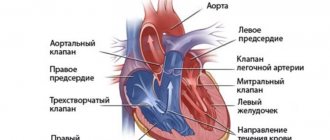
How does the device interact with the heart?
A pacemaker is a device that operates according to a certain principle. To normalize the functioning of the myocardium, electrical impulses are sent to certain areas of the heart using electrocatheters. Early models of devices operate in continuous mode, current pulses are sent constantly.
Modernized types of devices, with a normal heartbeat, are in a standby mode, from which they exit when the heartbeat rhythms are disturbed. If within the time specified by the program the myocardium does not begin to contract in the correct rhythm, the device switches to activity mode. Using electrical impulses, it restores normal heart function (work on demand).
Some models of pacemakers (pacers, pacemakers) have a tracking mode.
It allows you to collect data on the work of the heart, track such disorders as:
- ventricular fibrillation;
- atrial flutter;
- atrial fibrillation.
The collected information is transferred to doctors for further analysis. The battery power of this type of sensors is consumed faster.
Types of pacemakers
Devices are divided into only two types: standard and internal. An internal pacemaker is not only a standard device that stimulates the heart, but also a defibrillator. A built-in defibrillator involves applying an electrical current to the heart to restore proper contractions.
Device:
- can do more than just control heart rate;
- can restore heartbeat after a life-threatening arrhythmia occurs, which some call a “lethal rhythm.”
The meaning is the same as when performing this action manually, but the wires of the device are located inside and are connected directly to the heart. Because of this, the electrical shock is weaker and not too painful.
Standard pacemaker - Sends weak electrical impulses to the heart through wires that are attached to the heart. This helps with heart rhythm disorders when the heart is not able to send signals on its own.
Can you feel the pacemaker working?
Immediately after surgery, most patients experience unpleasant feelings from the operation of the device in its active mode.
They are perceived by a person as:
- feeling of buzzing in the chest;
- vibration;
- twitching and contractions in the chest;
The sensation may intensify during sleep when the patient lies on his side. The operation of the device can be felt during active physical efforts or emotional experiences. Over the course of 2 months, you gradually become accustomed to the operation of the sensor and the feeling of discomfort disappears.
Recovery after surgery
Rehabilitation after installation of a pacemaker usually lasts from a week to a month. Below are some tips on how to behave during the recovery period. You should find out more detailed information from your doctor. Only he can tell you in detail about the necessary lifestyle adjustments depending on the specific situation. What you should pay attention to:
- You should try to avoid lifting heavy objects and excessive physical activity. This will allow the postoperative wound to heal faster and the pacemaker to “fix.”
- Eliminate pressure after installing the pacemaker on the area where it is placed in the tissue.
- Tell your doctor if there is swelling, redness, or discharge from your surgical wound.
- Contact your doctor if your low-grade fever does not disappear within 2 days.
One of the complications of pacemaker implantation that can occur in the long term is swelling of the left upper extremity.
Wires directed from the device to the heart first enter a vein that runs upward along the chest wall. Through it they enter the vein through which blood flows from the upper limb. The wires then penetrate the superior hollow and the heart. They are quite thick, which can cause inflammation of the veins and their narrowing - this leads to congestion in the arm and its swelling.
When your arm hurts after installing a pacemaker, this may be one of the symptoms of inflammation of the vein. The condition is diagnosed using ultrasound or venography. The last procedure involves the introduction of a contrast agent. If the diagnosis is confirmed, this problem can be resolved with balloon angioplasty. Another option is to move the wires from the damaged vein to another.
To see how quickly the patient gets used to the pacemaker and what sensations he experiences, watch this video:
Types of pacemakers and special operating modes
A pacemaker is a device that can have several modes of operation. Since 1974, coding of device markings of 3-5 letters has been adopted.
Their designations:
| Letter 1 | Letter 2 | Letter 3 | Letter 4 | Letter 5 |
| Indicates the chamber of the heart being stimulated. | Sensitivity function. Indicates which camera. analyzed by the stimulant. | The type of reaction of the pacemaker to the received data on the activity of the analyzed cameras. | Indicates the type of pacemaker setting. | Multifocal myocardial stimulation. A function that allows you to stop an attack of tachyarrhythmia, perform defibrillation or cardioversion. |
| A – atrium (Atrium). V – ventricle (Ventricle). D – atrium with ventricle (Dual). | A – atrium. V – ventricle. D – atrium with ventricle. O – lack of sensitivity function. | I – blocking of generator pulses (Inhibition). T – triggering generator pulses (Triggering). D – blocking and starting (Dual). O – no reaction. | R – the ability to increase or decrease the frequency of impulses when changing motor activity (Rate-adaptive). | O – lack of function in the device. A, V, D - presence of a second electrode. |
Common stimulation modes:
| VVI | AAI | VVIR | AAIR | DDD | DDDR |
| 1-chamber, ventricular, on demand. | 1-chamber, atrial, on demand. | 1-chamber ventricular, on demand, with frequency adaptation. | 1-chamber atrial, on demand, with frequency adaptation. | 2-chamber atrioventricular biocontrolled. | 2-chamber atrioventricular biocontrolled with frequency adaptation. |
Permanently worn pacemakers are divided according to their impact zones.
