The structure of platelets
Small platelets of blood are responsible for blood clotting. They are the smallest elements and are 2-3 microns, do not have a cell nucleus and DNA, and therefore cannot arise as a result of cell division. Their shape resembles a colorless disk. There are 250 million platelets in one liter of blood. From production in the bone marrow to excretion, they circulate in the body for seven days.
The cells are formed in the bone marrow by megakaryocytes. With a diameter of about 150 microns, these giant cells are among the largest. Bone marrow cells gradually shed small fragments, which then enter the blood as platelets. Although they do not have a core, they perform many functions.
Participation in the folding [edit | edit code ]
A special feature of the platelet is its ability to activate - a rapid and, as a rule, irreversible transition to a new state. The activation stimulus can be almost any environmental disturbance, even simple mechanical stress. However, the main physiological activators of platelets are collagen (the main protein of the extracellular matrix), thrombin (the main protein of the plasma coagulation system), ADP (adenosine diphosphate, appearing from destroyed vascular cells or secreted by the platelets themselves) and thromboxane A2 (a secondary activator synthesized and released by platelets; its additional function is to stimulate vasoconstriction).
Activated platelets become able to attach to the site of damage (adhesion) and to each other (aggregation), forming a plug that covers the damage. In addition, they participate in plasma coagulation in two main ways - exposure of the procoagulant membrane and secretion of α-granules.
Sequence of primary biochemical and morphological changes upon activation [ edit | edit code ]
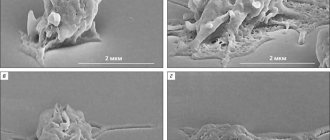
The initial stages of platelet activation under the influence of external factors are associated not only with the appearance of biochemical markers, but also with morphological changes in the form of the platelet. As has been shown by flow cytometry and electron microscopy, the most sensitive sign of activation (when platelets are exposed to ADP) are morphological changes [6]. The appearance of biochemical and morphological changes, arranged according to the degree of decrease in sensitivity, is as follows: change in platelet shape, conformational changes in glycoprotein IIb/IIIa, expression of P-selectin, expression of phosphatidylserine.
Exposure of the procoagulant membrane [edit | edit code ]
Under normal conditions, the platelet membrane does not support clotting reactions. Negatively charged phospholipids, primarily phosphatidylserine, are concentrated in the inner layer of the membrane, while phosphatidylcholine in the outer layer binds coagulation factors much less well. Although some coagulation factors can bind to non-activated platelets, this does not lead to the formation of active enzymatic complexes. Activation of the platelet presumably leads to the activation of the scramblase enzyme, which begins to quickly, specifically, bidirectionally and ATP-independently transfer negatively charged phospholipids from one layer to another. As a result, thermodynamic equilibrium is established, in which the concentration of phosphatidylserine in both layers is equalized. In addition, upon activation, many transmembrane proteins in the outer layer of the membrane undergo alignment and/or conformational changes, and they acquire the ability to specifically bind coagulation factors, accelerating reactions involving them.
Similar article - IVF for infertility of unknown origin
Platelet activation has several degrees, and procoagulant surface expression is one of the highest. Only thrombin or collagen can produce such a strong response. A weaker activator, especially ADP, can contribute to the work of stronger activators. However, they are not able to independently cause the appearance of phosphatidylserine; their effects are limited to changes in platelet shape, aggregation and partial secretion.
Secretion of α-granules [edit | edit code ]
Platelets contain several types of granules, the contents of which are secreted during activation. Essential for coagulation are α-granules containing high molecular weight proteins such as factor V and fibrinogen.
Platelet functions
Laminae not only play a key role in hemostasis and vascular disease, they also contribute to inflammation, tumor angiogenesis, and embryonic development. Platelets contain many biologically active molecules, such as plaque aggregation factors, growth factors and many other compounds that are released when blood cells are activated.
Blood plates help stop bleeding in three ways:
- Sticking to surrounding tissue.
- Clustered with other plates.
- By releasing chemical compounds that stimulate the aggregation of other cells.
There are many rare diseases associated with poor platelet function, where the platelet count is normal but the cells do not work normally. Some medications, such as aspirin, can suppress lamellar function.
It is important to know which medications affect your blood cells and understand that taking these medications may increase your risk of bleeding.
Note! The most common drugs that affect cell dysfunction are medications prescribed for the prevention of coronary heart disease, stroke and peripheral arterial diseases, as well as non-steroidal drugs.
Habitat
Platelets come from bone marrow cells called megakaryocytes. Megakaryocytes are cells that break down into fragments to form blood platelets. These cell fragments do not have a nucleus but contain structures called granules. The granules contain proteins necessary for blood clotting and breaking the seal of blood vessels. One megakaryocyte can produce from 1000 to 3000 plates.
