A general blood test is perhaps the most common laboratory diagnostic method. In modern civilized society, there is practically not a single person who does not have to repeatedly donate blood for a general analysis.
After all, this study is carried out not only on sick people, but also on completely healthy people during routine medical examinations at work, in educational institutions, and in the army.
This blood test includes determination of hemoglobin concentration, number of leukocytes and leukocyte formula count, determination of the number of red blood cells, platelets, erythrocyte sedimentation rate (ESR) and other indicators.
Thanks to the correct interpretation of the results of a general blood test, it is possible to establish the cause of certain symptoms in adults, determine the type of disease of the blood and internal organs, and select the correct treatment regimen.
What it is?
A general (detailed) blood test includes:
- Hemoglobin and hematocrit levels.
- Erythrocyte sedimentation rate (ESR), formerly called reaction rate (ERR).
- Color index calculated according to the formula, if the study was carried out manually, without the participation of laboratory equipment;
- Determination of the content of cellular elements of blood: erythrocytes - red blood cells containing the pigment hemoglobin, which determines the color of blood, and leukocytes, which do not contain this pigment, therefore are called white blood cells (neutrophils, eosinophils, basophils, lymphocytes, monocytes).
As you can see, a general blood test shows the reaction of this valuable biological fluid to any processes occurring in the body. As for the correct testing, there are no complex, strict regulations regarding this testing, but there are certain restrictions:
- The analysis is carried out in the morning. The patient is prohibited from consuming food or water 4 hours before taking a blood sample.
- The main medical supplies used for drawing blood are a scarifier, cotton wool, and alcohol.
- For this examination, capillary blood is used, which is taken from a finger. Less often, according to the doctor's instructions, blood from a vein can be used.
After receiving the results, a detailed breakdown of the blood test is performed. There are also special hematology analyzers that can automatically determine up to 24 blood parameters. These devices are capable of producing a printout with a transcript of the blood test almost immediately after blood collection.
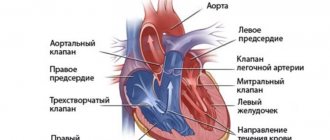
Structure and functions
A lot of necessary information useful for a person can be learned from the test results. Judging by them, it is possible to identify all the processes occurring in the body. To correctly interpret the results, you need to know all the main indicators. All blood cells have a common origin, but they play different roles and have their own functions.
The functions of red blood cells, leukocytes and platelets and the quality of their work greatly influence the condition of the blood in the body. They are similar in some ways and different in others.
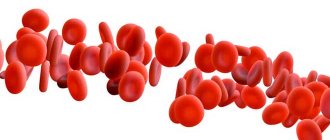
Red blood cells
One of the components of blood is the red blood cell; its structure and functions are important for the body. The particles do not have a nucleus or cytoplasmic organelles. The appearance resembles a double-sided disk convex inward. Its dimensions: diameter - 7-8 microns, thickness 1-2.5 microns. Their plasticity allows them to pass through holes smaller than themselves. The older the red blood cell, the less plasticity it has. Due to the structure of the membrane, half of which is protein, it is a good conductor of oxygen, carbon dioxide, etc. Hemoglobin is the most important component that contains iron.
This cell element has the following functions:
- Transport - the transfer of gases (oxygen is released, carbon dioxide is released) and other substances.
- Role in blood coagulation and regulation of viscosity.
- The cell breathes due to hemoglobin, which attracts O2 and CO2.
- Protective (creating immunity) - maintain balance in vascular formation.
Important information: What does ESR mean above normal or elevated in a child’s blood test?
Red blood cells carry out their activity for 100-120 days. In the liver or spleen they are broken down and converted into a component of bile.
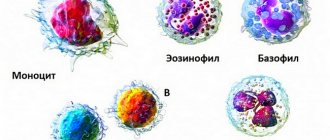
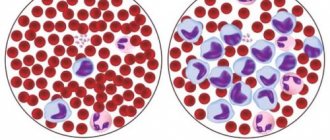
Leukocytes
Leukocytes are found in blood plasma and lymph. They are white bodies with colorless cytoplasm. The shape of their nuclei is not constant, this distinguishes leukocytes from other elements. This feature determines the duration of their existence from 2 to 4 days. They are formed in the spleen, lymph nodes and bone marrow.
Leukocytes vary in appearance, structure and functions, because... They begin their growth either along one or the other branch of hematopoiesis.