1-chamber pacemaker
A pacemaker with 1 electrical catheter, which is attached to the atrium or ventricle. Early models generated pulses asynchronously, continuously, at a programmed contraction frequency. Modern 1-chamber stimulators operate on demand.
Their disadvantage is that the contractions of the atrium and ventricle may periodically coincide, and in this case the blood from the ventricle enters the atrium and the veins of the heart.
Implantation of devices with 1 electrode is indicated only for permanent atrial fibrillation and sick sinus syndrome (SSNS). In other cases, preference is given to an pacemaker with a number of electrodes of 2 or more.
2-chamber pacemaker
When installing this model of stimulator, 2 electrodes are attached to the heart. With such stimulation, the rhythms of the ventricle and atrium are coordinated, the physiological heart rate is maintained, which guarantees proper blood flow in the heart, complete filling of the vessels with blood and patient comfort.
Common electrode mounting:
- in the atrium and ventricle (atrioventricular stimulation);
- in the right atrial appendage and in the coronary (coronary) sinus of the heart (biatrial stimulation);
A 2-chamber pacemaker may have a frequency adaptation function. In the labeling, it is designated by the letter R. The function allows you to change the frequency of rhythm control and program the duration of the atrioventricular delay.
Pacemakers with frequency adaptation will allow you to engage in sports such as swimming and running. However, additional device options lead to a shorter battery life. However, additional device options lead to a shorter battery life.
A 2-chamber pacemaker is implanted when:
- pathologies with a decrease and increase in heart rate;
- bradycardia with a pulse below 40 beats/min;
- severe disturbances of myocardial contractile function during physical activity;
- carotid sinus syndrome;
- atrioventricular (AV) block of degree 2 or higher;
3-chamber pacemaker
Devices with 3 electrodes stimulate 3 cardiac sections (atrium and two ventricles). Stimulation occurs in a certain sequence, ensuring the natural movement of blood through the chambers of the heart. The configuration of the device allows it to be operated in 1- or 2-chamber pacemaker mode.
Often the pacemaker is equipped with a touch sensor and has a frequency adaptation function. Sensors take readings about the respiratory rate, processes of nervous activity, and the patient’s temperature. Based on these data, the optimal pacemaker mode is selected.
The sensor is implanted when:
- Cardiac dysfunction (resynchronization).
- Dyssynchrony of the heart chambers against the background of bradyarrhythmia or severe bradycardia.
- Rigid sinus rhythm, provoked by depletion of organ reserves.
Temporary pacemaker
To prevent deaths from cardiac arrhythmias, a temporary pacemaker is used in medical practice.
It is installed when:
- Myocardial infarction.
- Arrhythmias.
- With right ventricular infarction and uncoordinated contraction of the atria and ventricles.
- Absolute blockade.
- For type I atrial flutter.
- Supraventricular tachycardia with the participation of the AV node and sustained monomorphic ventricular tachycardia.
- Slow heart rate combined with fainting.
- Ventricular tachycardia against the background of bradycardia and other life-threatening pathologies.
The device is installed by a resuscitator. Device installation methods:
| Endocardial | A catheter is first secured in the central vein and through it the electrodes are passed into the chambers of the heart. To exclude pneumothorax (accumulation of air in the pleural cavity), the patient is given an x-ray. Installing the electrode takes a lot of time and requires trained specialists, but this method is recognized as the most effective. |
| Through the esophageal | The electrode is inserted into the esophagus and installed in it at the level of the atria. The method is not effective for AV blockades. |
| Transcatoral (external) | The electrode is attached externally to the chest. The method is used as prophylaxis in case of likelihood of proarrhythmic complications, or as an emergency measure in critical situations. This method uses long and powerful pulses of electric current (200 mA), which causes severe pain to the patient. Pacing is carried out after anesthesia or immersion of the patient in a sedative state. |
Pacemaker defibrillator
Pacemakers of this type are designed to detect and eliminate ventricular fibrillation, which in 5% ends in clinical death. In normal mode, the device monitors the heartbeat and normalizes it. When an arrhythmia occurs, the device generates low-energy discharges that restore the normal heartbeat rhythm.
After the attack is removed, the device switches to monitoring mode.
Sensors are implanted for the following diseases:
- Congenital heart defects.
- Heart attacks that harm the heart's electrical system.
- Long QT syndrome.
- Brugard's syndrome.
