Lymphocytes are a type of cell of the human body's immune system. These cells are formed as a result of differentiation during the development of bone marrow cells. Lymphocytes are responsible for carrying out such important functions of the immune system as recognizing various bacteria and infections, as well as ensuring a timely immune response of the body to the appearance of foreign elements in its internal environment.
There are several types of lymphocytes in the human body:
- T lymphocytes , these cells are formed in the thymus tissue. This type of lymphocyte is responsible for recognizing bacteria. T-lymphocytes are responsible for the formation of an adequate immune response of the body to the penetration of foreign bacteria into the body.
- B lymphocytes represent about 15% of the total number of lymphocytes. These cells are produced by the tissue of the tonsils, lymph nodes, and also in the spleen. This type of lymphocyte synthesizes specific proteins called antibodies. Antibodies search for viruses, bacteria and tumor cells in the human body and ensure their destruction.
- NK lymphocytes . This type of lymphocyte makes up about 10% of the total number of these elements in the peripheral blood. NK cells prevent infections from entering the body, as well as destroy tumor cells.
Types of lymphocytosis
Lymphocytosis has a code according to ICD-10 (International Classification of Diseases, 10th revision) - D72.8.
Relative lymphocytosis
Relative lymphocytosis is a phenomenon in which leukocytes are within normal limits per unit volume of blood. At the same time, the number of lymphocytes in proportion to cells of the same class is increased. This picture can occur as a variant of the norm if the test was taken by a child under two years of age. In children, during the development of the immune system, the number of lymphocytes and neutrophils changes. This phenomenon is physiological in nature and is called neutrophil-lymphocyte crossover.
Human immune cells
In adults, this indicator often indicates a depleted immune system and is a sign of a protracted purulent-inflammatory disease - furunculosis or prolonged pneumonia. At the same time, the number of neutrophils decreases relative to lymphocytes, because most of the neutrophils go into pus and do not have time to recover. Neutropenia is a sharp drop in the number of neutrophils in the blood.
If the number of lymphocytes is reduced to a critical level, this is leukopenia. It can occur with a genetic defect, metabolic disorder with a lack of folic acid, B vitamins and copper, bone marrow lesions, work with chemical reagents - pesticides, benzenes, etc.
If the number of lymphocytes is increased, this clinical picture may indicate:
- splenomegaly – enlargement of the spleen;
- hyperthyroidism - the release of thyroid hormones is greater than what the body requires;
- Addison's disease - the adrenal glands do not produce the required amount of hormones, especially cortisol.
Granulopenia is a reduced content of granulocytes in the bloodstream. A granulocyte is a white blood cell with a large segmented nucleus. Provides cellular immunity. Production is suppressed in typhoid fever and tularemia.
Relative lymphocytosis is more common than absolute lymphocytosis.
Absolute lymphocytosis
Absolute lymphocytosis is an absolute increase in the number of lymphocytes in the blood. The type of action is reactive lymphocytosis. Occurs as a reaction to another acute disease:
- acute infections - chicken pox, measles, hepatitis of various origins, whooping cough;
- tuberculosis;
- oncological diseases – lymphosarcoma, lymphocytic leukemia;
- autoimmune disease - AIDS.
After eliminating the cause of the disease, it goes away within 1-2 months.
Infectious lymphocytosis
Infectious lymphocytosis appears during the formation of acute damage to the body
T-lymphotropic virus. T-lymphotropic viruses are viruses from the genus deltaretroviruses that cause malignant formations of hematopoietic tissue - T-cell leukemia and lymphoid tissues - T-cell lymphoma in humans. Affects adults. Rarely seen.
Oncological (malignant) lymphocytosis
Malignant lymphocytosis manifests itself as an independent disease of the lymphoproliferative profile - chronic or acute leukemia.
Causes of lymphocytosis in adults
Conventionally, a distinction is made between reactive and malignant lymphocytosis. The first is due to the protection of the immune system from the disease and goes away a month or two after recovery, the second is associated with cancer that is not associated with external factors.
In order to determine the root cause of the deviation, one blood donation is not enough. Perhaps the doctor will prescribe additional examination, including a bone marrow examination, a more detailed analysis of the status of lymphocytes, etc.
The causes of lymphocytosis in the blood may be as follows:
- Viral (measles, whooping cough, chickenpox, HIV, hepatitis, ARVI, rubella, etc.);
- Bacterial diseases (tuberculosis, brucellosis, syphilis, etc.);
- Injuries;
- Burns (including sunburn);
- Hypersensitivity to drugs;
- Blood transfusions;
- Postoperative condition after removal of the spleen;
- Autoimmune diseases (lupus erythematosus, rheumatoid arthritis);
- Emotional stress, nervous breakdowns;
- Constant and frequent smoking;
- Vitamin B12 deficiency in the body;
- Condition with risk of tumor development (malignant thymoma);
- Oncological diseases (chronic lymphocytosis, lymphoblastic leukemia, malignant lymphoma).