The myeloid lineage includes:
- Neutrophils are contained in cells, enter the tissue only when necessary for phagocytosis (destruction), and then die.
- Basophils - serve to produce substances in immune reactions. Their stay in the blood is short, then they turn into mast cells, and these are tissues.
- Eosinophils - act against parasites, participate in allergic reactions. Tissue life is small.
- Monocytes - unlike neutrophils, large viruses or a cell with bacteria are attracted to the process of phagocytosis. They do not linger in the blood; they become tissue macrophages in tissues and support local immunity.
The lymphoid germ includes lymphocytes, the production of antibodies is their main goal. There are 2 types: T- and B-lymphocytes. Their ratio is called the leukocyte formula, which indicates favorable or unfavorable changes in the human immune system.
Their composition is variable. This makes it possible to implement its main function. First of all, these are cells of the immune system. The main function is to prevent the introduction of pathogenic substances into the body.
Important information: Norm of lymphocytes in the blood of men (table by age)
Functions of leukocytes:
- Leukocytes recognize signals from other cells about danger.
- Activation and appropriate response to signals. Antibody production.
- Phagocytosis is the process of absorption and digestion of foreign microorganisms.
- Destruction and removal of protein-based toxins.
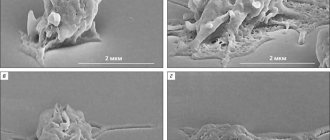
Platelets
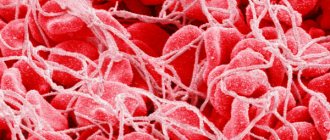
They are small plates formed from megakaryocytes (large bone marrow cells). They accumulate proteins necessary for the production of blood clots. Parts of their cytoplasm separate and enter the bloodstream. They do not have a nucleus, but have a large number of granules. If there is damage along the way, the platelet attaches to it with its processes, so it stops the bleeding.
Functions of platelets:
- Platelets form a platelet plug and secrete substances to constrict blood vessels.
- They build up the metabolic process in the vessels.
- Adhesion (sticking) of some antigens and pathogens.
- They provide their surface to accelerate coagulation.
Platelets are an integral part of the complex clotting process. There must be a constant dynamic equilibrium with an anticoagulant function, due to which the blood is maintained in a liquid state, but if the vessel is damaged, a blood clot forms.
Complete blood count: normal indicators in the table
The table shows the normal number of blood elements. These values may differ in different laboratories, so to find out whether the blood test results accurately correspond to the norm, it is necessary to find out the reference values of the laboratory in which the blood test was carried out.
Table of normal indicators of a general blood test in adults:
| Analysis: | Adult women: | Adult men: |
| Hemoglobin | 120-140 g/l | 130-160 g/l |
| Hematocrit | 34,3-46,6% | 34,3-46,6% |
| Platelets | 180-360×109 | 180-360×109 |
| Red blood cells | 3,7-4,7×1012 | 4-5,1×1012 |
| Leukocytes | 4-9×109 | 4-9×109 |
| ESR | 2-15 mm/h | 1-10 mm/h |
| Color index | 0,85-1,15 | 0,85-1,15 |
| Reticulocytes | 0,2-1,2% | 0,2-1,2% |
| Thrombocrit | 0,1-0,5% | 0,1-0,5% |
| Eosinophils | 0-5% | 0-5% |
| Basophils | 0-1% | 0-1% |
| Lymphocytes | 18-40% | 18-40% |
| Monocytes | 2-9% | 2-9% |
| Average red blood cell volume | 78-94 fl | 78-94 fl |
| Average hemoglobin content in erythrocytes | 26-32 pg | 26-32 pg |
| Band granulocytes (neutrophils) | 1-6% | 1-6% |
| Segmented granulocytes (neutrophils) | 47-72% | 47-72% |
Each of the given indicators is important when deciphering a blood test, however, a reliable result of the study consists not only of comparing the data obtained with the norms - all quantitative characteristics are considered together, in addition, the relationship between various indicators of blood properties is taken into account.