- Sudden cardiac arrest and the risk of its recurrence.
Indications and contraindications for installation
A pacemaker is a device whose implantation may be delayed in a patient due to:
- Acute infectious and viral diseases.
- Acute course of chronic diseases.
- Mental disorder in the acute period.
There are no strict restrictions on installing a pacemaker. Before implanting the device, the doctor decides on the validity of this procedure.
Indications for sewing in the device can be divided into:
| Absolute | Relative |
| Episodes of asystole according to ECG lasting more than 3 s. Recorded heart rate, with physical activity, less than 40 per minute. Three-bundle blockade in the His system. Second degree AV block due to symptomatic bradycardia. | AV block of the third degree with a heart rate at a load above 40 beats/min., without clinical manifestations. The presence of 2- and 3-bundle blockades, without ventricular tachycardia and transverse blockades, accompanied by fainting. AV block of type 2 and degree II in the absence of clinical manifestations. |
If there are absolute indications for installing a stimulator, contraindications are no longer taken into account. The procedure for implanting a stimulator is carried out as planned or urgently. In case of relative indications for installing a pacemaker, the decision on surgery is made individually, taking into account the physical condition of the patient.
Patient reviews
I am 55 years old, I had an EX 452 pacemaker installed 3 years ago in DDD mode. I go to the doctor every six months, sometimes more often. During this time, only the electrode was changed.
I am 66 years old and have had a pacemaker for 8 years. Or rather, two in turn - the second one was reimplanted 3 years after the implantation of the first pacemaker. I lead an active lifestyle, I am a former athlete. Almost nothing has changed with ECS - jogging, active rest. There is no need to dwell on the disease, you need to live. And when there are failures, doctors promptly fix the problem. I would like to note that my heart does not beat on its own - only the pacemaker works.
Does anyone know what the life expectancy is with a pacemaker? Implanted a year ago, all this time the fear that it will turn off, the batteries will run out, something will happen... I’m already tired of living in fear!
If you are afraid, then you can get health problems from fear. It seems to me that now the devices are so technically advanced that it is simply stupid to be afraid. Well, a person in his life does not feel a panicky fear that his heart will take - and stop? There are all sorts of cases. And a person with a pacemaker is more protected from any misunderstandings - the work of the heart is controlled by a smart device. I have had ECS for 6 years, I follow the rules of a healthy life - and I am not afraid of anything.
In 2009, I gave birth to a daughter with an electric pacemaker - they installed the device right before giving birth. Now I’m used to it, I don’t even notice, in everyday life and at work (I’m a teacher) there have been no changes - everything is the same as before. So live a healthy life, enjoy life and don’t be afraid of anything - everything will be fine!
I had a blockade of the 2nd degree, type 3. A pacemaker was installed a year and a half ago. I live as before, I even run, I graduated from college, I work in production - no problems. I used to be afraid of everything, the biggest fear was to die, that my heart wouldn’t stand it. And with the stimulant, this fear went away. I would also like to say about the operation itself - the seam is almost invisible, nothing sticks out outwardly. Don’t be afraid and use a stimulator – it significantly improves your quality of life!
We suggest you read: Tachycardia after a glass of alcohol - All about hypertension
Pre-installation inspection
A pacemaker is a device that requires a thorough examination of the patient before installation. This minimizes risks and reduces the likelihood of postoperative complications. The following diagnostic tests may be prescribed to the patient before surgery.
Mandatory:
- Ultrasound of the heart.
- ECG.
- Daily Holter monitoring.
Additional examinations:
- ECG under load.
- Chest X-ray.
- Coronary angiography.
- Dopplerography (USDG) of the brachiocephalic arteries.
- Electrophysiological study of the heart (EPS).
Tests prescribed before installing the stimulator:
- Detailed blood and urine analysis.
- HIV.
- Hepatitis B and C.
- Syphilis.
How is the pacemaker implantation procedure performed?
The operation takes place in the X-ray operating room with the patient fully conscious. He is given an anesthetic injection in the collarbone area. An electrode is inserted through an incision in the skin and subclavian vein, which is then carefully advanced towards the heart. The movement of the special electrode is monitored using x-rays.
To find the optimal location for fixing the electro-catheter, a cardiogram is made after each possible attachment point. Next, the wire is fixed in one of the chambers of the heart. If additional electrodes are available, all manipulations are repeated through the same incision.
A bed is formed in the thickness of the pectoral muscle, and the ECS body is placed into it. The vessels and skin are sutured, and an aseptic bandage is applied to the incision site. The operation lasts from 40 minutes to 2.5 hours. Its duration depends on the number of electrocatheters on the device
The operation and its duration
This operation is minimally invasive (small) and is performed under local anesthesia. But the operating room must have an X-ray machine.