The plates live in the blood for approximately 10 days. When cells become old or damaged, they are removed from the circulation by the spleen. The organ filters blood from old cells and also preserves functional red and white blood cells. These cells help blood clot, compensate for blood loss, and fight infectious agents such as bacteria and viruses.
Life expectancy of red blood cells - how long is it?
Platelets (blood platelets) are formed from giant cells of the red bone marrow - megakaryocytes. Platelets in the bloodstream are round or slightly oval in shape, with a diameter of 2-5 microns. Platelets do not have a nucleus, but have a large number of granules (up to 200) of various structures.
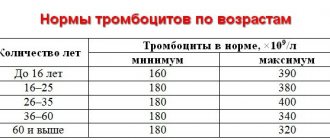
Normally 2-4 × 1011/l (Smirnov –180 × 109-320 × 109), or 200-400 thousand in 1 µl. An increase in the number is “thrombocytosis”, a decrease is “thrombocytopenia”. Under natural conditions, the number of platelets is subject to significant fluctuations.
Life expectancy is 5-8 days.
Thrombocytopoiesis is the process of platelet formation in the bone marrow. This process consists of the following stages: SC-PSC (CFU - MGCE) - unipotent precursors (CFU - MGC) → megakaryoblast → promegakaryocyte → megakaryocyte → platelets.
Factors stimulating thrombocytopoiesis:
- Short-acting thrombocytopoietins - enhance the detachment of blood platelets from megakaryocytes and accelerate their entry into the blood.
- Long-acting plateletpoietins – promote the precursors of bone marrow giant cells into mature megakaryocytes.
- IL-6 and IL-11 have a direct effect on the activity of thrombocytopoietins.
Platelets have the following properties: [2]
- phagocytosis;
- amoeboid motility;
- easy destructibility;
- adhesion;
- aggregation;
- viscous metamorphosis.
Platelets perform a number of functions:
- The homeostatic function is aimed at the formation of a blood clot in the microcirculation vessels.
- The angiotrophic function is manifested in the fact that platelets influence the structure and function of microvasculature vessels, nourishing the endothelial cells of the capillaries.
- Regulation of vascular wall tone is carried out due to serotonin, located in platelet granules, and thromboxane A2, produced in platelets from arachidonic acid during the process of platelet aggregation.
- Participation in the blood coagulation process is carried out due to platelet-derived blood coagulation factors.
Leukocytes are nucleated cells, the structural organization of which is identical to other cells of the body. Dimensions - 4-20 microns. Life expectancy is also very variable and is:
- for granulocytes and monocytes from 4-5 to 20 days
- for lymphocytes 100-120 days
The number of leukocytes in peripheral blood is (4-9) × 109/l. An increase in the number of leukocytes in the blood is “leukocytosis”, a decrease is “leukopenia”.
Neutrophils live in circulation from 8 to 10 hours, in tissues for 2-6 days. Quantity 2.0-5.5×109/l of blood (48-78% of the total number of leukocytes)
Basophils 40-60 in 1 µl, (0-0.06)×109/lily 0-1% of the total number of leukocytes. They live in blood for 1-2 days.
Eosinophils stay in the bloodstream for no more than 12 hours, after which they penetrate into tissues, where they live for 10-12 days. [3] Number (0.02 - 0.3) × 109/l, or 0.5 -5% of the total number of leukocytes .[6]
Lymphocytes up to 100 days or more. 18-40%.
PC monocytes – 12-104 hours, tissue – months, years.
It is important for patients with pathologies of the hematopoietic system to know what the lifespan of red blood cells is, how aging and destruction of red cells occurs, and what factors reduce their lifespan.
The article discusses these and other aspects of the functioning of red blood cells.
Physiology of blood
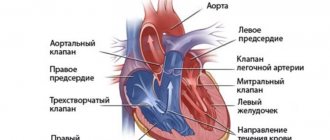
The single circulatory system in the human body is formed by blood and organs involved in the production and destruction of blood cells.
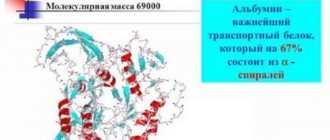
The main purpose of blood is transportation, maintaining the water balance of tissues (adjusting the ratio of salt and protein, ensuring the permeability of the walls of blood vessels), protection (supporting human immunity).
The ability to clot is the most important property of blood, necessary to prevent heavy blood loss in the event of damage to body tissues.
Important
The total blood volume in an adult depends on body weight and is approximately 1/13 (8%), that is, up to 6 liters.
In a child’s body, the blood volume is relatively larger: in children under one year old – up to 15%, after one year – up to 11% of body weight.
The total volume of blood is maintained at a constant level, while not all of the available blood moves through the blood vessels, some part is stored in blood depots - the liver, spleen, lungs, and skin vessels.