Platelet norms by gender and age
| Gender, age | Norm, cells/l |
| In adult men | 3.9•10 12 –5,5•10 12 |
| In adult women | 3,9•10 12 –4,7•10 12 |
| In fetal cord blood | 3,9•10 12 –5,5•10 12 |
| 1-3 days from birth | 4.0•10 12 –6.6•10 12 reticulocytes - 3–51% |
| 7 days | 3,9•10 12 –6,3•10 12 |
| 14 days | 3,6•10 12 –6,2•10 12 |
| 30 days | 3,0•10 12 –5,4•10 12 |
| 60 days | 2,7•10 12 –4,9•10 12 |
| 6 months | 3,1•10 12 –4,5•10 12 reticulocytes - 3–15% |
| up to 12 years | 3,5•10 12 –5,0•10 12 reticulocytes - 3–12% |
| Teenage girls 13–19 years old | 3,5•10 12 –5,0•10 12 reticulocytes 2-11% |
| Teenage boys 13–16 years old | 4,1•10 12 –5,5•10 12 reticulocytes 2-11% |
| 16 - 19 years old | 3,9•10 12 –5,6•10 12 |
| Aged people | 4,0•10 12 |
| Pregnant | 3,5•10 12 –5,6∙10 12 reticulocytes - approximately 1% |
Now there is a firm belief that the iron released during the death of red blood cells is completely used for the construction of new molecules, having previously been deposited in the liver and spleen in reserve. From the reserve, it takes part in hemoglobin formation in the bone marrow.
In addition to the use of reserve iron, a mechanism has been discovered for the direct utilization of hemoglobin iron by hematopoietic cells.
| Gender, age | Norm, units per liter (U/l) |
| Babies up to 3 days old | 7 – 32 × 109 |
| Up to 1 year | 6 – 17,5 × 109 |
| 1-2 years | 6 – 17 × 109 |
| 2-6 years | 5 – 15,5 × 109 |
| 6-16 years | 4,5 – 13,5 × 109 |
| 16-21 years old | 4,5 – 11 × 109 |
| Adult men | 4,2 – 9 × 109 |
| Adult women | 3,98 – 10,4 × 109 |
| Elderly men | 3,9 – 8,5 × 109 |
| Older women | 3,7 – 9 × 109 |
Red blood cells
Formed elements of blood. They contain hemoglobin, which is found in each of the red blood cells in equal quantities. Red blood cells transport oxygen and carbon dioxide in the body.
Promotion:
- Vaquez disease (erythremia) is a chronic leukemia.
- As a result of hypohydration with sweating, vomiting, burns.
- As a consequence of hypoxia in the body in chronic diseases of the lungs, heart, narrowing of the renal arteries and polycystic kidney disease. An increase in erythropoietin synthesis in response to hypoxia leads to an increase in the formation of red blood cells in the bone marrow.
Decrease:
- Anemia.
- Leukemia, myeloma - blood tumors.
The level of red blood cells in the blood also becomes lower in diseases that are characterized by increased breakdown of red blood cells:
- hemolytic anemia;
- iron deficiency in the body;
- lack of vitamin B12;
- bleeding.
The average lifespan of an erythrocyte is 120 days. These cells are formed in the bone marrow and destroyed in the liver.
Platelet cytology
Platelets are cells without nuclei. They consist of two zones: one light zone - the hyalomere and a centrally located granular zone - the granulomere. Their cytoplasm contains dense granules containing ADP, ATP, GDP, GTP, inorganic phosphates, serotonin and calcium ions. Platelets have many mitochondria and enzyme systems. In the central zone there are alpha granules, which contain fibrinogen, albumin, kallikrein, endothelial growth factor, platelet growth factor and others. The cytoplasm of platelets also contains glycogen vesicles, lysosomes, contractile microfilaments, microtubules, remnants of the endoplasmic reticulum, and the Golgi apparatus. Lysosomes contain acid hydrolases such as beta-galactosidase, beta-arabinosidase and arylsulfatase. Platelets produce certain cytokines as platelet-derived growth factor, which stimulates the regeneration of endothelial and smooth muscle cells.
Platelets
Formed elements of blood involved in ensuring hemostasis. Platelets are formed in the bone marrow from megakaryocytes.
An increase in the number of platelets (thrombocytosis) is observed when:
- bleeding;
- splenectomy;
- reactive thrombocytosis;
- treatment with corticosteroids;
- physical stress;
- iron deficiency;
- malignant neoplasms;
- acute hemolysis;
- myeloproliferative disorders (erythremia, myelofibrosis);
- chronic inflammatory diseases (rheumatoid arthritis, tuberculosis, cirrhosis of the liver).