Before the operation, anesthesia is performed, the duration of which rarely exceeds 40 minutes. This is enough to make an incision in the chest and insert an electrode into the desired area of the heart. In case of installation of two- or three-chamber devices, the procedure is repeated with the remaining cavities of the heart.
Setting the pacemaker
The doctor then programs and tests the device. After a trial ECG, if it satisfies the surgeon, the stimulator body is fixed under the skin of the pectoral muscle or in the subclavian region. After which the tissues are sutured and sutures are applied.
In some cases, the pacemaker is installed in the abdominal area. Guided by the results of examinations, the characteristics of the disease and individual nuances, the doctor determines how the pacemaker is installed.
Features of the operation at different ages
The operation to install an pacemaker is performed the same for people of all ages.
However, due to age-related changes in the body of older people, there are several features:
- The dosage of painkillers may be increased, since people over 55 years of age have a lower pain threshold.
- Due to the fragility of the tissue, more attention is required from the surgeon to avoid piercing the walls of the heart.
- In old age, muscles have a tendency to fatty degeneration, sclerosis - the replacement of muscle tissue with connective and fatty tissue. This leads to an increase in the stimulation threshold and an increase in the strength of electrical impulses necessary to contract the heart muscles. If the tissue at the site of electrode attachment is sclerotic, the pacemaker battery charge is consumed faster.
Complications during surgery
Due to the fault of the implantologist:
Sterility of dental instruments is a necessary condition for safe surgery
- Infection of the hole due to insufficient sterility of instruments;
- incorrect selection of pin;
- violation of the rules of preoperative preparation;
- installing an implant on insufficiently dense bone, refusing bone grafting and sinus lifting;
- injury or overheating of the bone;
- violation of sterility;
- ignoring contraindications.
Damage to the maxillary sinuses
Injury to the maxillary sinus can occur due to erroneous determination of the height of the alveolar process or too much pressure on the instrument. In this case, the implant is removed and drug treatment is carried out. The next attempt at implantation is carried out no earlier than 6 months later.
Damage to the mandibular nerve
The risk of damage increases when implanted above the mandibular canal, in cases where the bone is not dense enough. In this case, bone grafting (tissue augmentation) is first performed. The injury can cause facial numbness and drooling from the mouth.
Postoperative period
Recovery after surgery in the hospital takes 4 to 10 days. In the first days after surgery, pain will persist at the incision site, which is relieved with analgesics.
Possible postoperative complications:
- Swelling and hematomas in the operated area.
- Hemorrhagic complications.
- Infectious complications.
- Air in the pleural cavity.
- Blockage of blood vessels and, as a result, poor circulation.
Postoperative complications occur in less than 5% of cases.
How to determine whether the ECS is working correctly?
The first check is scheduled 2 days after surgery. If there are heartbeat disturbances or the possibility of their development, a re-check is done after 15 days. After discharge, the functioning of the stimulator is checked after 1 month. Next come scheduled inspections every 2 months for 3-7 years.
Further checks become more frequent up to 1 per month, and the remaining battery reserve is monitored.
When diagnosing, use:
- Electrocardiograph. ECG data measures coronary blood flow and spontaneous rhythm of contractions.
- A device for programming the stimulator chip is used to adjust the settings.
- An impulse duration meter and a stimulus frequency analyzer check how signals from the heart are perceived and ECS impulses are generated, and the heartbeat rhythm is analyzed.
- The position of the electrode is determined using radiography.
- The remaining battery capacity is checked with a special magnet.
In the absence of these devices, it is impossible to accurately assess the operation of the device. At home, doctors recommend using a wrist heart rate monitor and focusing on your own well-being.
Can I work and play sports after installation?
If the postoperative period passes without complications and the pacemaker works well, most patients return to their previous work duties, but taking into account new circumstances.
Recommendations from specialists regarding the work activity of a patient with a cardiac pacemaker:
- The attending physician must be notified if the patient’s work activity involves the operation of electrical appliances and electrical equipment under high voltage, very strong industrial magnets, radars, and other sources of electromagnetic radiation.
- Colleagues of a patient with a pacemaker should be aware of this fact and have coordinates and first aid instructions in case of ventricular tachycardia and any emergency situations with the patient’s health.
- Just as in everyday life, a person with ECS must avoid working with excessive physical stress, as well as the risk of falling, blows to the chest and heart, and overstraining the chest muscles during physical labor. If before the operation the patient had harmful working conditions that fall into the categories of the above types of work, he needs to change the type of work activity and switch to easier work.
Can a person with a pacemaker play sports?
There is an opinion that a person with ECS cannot engage in any type of physical exercise - this is not true. Moreover, light sports and some physical exercises are very beneficial and strengthen the heart and blood vessels, stimulating the body to function normally.
Before starting any sport, you must obtain recommendations from your doctor regarding the amount of exercise, time of exercise and the appropriateness of the chosen physical exercises.