Blood consists of two main parts - liquid (plasma) and formed elements (erythrocytes, leukocytes, platelets). Plasma occupies 52–58% of the total, blood cells account for up to 48%.
The formed elements of blood include erythrocytes, leukocytes and platelets. The fractions play their role, and in a healthy body the number of cells in each fraction does not exceed certain acceptable limits.
Platelets, together with plasma proteins, help clot blood and stop bleeding, preventing excessive blood loss.
Leukocytes - white blood cells - are part of the human immune system. Leukocytes protect the human body from the effects of foreign bodies, recognize and destroy viruses and toxins.
Due to their shape and size, white bodies leave the bloodstream and penetrate the tissues, where they perform their main function.
Advice
Erythrocytes are red blood cells that transport gases (mostly oxygen) due to the protein hemoglobin they contain.
To keep the blood in a liquid state, 2 systems are counteracted, namely coagulation and anticoagulation. With the help of these mechanisms, coagulation homeostasis occurs. Platelets play a huge role in blood clotting, life expectancy, their role - such questions often worry people.
To understand why there is such a concentration of nuclear-free bodies in the blood, you need to know not only the life expectancy of platelets, but also the speed and quantity of them that appear. For every kilogram of human weight there are about 15x106. About 3,000 platelets are released from each megakaryocyte during division.
Every day the human body produces about 66 ± 14.6 thousand platelets per microliter of blood. In the blood of an adult there should be from 180 to 320x10
of these blood cells, in children they can be from 150 to 450x10
We suggest you read: Bruises on the legs due to varicose veins, how to treat bruises
. But when calculating their number, it is necessary to take into account age. For example, in newborns who are not yet 10 days old, they can be from 99 to 420x10
Type of platelet
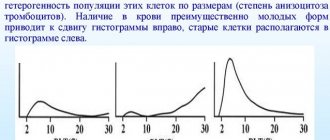
The cell fragments contain proteins on their surface that allow them to stick to breaks in the blood vessel wall. They enclose granules that can secrete other proteins needed to create a strong plug to seal broken blood vessels. Platelets also contain proteins that allow them to change shape when they become sticky. The circulating population of plates is heterogeneous in size and duration of existence.
Age variety of cells:
- Young platelets. Cells recently released from the bone marrow by megakaryocytes. They are characterized by an increased average volume and a larger number of dense granules than older plates.
- Old or damaged cells. The system detects changes that accumulate on the surface of cells as we age and responds by binding and removing them when the form reaches a critical level.
Appearance of plates
Blood plates are a flat clump of thin branches with numerous tentacles. They are usually relatively tough. In this inactive state, blood platelets pass through the entire body. If there are bloodstream injuries anywhere, they become active. The cells open their tentacles allowing for rapid closure of the wound.
When the plates are activated at the site of a ruptured blood vessel, they change shape. They become round and extend long threads or may look like an octopus, with tentacles, attracting and coming into contact with the broken blood vessel wall. With these long strands of plaque, they form a plug to seal the broken blood vessel.
Platelet structure
The plates have a diameter of 1.5 microns to 3.0 microns and are flat, disc-shaped. During blood clotting, cells change their shape thanks to activators such as ADP, collagen, thromboxane and thrombin. There is a convexity of the pseudopodia, which is associated with a multiple increase in the surface. This promotes thrombus formation through fibrin-mediated binding to other cells. This process describes platelet function and is called aggregation.
Structurally, the platelet is divided into four zones:
- Peripheral - rich in glycoproteins necessary for adhesion, activation and aggregation of plates.
- Sol-gel zone – contains microtubules that allow cells to maintain their discoid shape.
- Organella – has platelet granules. Alpha granules contain coagulation mediators such as factor V, factor VIII, fibrinogen, fibronectin, growth factor and chemotactic agents. Delta granules or dense bodies contain ADP, calcium, serotonin, which are platelet activating mediators.
- Membrane zone - includes membranes that are organized into a dense tubular system responsible for the synthesis of thromboxane A2.
Life cycle and functionality
If the blood flow is damaged, the passing plates are activated for a short time, spreading long tentacles. Thus, they find themselves drawn into each other. In addition, they activate the enzyme thrombin, which triggers the formation of the protein fibrin. Fibrin is a kind of cellular glue.
Next, the passing cells spread their tentacles, which stick to the existing lumps. In a short time, usually within 2-4 minutes, a network of tens of thousands of plaques is formed, and other blood components no longer pass through it. Fibrin binds the network of plates so that blood plasma can no longer leak out - after which regeneration begins. The wound is closed.