The causes of lymphocytosis in children are usually due to imperfections of the immune system in childhood. However, the reasons listed above should not be excluded, especially if lymphocytosis in a child is observed over a long (more than six months) period of time.
Lymphocytosis is often observed in preschool children, but generally this does not indicate a serious illness.
Lymphocytosis in children under one year of age can also appear due to incompletely formed immunity. It is important to pay attention to the child's behavior and not engage in self-analysis if you do not have a medical education. Do not hesitate to clarify the primary diagnosis with your doctor; perhaps he will prescribe medications to support immunity or intestinal microflora.
Causes of lymphocytosis
Lymphocytes are predominantly localized in the bone marrow. But in addition to the bone marrow, the lymphocyte depot is also located in the spleen, small intestine, tonsils of the throat, and in groups of lymph nodes. When a foreign pathogen enters the body, an immune response follows - the number of white blood cells increases.
Leukocyte in human blood
Infections of viral and bacteriological origin are the most common causes of lymphocytosis. These also include:
- Viral infections - infectious mononucleosis (Filatov's disease), hepatitis A, acute viral hepatitis, measles, ARVI, HIV, cytomegalovirus infection.
- Bacterial infections - tuberculosis, staphylococci, syphilis, salmonella, typhoid fever, whooping cough. Also brucellosis - Maltese fever.
- Diseases caused by parasites – toxoplasmosis.
- Diseases of the endocrine system - hyperthyroidism, Addison's disease.
- Rheumatic diseases - gout, rheumatoid arthritis.
- Diseases of the lymphatic system - lymphoma, Waldenström's macroglobulinemia, chronic lymphocytic leukemia.
- Diseases of oncological origin, malignant and benign, including damage to the hematopoietic organs.
Among the causes of an increase in lymphocytes in the blood are not only diseases. Lymphocytosis also causes:
- Long-term smoking of tobacco. Smokers have increased lymphocyte levels.
- Stress, which provokes hormonal surges. This includes menstrual periods for women and heavy physical activity. If, during a stressful situation, a subconscious “fight or flight” reaction occurs, then the level of “natural killer” cells in the blood increases. If such stress lasts a long time and becomes chronic, the opposite effect appears - leukopenia. Lymphocytosis is temporary and goes away on its own.
- Poisoning of the body with heavy metals or chemicals - lead, carbon disulfide, arsenic.
- Splenectomy.
- Treatment with certain drugs - chloramphenicol, phenytoin, levodopa, glucocorticoid drugs. Or an overdose of analgesics.
- Exhaustion of the body can be characterized by loss of strength, lethargy, and low temperature.
Treatment of lymphocytosis
Treatment of lymphocytosis is aimed primarily at eliminating the cause that caused a corresponding increase in lymphocytes in the bloodstream. Therapy must be carried out, since this condition can subsequently lead to various unpleasant complications, including large blood loss and decreased blood clotting.
As practice shows, relative lymphocytosis caused by acute respiratory viral infections goes away on its own after two weeks. If it is possible to accurately establish the cause of the change in the composition of the blood flow, then this condition does not require treatment.
Infectious lymphocytosis is treated mainly with the use of medications - sulfonamides and ACTH. In a child, such changes in the composition of the bloodstream are usually treated with the use of aureomycin. It also assumes:
- Maintaining bed rest;
- Taking vitamins;
- Symptomatic drugs;
- Desensitizing agents.
If a secondary infection occurs, the patient may be prescribed antibacterial therapy.
Symptoms of lymphocytosis
It is not an independent disease, except for the infectious form. In most cases, this is an additional symptom to the disease. Therefore, signs of lymphocytosis are the symptoms of the underlying disease, which caused a shift in the leukocyte formula.
Only a qualified specialist can prescribe treatment after a complete examination and diagnosis.
Symptoms of probable lymphocytosis include:
- Enlarged liver – hepatomegaly, spleen – splenomegaly.
- Enlarged lymph nodes – lymphadenopathy.
- Increased activity of the sweat glands.
- Weakness and fatigue.
- A sharp change in body temperature, which is accompanied by exhaustion and chills.
- Disturbances in the digestive system - vomiting, nausea, diarrhea, constipation, alternation of stools.
- Hyperthermia of the pharynx mucosa, cough, runny nose, and other symptoms of respiratory tract disease.
- Nervous disorder, lack of appetite, sleep disturbances.
- Almost white skin.
- Enlargement of the tonsils of the throat against the background of high body temperature up to 40 degrees.
- The level of lymphocytes in the bone marrow is increased.