The following sports and exercises are prohibited for a person with a pacemaker:
- All sports involving direct contact and risk of impact. For example, game sports - hockey, football, as well as martial arts - taekwondo, karate.
- Shooting from a shotgun and rifle - the recoil of the weapon at the location of the stimulator can damage the tissue above the device, as well as mechanically affect the pacemaker itself.
- Scuba diving, diving to any depth, diving.
- All sports associated with lifting weights, concussion of the shoulder girdle, risk of falls and blows to the chest area - high jumps, boxing, barbell.
During physical exercises recommended by the doctor, the patient should focus on his own well-being and stop exercising as soon as alarming symptoms or fatigue arise.
During physical activity and outdoor recreation in the warm season, it is necessary to protect the stimulator area from direct sunlight.
Rehabilitation
During the first days after surgery, you should limit your homework; if you feel tired or have discomfort, you should stop and rest. Lifting weights of more than 2 kg can cause postoperative sutures to come apart. Loading the upper body is prohibited for 1-3 months.
Sharp raising of arms up and to the sides is prohibited. During this period, only therapeutic exercises recommended by the attending physician are allowed. It is required to follow doctors' recommendations for caring for a postoperative wound. You can’t get it wet or pick off the sores. If rehabilitation proceeds without complications, 5 days after surgery you can take a warm shower.
Is it possible for a person with a pacemaker to work on a computer, make cell phone calls, and do ultrasounds?
Modern stimulants impose very few restrictions on the patient's life.
The implantation of a pacemaker in itself does not prevent a person from living a normal, ordinary life. The only thing is that in the first 3-4 months you need to reduce the load on your hand (usually the left) in order for the wound to heal. And then any load is possible, naturally, within reasonable limits. There is no need to perform feats, but going to the store, cleaning, washing, sweeping the floor - all this is within the capabilities of a person with an artificial pacemaker.
A special note for fanatical gardeners: do not grab a shovel immediately after the operation. But in six months - just right. But again: the work should be moderate. If a person is tired, he should rest. Not because the stimulator is overworked - nothing will happen to it, but excessive load on a diseased heart can lead to bad consequences.
After all, the electrical device doesn’t care what a person is doing: lying, sitting, running. The heart is primarily responsible for overall blood circulation. And the amount of load permissible for the patient depends, firstly, on the underlying heart disease, and secondly, on how advanced the device was installed.
Complications in the long term
The risk of complications with long-term use of a pacemaker is no more than 7%.
List of possible complications:
- Pastosity of the upper limb from the side of the pacemaker installation.
- Increased fatigue during exercise.
- Systemic infection.
- Displacement of the cardiac sensor relative to the bed.
- Inflammation and suppuration in the bed.
- Displacement of electrocatheters and inflammation at the site of their junction with the tissues of the heart.
- Deep vein thrombosis.
Life with a pacemaker
When implanting a permanent pacemaker, you must follow a number of medical restrictions and recommendations for life.
Limitations in daily life
- The area of the body with the implanted device must not be exposed to direct sunlight; it must be covered.
- It is prohibited to stay near electrical substations, high-voltage lines and cables.
- Do not approach satellite dishes, TV towers, or radar stations.
- Do not go through metal detectors.
- Do not perform types of work associated with muscle tension in the upper body - carrying loads, chopping wood.
- Impacts and pressure on the operated area should be avoided. Do not try to move the device by hand.
Use of household appliances, electronics, tools
- You should get into the habit of not touching electrical appliances, sockets, wires with the hand on the side of which the pacemaker is located.
- Use only grounded and insulated power tools. Telephones, microwave ovens, audio players, in any mode, must be at a distance of at least 0.3 m from the pacemaker.
- You should refrain from working with vibrating tools - hammer drill, lawn mower, drill.
Physical education and sports with a pacemaker
After the rehabilitation period, patients are allowed moderate physical activity. Traumatic, contact and active sports are not allowed.
| Forbidden | Allowed | Limited |
| Trampolines. | Race walking. | Cross-country skiing. |
| Sambo, judo, karate. | Yoga. | Volleyball. |
| Parachuting. | Classes in the pool. | Small towns, baseball. |
| Weightlifting. | Pilates. | Shooting. |
Limitations in professional activities
After the surgical intervention, the patient may be assigned a disability of group II-III.
Prohibited types of work:
- Welder (minimum distance to the welding machine 61 cm)
- Loader
- Electrician and electrician.
Prohibited medical procedures
Before performing any medical procedures, you should consult your doctor in advance.
Strictly prohibited manipulations:
- Electrophoresis
- Warming up.