A decrease in platelet count (thrombocytopenia) is observed with:
- decreased platelet production;
- DIC syndrome;
- increased destruction of platelets;
- hemolytic-uremic syndrome;
- splenomegaly;
- autoimmune diseases.
The main function of this blood component is to participate in blood clotting. Platelets contain the bulk of clotting factors, which are released into the blood when necessary (damage to the vessel wall). Thanks to this property, the damaged vessel is clogged by the forming thrombus and bleeding stops.
Platelet functions
Platelets play an important role in hemostasis processes. In addition, they are involved in the regeneration of endothelial cells, smooth muscle cells and fibroblasts due to the factors they produce.
When the integrity of the vessel wall is compromised, many platelets accumulate at the site of damage. This phenomenon is called adhesion. Adhesion is a receptor-dependent process that occurs with the participation of collagen and glycoprotein receptors and von Willebrand factor receptor. Then aggregation occurs to form a platelet plug. Aggregation is also a receptor-dependent process. During aggregation, platelets change their shape, becoming rounded, increasing in volume and forming a pseudopod. These changes are called viscous metamorphosis. These processes are accompanied by the spillage of contents into platelet organelles, which includes the release of vasoconstrictors (thromboxane A2, serotonin), blood clotting factors and platelets.
Leukocytes
White blood cells. Formed in red bone marrow. The function of leukocytes is to protect the body from foreign substances and microbes. In other words, it is immunity.
Increase in leukocytes:
- infections, inflammation;
- allergy;
- leukemia;
- condition after acute bleeding, hemolysis.
Decrease in leukocytes:
- bone marrow pathology;
- infections (flu, rubella, measles, etc.);
- genetic abnormalities of immunity;
- increased spleen function.
There are different types of leukocytes, so a change in the number of individual types, and not all leukocytes in general, is of diagnostic importance.
Functions of leukocytes
The life of leukocytes in a person’s blood implies the performance of certain functions:
- informational;
- protection from the action of harmful cells that pose a danger;
- antibody production;
- hemostatic functionality;
- transport;
- synthetic;
- emigration of leukocytes.
Depending on how many leukocytes are in the blood, you can get information about the physical condition of a person and the possible development of pathology. The protective function involves a process called phagocytosis - when a pest enters the bloodstream, leukocytes attack the enemy and kill him.
The function of blood clotting is provided - hemostatic functionality. A function such as the production of antibodies characterizes the formation of active protein compounds to combat pathogens. Also, with the help of leukocytes, amino acids and active components are transported through blood vessels to organs.
Emigration of leukocytes occurs during the development of disease in the body. During this process, protected cells move through the walls of blood vessels and rush to the source of infection, destroying diseased tissue.
Basophils
When released into the tissues, they turn into mast cells, which are responsible for the release of histamine - a hypersensitivity reaction to food, medications, etc.
- Increased: hypersensitivity reactions, chicken pox, hypothyroidism, chronic sinusitis.
- Decreased: hyperthyroidism, pregnancy, ovulation, stress, acute infections.
Basophils take part in the formation of delayed-type immunological inflammatory reactions. They contain large amounts of substances that cause tissue inflammation.
Granular leukocytes
The group of granular leukocytes includes: neutrophils, eosinophils and basophils. Neutrophil granulocytes are the first to participate in the inflammatory process. These are the most numerous leukocytes. Their lifespan is about 5 days. They have the properties of chemotaxis, adhesion, diapedesis and phagocytosis. Eosinophilic granulocytes provide protection against parasitic infections. Their number increases in allergic conditions and parasitosis. Basophil granulocytes are involved in the allergic and antigen response and secrete heparin, histamine and leukotrienes.
Neutrophils
They are divided into several groups - young, rod and segmented. Neutrophils provide antibacterial immunity, and their varieties are the same cells of different ages. Thanks to this, it is possible to determine the severity and severity of the inflammatory process or damage to the hematopoietic system.
An increase in the number of neutrophils is observed during infections, mainly bacterial, injuries, myocardial infarction, and malignant tumors. In severe diseases, mainly band neutrophils increase - the so-called. rod shift to the left. In particularly severe conditions, purulent processes and sepsis, young forms can be detected in the blood - promyelocytes and myelocytes, which should not normally be present. Also, during severe processes, toxic granularity is detected in neutrophils.