The average lifespan of human platelets is 8-12 days. Degradation occurs mainly in the spleen, lungs and to a lesser extent in the liver. The bone marrow must continually produce new platelets to replace those that are destroyed, used up, or lost through bleeding. Determining the number of platelets in the blood will help diagnose a number of disorders associated with too few or too many of them. A shortened platelet lifespan is also associated with an antibody response or increased blood clotting.
Number of cells
To understand why there is such a concentration of nuclear-free bodies in the blood, you need to know not only the life expectancy of platelets, but also the speed and quantity of them that appear. For every kilogram of human weight there are about 15x10 6. About 3,000 platelets are released from each megakaryocyte during division. Another 7-17% of the total is formed in the lungs. This happens because proplatelets also enter the bloodstream. They independently reach the microcircular bed of the lungs. And already in it the process of releasing platelets occurs.
Normal platelet count in human blood
Under a microscope, the cell looks like a tiny plate. Your doctor may order a blood test to see if your bone marrow is producing the right amount. In healthy people, the number of platelets ranges from 150,000 to 380,000 per microliter of blood. This indicator is considered normal.
Control values, as well as specific indicators, may vary between laboratories. Additionally, there may be daily or seasonal variations in disease-free rates. Before reacting to abnormal results, ask a specialist to interpret the tests based on your personal history. Studies are assessed in the context of other disorders and over time.
On a note! The number of cells also tends to decrease with age.
Levels below the normal limit may not be a cause for concern in older adults, especially if there are no other symptoms.
Leukocytes
In addition to red blood cells, blood contains relatively colorless cells - white blood cells (leukocytes) . They include granulocytes (polymorphonuclear leukocytes or polymorphonuclear cells), lymphocytes and monocytes. Their lifespan, unlike the lifespan of red blood cells, varies widely and ranges from several hours to several years. Together with the organs of the immune system (spleen, thymus gland, lymph nodes, tonsils, etc.), white blood cells form the immune system, which is divided into nonspecific and specific.
What does a change in platelet count indicate?
Rare conditions cause the bone marrow to produce too many plaques, sometimes as many as one or two million per microliter. Some patients have an increased risk of blood clots, but many people with these disorders do not have problems. A low cell count disorder is called thrombocytopenia. An enlarged spleen or immune thrombocytopenia results in a shortened average lifespan, resulting in an overall low platelet concentration with a constant production rate.
Conversely, after removal of the spleen, there is a dramatic increase in platelet counts due to the lack of indirect degradation. Pathological changes in the bone marrow lead to essential thrombocythemia and polycythemia vera. An increase in the number of plates is called thrombocytosis.
Other rare diseases associated with platelet deficiency:
- TAR syndrome.
- Wiskott-Aldrich disease.
- Gray platelet syndrome.
- Jacobsen's syndrome.
- Gaucher's disease.
Thrombocytopenia
Thrombocytopenia is the inability of the bone marrow to produce the normal number of platelets. The disorder is also associated with increased breakdown of plaques once they form and are released into the circulation. If the platelet count becomes too low, bleeding may appear under the skin as a bruise, inside the body as internal bleeding, or externally. Thrombocytopenia is caused by many conditions, including several medications, cancer, kidney disease, pregnancy, infections, and a compromised immune system.
Signs and symptoms of thrombocytopenia:
- easy or excessive bruising (purpura);
- superficial bleeding on the skin, which appears as a rash with reddish-purple spots (petechiae) of precise size, usually on the lower leg;
- prolonged blood loss from cuts;
- bleeding from the gums or nose;
- blood in urine or stool;
- unusually heavy menstrual flow;
- fatigue;
- enlarged spleen;
- jaundice.
Note! Various medications can affect the number of platelets in the blood. During pregnancy, platelet levels often decrease. About 5-10% of pregnant women have less than 150,000 platelets/mm.
Probable diseases
- Leading to a decrease in the number of platelets in the blood
- Leading to an increase in the number of platelets in the blood or to disruption of their functionality
- Impaired platelet adhesion and aggregation ability
- Bernard-Soulier syndrome
- Glanzmann's thrombasthenia
- Scott syndrome
- von Willebrand disease
- Hermansky-Pudlak syndrome
- Gray platelet syndrome
- Disorders of platelet metabolism
- Reduced cyclooxygenase activity, congenital or acquired
- Platelet pool deficiency, congenital or acquired
- Diseases in which platelets play a key role
When platelet levels decrease, there is a high risk of developing aplastic anemia, Werlhoff and Gaucher disease, and cytopenic purpura. With an increase in the number of red plates in the blood, the likelihood of dengue fever and hemolytic syndrome arises. But first of all, you should be checked for cancer. Impaired platelet function of aggregation and adhesion leads to Bernard-Soulier, von Willebrand, Pudlak, and Scott syndromes. When red cell metabolism fails, atherosclerosis, cardiac ischemia, cerebrovascular and arterial diseases, malaria, asthma, and cancer are observed.