- Magnetic resonance imaging
- Magnetotherapy
Pacemaker and electromagnetic devices
There are also some restrictions associated with the possible exposure of the device to magnetic and electromagnetic fields. Currently, all devices have fairly reliable protection from electromagnetic fields, and the use of devices and technology that surrounds us in everyday life does not require any special restrictions. This applies to computers, microwave ovens, and mobile phones. It is not recommended to carry a mobile phone in your breast pocket.
However, this or that powerful impact may disrupt the operation of the implanted device or cause harm to the patient.
Replacing components or the pacemaker itself
When the battery life is approaching, the device gives a signal during a routine inspection. After this, the ECS housing must be replaced. This operation, in the absence of complications, lasts 20-40 minutes. The electrodes are usually left in their normal operating condition.
Replacement of electrodes is required in the following cases:
- Inflammatory processes at the place where the wire is attached.
- Their dislocation and mechanical damage.
In this case, the doctor makes a decision to disconnect the old core and remove it, or leave it and insert a new one. Up to 5 electrodes can be located in the heart at the same time, without disrupting its functions. The operation with the replacement of electro-catheters and housings requires from 1.5 to 2.5 hours.
Programming (checking) the pacemaker
Technological progress in the development of pacemakers (pacers) has advanced far enough to significantly expand the available indications for their installation. Today, cardiac pacing is used not only in cases of cardiac arrhythmia, but also in a number of other diagnoses that are in no way related to arrhythmias.A modern pacemaker is an innovative programmable medical device that has not only therapeutic, but also diagnostic functions and capabilities. Checking the pacemaker with mandatory debugging of the settings is carried out on a regular basis. Careful control over the stimulation produced is an important part of the entire therapeutic process for a patient with an implanted pacemaker, and the organization of adequate work of the dispensary observation service for such patients has become one of the main goals of modern healthcare. For such control to be of high quality, it is necessary, at a minimum, to provide medical institutions with qualified personnel and equip them technically at the proper level.
With the introduction of technological innovations, almost every year new pacemaker models become available to cardiologists. This presupposes the uniform acquisition of a fairly large amount of specialized medical knowledge. In addition to general information regarding cardiac stimulation, physicians need complete and detailed knowledge of specific types of pacemakers, programmers, electrodes, etc. The programmer not only allows for programming the pacemaker, it is also an important part of the control system. Thanks to such a device, you can access the pacemaker, analyze the stimulation system and set the program. Traditionally, manufacturing companies produce their own programmer models that are incompatible with ECS produced by other companies.
The minimum set of technical equipment includes:
- electrocardiograph (preferably multichannel), equipped with a monitor;
- programmers (based on the various brands of pacemakers used in the medical institution);
- pulse duration tester - it allows you to check the operation of domestically produced pacemakers that do not have a telemetry function;
- stimulation frequency analyzer;
- magnet;
- external defibrillator.
Even though the basic principle of operation of all pacemakers is common, devices of the same type from different manufacturers differ in their own specifics: their functions and programs can be implemented in different ways. Therefore, an electrocardiogram taken from a patient with a normally functioning stimulation system may often seem unusual, which is mistakenly interpreted as a failure in the stimulation system. Without understanding the established pacemaker program and the way to implement its functions, interpretation of the patient’s cardiogram is difficult and sometimes completely impossible. Based on this, special rooms should be created to monitor the stimulation system in patients with pacemakers, and clinics that implant pacemakers should be used.
Testing of pacemakers in Moscow is carried out on the basis of the Moscow Cardiac Stimulation Center, where there are special rooms for monitoring patients with installed Russian pacemakers and foreign-made devices. Every year, about 3,000 patients pass through the center who want to check their pacemaker in Moscow and make sure it is working well.
Why is it necessary to check the operation of a pacemaker?
An pacemaker implanted in a patient is not only a medical device, but also a foreign body, on the correct operation of which the quality of life of the patient, and sometimes life itself, depends. That is why such patients require constant monitoring. Monitoring a patient with a pacemaker is not just a check of the pacemaker, but an objective assessment of the operation of the entire stimulating system, which consists of three important components:
- Patient's heart.
- Electrodes.
- Electrocardiostimulator.
What does the verification process consist of?
Checking the pacemaker's performance involves assessing the condition of each of these components. The main control tasks can be reduced to the following points:
- analysis of the current functionality of the pacemaker and its electrode (or several), allowing timely identification and elimination of possible stimulation disturbances;
- assessment of the correctness of the choice of stimulation program with the ability to adjust program parameters and their values in order to optimize stimulation according to the patient’s needs;
- assessment of the functionality of the power source and optimal adjustment of its energy parameters (allows not only to extend the life of the stimulator, but also to respond in time to the need to replace it);
- timely detection and elimination of complications caused by the stimulation process, but not directly related to true disturbances in the functioning of the system;
- educational work with the patient.