Thrombocytopoiesis
Platelets are derived from proplatelets, which in turn are derived from megakaryocytes. As platelets pass through the pulmonary capillaries, they break down into platelets. The earliest platelet precursor is an acetylcholinesterase-positive cell, which is the progenitor of megakaryocytes. Megakaryocytes are large polyploid cells from which proplatelets and hence platelets are derived. Interleukin-3, interleukin-6 and interleukin-11 are required for normal thrombocytopoiesis. The main regulator of this process is thrombopoietin, produced by hepatocytes (liver cells). The life cycle of platelets in the blood lasts from 5 to 11 days. They then lose their functional abilities and undergo phagocytosis through macrophages in the spleen, lungs and liver.
Color index
Reflects the relative content of hemoglobin in red blood cells. Used for the differential diagnosis of anemia: normochromic (normal amount of hemoglobin in the red blood cell), hyperchromic (increased), hypochromic (decreased).
- A decrease in CP occurs with: iron deficiency anemia; anemia caused by lead intoxication, in diseases with impaired hemoglobin synthesis.
- An increase in CP occurs with: insufficiency of vitamin B12 in the body; folic acid deficiency; cancer; polyposis of the stomach.
Color index (CI): 0.85-1.1.
Increase in platelets
When platelets are elevated in a person's blood, doctors talk about thrombocytosis. This condition can be pathological and physiological. Reasons for an increase in cell concentration that are not associated with diseases are:
- Period.
- Pregnancy.
- Intense physical activity.
- Taking medications.
Among the pathologies that can cause thrombocytosis are:
- Malignant neoplasms of internal organs and blood.
- Infectious diseases occurring in acute form.
- Development of inflammatory processes in the body.
- Autoimmune disorders.
- Malfunction of the liver and gall bladder.
- Surgery to remove the spleen.
- Bone marrow lesions.
- Bleeding.
- Obesity.
- Stress.
Drinking alcohol on the eve of donating blood for analysis can cause platelet abnormalities. There may simply be an incorrect result due to incorrect testing technique in the laboratory.
Elevated levels occur due to many reasons. Some do not depend on a person’s will, while others can be eliminated by each patient independently, for example: stop drinking alcohol.
Hemoglobin
An increase in hemoglobin concentration occurs with erythremia (decreased number of red blood cells), erythrocytosis (increased number of red blood cells), as well as with blood thickening - a consequence of large loss of fluid by the body. In addition, the hemoglobin level is increased with cardiovascular decompensation.
If the hemoglobin value is more or less than the normal limit, this indicates the presence of pathological conditions. Thus, a decrease in the concentration of hemoglobin in the blood is observed with anemia of various etiologies and with blood loss. This condition is also called anemia.
Monocytes
Monocytopenia – stress.
Monocytosis - in malignant diseases.
The term "smearing" refers to the appearance of young, immature forms of white blood cells in the peripheral blood and is usually a sign of the manifestation of pathological processes in leukopoiesis.
The leukocyte formula in children differs significantly from that in adults. Persistent lymphocytosis (increased number of lymphocytes) is typical for newborns. The number of lymphocytes gradually increases after birth, and the number of neutrophil granulocytes decreases. This condition is called physiological lymphocytosis. By the third year of life, the number of lymphocytes begins to decrease significantly, and the number of neutrophils begins to increase. At the age of 14-15 years, the number of leukocytes begins to approach the norm for an adult.
Hematocrit
Hematocrit is the percentage ratio of the volume of the blood being tested to the volume occupied by red blood cells in it. This indicator is calculated as a percentage.
A decrease in hematocrit occurs when:
- anemia;
- fasting;
- pregnancy;
- water retention in the body (chronic renal failure);
- excess protein content in plasma (myeloma);
- drinking plenty of fluids or administering large amounts of intravenous solutions.
An increase in hematocrit above normal indicates:
- leukemia;
- polycythemia vera;
- burn disease;
- diabetes mellitus;
- kidney diseases (hydronephrosis, polycystic disease, neoplasms);
- fluid loss (excessive sweating, vomiting);
- peritonitis.
Normal hematocrit values: Men – 40-48%, women – 36-42%.
Causes of increased leukocytes
If lymphocytes are elevated, it means lymphocytosis is present. It develops as a result of infectious pathologies, acute allergic reaction, anaphylactic shock, the occurrence of malignant and benign neoplasms, and autoimmune disorders.