A functional test of the stimulation system involves not only taking a “passive” electrocardiogram (the generally accepted option), but also recording the patient’s ECG using provocation tests, as well as additional diagnostic functions and techniques (determined by the specifics of a particular model), which allow adequately analyzing the operation of the stimulation system and optimizing programming of pacemakers of this type.
What is included in the scope of work?
The scope of the check is directly determined by the model and type of pacemaker, but there is a single examination algorithm for all systems:
- interviewing the patient with subsequent analysis of the symptoms obtained;
- assessment of the condition of the stimulator placement site;
- general analysis of the patient’s ECG (including assessment of coronary circulation and spontaneous rhythm);
- assessment of perceptual and functioning function;
- assessment of the current state of the power source;
- assessment of the functional state of the electrode (if provided for by the model);
- assessment of the adequacy of specified treatment parameters and diagnostic functions;
- if necessary, assess the ventriculoatrial (VA) conduction and stimulant dependence of the patient;
- assessment of atrioventricular (AV) conduction during isolated atrial stimulation;
- reprogramming of current parameters based on data obtained after the survey.
Provocation tests
There are quite a lot of provocation tests suitable for checking: the specific choice is determined by the patient’s clinical situation:
- the position of the electrode is revealed by changing the position of the body in space and holding the breath;
- myopotential inhibition - special movements and tension of the pectoral muscles;
- determination of frequency response - tests with loads, etc.
Additional manipulations
Additional diagnostic procedures include:
- radiography (allows you to visualize the position of the electrode and assess its integrity);
- stimulation of the patient’s chest with an external pacemaker (allows inhibition of the implanted one);
- transesophageal recording of atrial potentials;
- displacement of the pacemaker in the bed (allows us to identify damage to the electrode in close proximity to the pacemaker or contact disturbances at the junction of the electrodes with the stimulator);
- magnetic verification of excessive perception of signals (so-called Oversensing), etc.
It is very important to interview the patient as thoroughly as possible and analyze his complaints. Analysis of the symptoms obtained allows us to adequately establish their relationship to the stimulatory system. Quite often they are associated only with the patient’s underlying disease, but it is important not to miss rare specific signals indicating certain dysfunctions of the stimulation system. This will allow you to suspect a problem even before conducting a full examination to identify pacemaker syndrome, myopotential inhibition, or violation of the integrity of the electrodes (if there are complaints of discomfort in the area of the pacemaker bed). The patient’s complaints will allow us to outline a plan for an objective examination and select adequate diagnostic procedures and provocative tests.
Inspection of the EX bed
One of the main problems of cardiac stimulation is the development of an inflammatory process in the area of the pacemaker bed. Thanks to the reduction in the overall dimensions of stimulators and the constant improvement of implantation techniques, the statistics of infectious complications have improved significantly in recent years (the figure varies between 0.5-5%). Often patients do not attach importance to the first (usually minimal) signs of a bedsore or inflammation: hyperemia (change in color saturation) or cyanosis, thinning of the skin directly above the site where the pacemaker is placed. These symptoms do not always develop in the early postoperative period, sometimes making themselves felt a considerable time (months and even years) after the introduction of the stimulant.
Visual inspection of the scar and pacemaker bed allows you to detect a bedsore at the location of the stimulator or its electrode, as well as predict its development. It is important to detect such changes in time - this will prevent perforation of the bed and/or the development of purulent inflammation.
General assessment of the electrocardiogram
ECG assessment involves the analysis of spontaneous and artificially provoked intervals and complexes. For this purpose, the ECG is recorded in twelve leads. Quite often, only standards are written down: based on an assessment of the temporal characteristics, the perceptual function of the stimulation system and its effectiveness, sometimes such an approach is justified. However, a routinely recorded electrocardiogram usually provides the most detailed picture.
Read more »
Assessing the condition of the power supply
The lifespan of high-quality operation of the pacemaker directly depends on a significant number of external factors taken into account: the frequency of stimulation, the magnitude of the energy impulse, the ratio between spontaneous and imposed rhythm, etc. The duration of the pacemaker operation can be calculated individually, based on data on the condition of the battery. It is important to adequately assess the state of the power source - this is one of the main points in controlling the stimulation system.
Read more »
Electrode condition assessment
As part of a stimulator circuit, a properly functioning electrode provides maximum effective stimulation. In most cases (statistics say about 80%), disturbances in the functioning of the stimulatory system arise due to an unsatisfactory condition or other problem associated with the electrodes. Speaking about a qualitative assessment of their condition, it is assumed that the integrity of the electrodes is directly assessed.
Read more »
Analysis and evaluation of diagnostic and additional therapeutic functions
Modern pacemakers are distinguished by a rich range of special therapeutic and diagnostic functions. Options for basic pre-installed special functions are determined by the model and manufacturer of the ECS.
Read more »
Why is it important to know the type of electrode installed?
Today, a large number of bipolar pacemakers are implanted, not always equipped with bipolar electrodes. When installing a monopolar electrode in tandem with such a device, if the bipolar configuration is set, the stimulation will not work effectively.
Why is it important to know the stimulated chamber (stimulation application point)?
The most indicative situation is the occurrence of idle stimuli against the background of developing atrial fibrillation. If the point of application of stimulation is the atrium, this picture is considered normal. If the stimulated chamber is the ventricle, then such a phenomenon is regarded as a disorder in the stimulatory system.
Based on all of the above, we can conclude that it is necessary to carefully prepare medical documents for a patient with an implanted pacemaker.
How often is monitoring of the stimulant system necessary?
The initial check is always carried out only in a hospital. If the patient is discharged (including if there are problems that do not require re-operation), the timing of subsequent checks is individually set for him. In the case where no errors are detected in the operation of the stimulation system in stationary conditions, subsequent control measures can be planned as follows:
- First check (1.5-3 months after implantation). This time period is due to the formation of a chronic stimulation threshold: it is at this time that all energy parameters of stimulation can be finally adjusted. Postoperative adaptation is completed, which allows you to adjust the parameters of frequency adaptation.
- Repeated checks (during the first year after surgery, at 6 and 12 months). Medical observation will make it possible to verify the adequacy of the chosen therapeutic tactics and the specified settings and stimulation parameters.
- Checks related to the end of the service life of the device - in conditions of a gradually discharging battery. Such checks should be carried out at shorter intervals: their frequency is determined by the presence of stimulant syndrome (dependence) in the patient and allows not to miss the time for the recommended replacement of the device.
How is the moment of reducing the interval between current checks determined?
Each manufacturing company provides estimated service life (average) for all released pacemaker models, based on basic stimulation parameters. But these deadlines should not be the only criterion.
Read more »
Authoritative opinion
Academician Amosov, who actually knew what a pacemaker was, said this: “It’s a pity, but there is a fundamentally wrong opinion that a person with a pacemaker is obviously disabled and must take care of himself constantly. This is wrong!". Implantation of a pacemaker is carried out solely to correct diagnosed bradycardia, which determines the general condition of the patient. ECS, while correcting bradycardia, does not solve all the problems associated with the underlying disease.
However, inserting a pacemaker literally works wonders. In addition to relieving unpleasant symptoms (loss of creation, etc.), many patients, while using ECS, note a significant improvement in their overall well-being - this allows them to live a full, active life.
return to the list of materials in the “SERVICES” section
How much does it cost to install the device?
The cost of an pacemaker device depends on its model and manufacturer. The most affordable Russian-made pacemakers. Most often, pacemaker implantation operations are carried out under a quota and within the framework of the compulsory medical insurance program.
Approximate cost for devices of different models and their installation:
| Model | Cost, rub. |
| EX made in Russia | |
| 1-chamber without frequency adaptation, without on-demand mode | 10500-2500 |
| 1-chamber with frequency adaptation, on-demand mode function | 25000-55000 |
| 2-chamber | 80000-25000 |
| 3-chamber | From 250000 |
| EX imported | |
| 1-chamber with frequency adaptation, on-demand mode function | 80000-100000 |
| 2-chamber | 160000- 450000 |
| 3-chamber | From 450000 |
| Electrode made in Russia | From 1500 |
| Imported electrode | From 2500 |
| Implantation of pacemaker without the cost of the device and electrodes | |
| 1-chamber | 20000 |
| 2-chamber | 26000 |
| 3-chamber | 31000 |
| Implantation of pacemaker complete with electrodes and introducers | |
| Biventricular, with delivery system | 514500 |
| DR with frequency adaptation | 326000 |
| DDD without frequency adaptation | 210000 |
A pacemaker is a device that will improve the quality of life and prolong it. The need for such an operation is determined by a cardiologist-arrhythmologist. He also selects the model and mode of the device individually for each patient.
Medical procedures prohibited after device installation surgery
Each patient who has a pacemaker has a special document in his hands - a certificate identifying him as a person with a pacemaker. This certificate contains information about the type of device, as well as the contact information of the treating physician.
This certificate gives the patient the right, for example, not to go through metal detectors at airports, or to refuse medical services that are prohibited to a person with ECS:
- Magnetic resonance imaging (which, if necessary, to examine a person, can be replaced with X-ray diagnostics or computed tomography).
- Ultrasound – if the device’s sensor must be passed over the area where the pacemaker is placed.
- Monopolar electrocoagulation (while bipolar coagulation can be performed in some cases if the doctor allows it).
- Lithotripsy.
- Some types of physiotherapy - for example, electrotherapy, magnetic therapy.
We suggest you read: How to lower blood pressure during bradycardia
It should be noted that echocardiography and ultrasound examinations outside the pacemaker area are not prohibited.