In addition to these diseases, an increase in the level of lymphocytes can be provoked by:
- Surgical intervention. When a person undergoes surgery, the number of leukocytes in the blood always increases. This condition is not dangerous to health; the indicator returns to normal after the body has fully recovered.
- Poor nutrition. This factor can lead to a weakening of the immune system. Usually, in order to restore the level of lymphocytes, it is enough to adjust the diet. If your body is severely weakened, you will need medical help.
- Taking certain medications. An increase in the number of cells due to this factor does not pose a threat to health; the indicator returns to normal as soon as the intake is stopped.
Types of leukocytes
- Monocytes. They have a longer lifespan than many white blood cells and help destroy bacteria.
- Lymphocytes. They produce antibodies to protect against bacteria, viruses and other potentially harmful invaders.
- Neutrophils. They kill and digest bacteria and fungi. They are the most numerous type of white blood cells and the first line of defense against infections.
- Basophils. These small cells release chemicals such as histamine and an allergy marker that help control the body's immune response.
- Eosinophils. They attack and kill parasites, destroy cancer cells and help with allergic reactions.
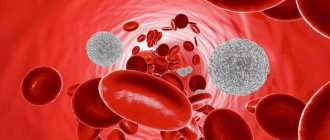
The bigger, the better?
Even with all their disease-fighting abilities, too many white blood cells can be a bad sign. For example, a person suffering from leukemia, a blood cancer, may have up to 50,000 white blood cells in one drop of blood. All its elements (erythrocytes, leukocytes and platelets) come from hematopoietic stem cells and bone marrow, as well as the umbilical cord of newborn children. On average, the body of an adult contains about 5 liters of blood, which mainly consists of plasma (55-60%) and blood cells (40-45%). The lifespan of red blood cells, white blood cells and platelets, as well as their structure and composition, differ, but they all play an important role in the functioning of the body.
The number of red and white blood cells in the blood can serve as an indicator of certain diseases. Leukopenia can be caused by factors that can impair bone marrow function. A condition characterized by a low number of red blood cells is usually called anemia, and can include iron deficiency and vitamin B12 deficiency. This disease can impair the blood's ability to carry oxygen, which may result in increased fatigue, shortness of breath, and paleness. The lifespan of white blood cells, platelets and red blood cells, their appearance, composition and functions are radically different, but they all play an important role. Thus, a reduction or significant increase in their number can lead to various health problems.
An important component of the blood system
White blood cells are an important component of the blood system, which also consists of red blood cells, platelets and plasma. Although they make up only about 1% of all blood, their impact is significant: they are essential for good health and protection against disease. We can say that these are immune cells. In a sense, they are constantly at war with viruses, bacteria and other “foreign invaders” that threaten your health.
When a specific area is attacked, white blood cells rush to destroy the harmful substance and prevent disease. White blood cells are produced within the bone marrow and stored in the blood and lymph tissues. Since the lifespan of human leukocytes is short, some types have a completely short lifespan - from one to three days. Therefore, the bone marrow is engaged in their constant reproduction.
Protection against infections
Blood is made up of several components, including red blood cells, white blood cells, platelets, and plasma. A healthy adult has between 4,500 and 11,000 white blood cells per cubic millimeter of blood. White blood cells, also called leukocytes or white corpuscles, are a cellular component of blood that protects the body from infection and disease by ingesting foreign materials and destroying infectious agents, including cancer cells, and by producing antibodies.
An abnormal increase in the number of white cells is known as leukocytosis, while an abnormal decrease in the number is called leukopenia. The number of white blood cells can increase in response to intense physical activity, convulsions, acute emotional reactions, pain, pregnancy, childbirth and some other painful conditions, such as infections and intoxications. Their numbers may decrease in response to certain types of infections or drugs, or in combination with certain conditions, such as chronic anemia, malnutrition, or anaphylaxis.
Destruction of leukocytes
The lifespan of leukocytes, platelets and erythrocytes has been sufficiently studied, which cannot be said about the processes of their destruction. It is known that all types of white cells, after a certain period of circulation in the blood, enter the tissues. There is no turning back now. In tissues they perform their phagocytic function and die. Important contributions to the study of white blood cells and their properties were made by Ilya Mechnikov and Paul Ehrlich. The first discovered and studied the phenomenon of phagocytosis, and the second brought out various types of leukocytes. In 1908, the scientists were jointly awarded the Nobel Prize for these achievements.
Source: www.syl.ru