In children, the general symptoms include bloating, unstable stools, paroxysmal vomiting, skin rashes (rarely), lethargy and tearfulness.
Main symptoms
Lymphocytosis is not considered an independent pathology. This is a consequence of a certain disorder or change in the body. Therefore, with lymphocytosis, symptoms of the primary disease may be observed. With viral pathogenesis, body temperature rises and a sore throat appears.
Cancer is accompanied by bone pain, fever, bleeding, and low body defenses. If lymphocytosis is accompanied by neutropenia, the risk of developing a viral infection increases. Monocytopenia indicates measles, mumps and chickenpox. If the number of monocytes exceeds the norm, it is recommended to be tested for monocytic leukemia.
Mononucleosis of infectious pathogenesis is accompanied by enlarged lymph nodes, weakness, and sweating. The disease develops against the background of the Epstein-Barr virus. In case of serious poisoning, the value of the relative and absolute level of lymphocytes increases.
The chronic course of lymphocytosis is provoked by a sluggish infection, immunodeficiency, and cancer. The patient experiences constant weakness. The clinical picture for any etiology is individual.
Diagnostics
When contacting a physician, diagnosis begins with a physical examination and medical history. The presence of lymphocytosis can only be determined through clinical studies. To do this, the patient donates blood for a general clinical blood test. Collect material in the morning. Before the analysis, the patient must inform the attending physician about what medications he took during the day. This information is important because taking certain medications affects your white blood cell count and can skew your results.
In addition to the general detailed clinical analysis, the following studies are carried out:
- for the presence of antibodies;
- immunophenotyping of lymphocytes to determine cell structure and lymphoblast profile;
- cytological examination of lymph node tissue - to exclude malignant tumors;
- bone marrow myelogram for comparison with the clinical picture provided by a peripheral blood test;
- if monocytes and lymphocytes exceed normal values, then this gives reason to assume that the patient has myelodysplastic syndrome or monocytic leukemia.
The diagnosis is made based on the following points:
- An increase in the blood lymphocyte formula and a decrease in the number of platelets - thrombocytopenia, indicates hypersplenism and autoimmune thrombocytopenic purpura. Hypersplenism is when the spleen quickly disposes of dead or spent blood cells along with healthy cells. It is also an accompanying symptom of liver diseases, blood diseases, spleen injuries and some types of lymphomas and leukemia.
Spleen in the human body
- Leukopenia, which is a symptom of a complication of a viral disease, including tuberculosis.
- Simultaneous increase in the level of red blood cells and lymphocytes. It is observed in bacterial and viral infections, which are accompanied by dehydration of the body - loose stools, vomiting, elevated body temperature, fever.
- Imbalance with a simultaneous decrease in lymphocytes and leukocytes.
Since lymphocytosis often accompanies oncological diseases, if there are no clinical symptoms of infectious diseases, the doctor prescribes additional examination:
- blood test for tumor markers;
- tomography - computed tomography or magnetic resonance imaging;
- ultrasound examination of the abdominal and pelvic organs;
- X-ray examination;
- fibrogastroduodenoscopy;
- If any formations are detected, a tissue biopsy is indicated.
Differences between absolute and relative lymphocytosis in a blood test
A few years ago I wrote how viral and bacterial infections differ according to a general blood test
, which cells become more and less numerous during various infections. The article has gained some popularity, but needs some clarification.
Even at school they teach that the number of leukocytes
should be between
4 and 9 billion
(× 109) per liter of blood.
Depending on their functions, leukocytes are divided into several types, so the leukocyte formula
(the ratio of different types of leukocytes) normally in an adult looks like this:
- neutrophils (total 48-78%): young (metamyelocytes) - 0%,
- stab - 1-6%,
- segmented - 47-72%,
For example, a general blood test revealed 45%
lymphocytes. Is it dangerous or not? Should we sound the alarm and look for a list of diseases in which the number of lymphocytes in the blood increases? We’ll talk about this today, because in some cases such deviations in blood tests are pathological, while in others they do not pose a danger.
Stages of normal hematopoiesis
Let's look at the results of a general (clinical) blood test for a 19-year-old guy
, a patient with type 1 diabetes mellitus. The analysis was done at the beginning of February 2020 in the Invitro laboratory:
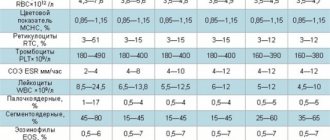
Analysis, the indicators of which are discussed in this article
In the analysis, indicators that differ from normal values are highlighted in red. Now in laboratory studies the word “ norm”
" is used less frequently, it is replaced by "
reference values
" or "
reference interval
".
This is done so as not to confuse people, because depending on the diagnostic method used, the same value can be either normal or abnormal. Reference values are selected in such a way that they correspond to the test results of 97-99%
of healthy people.
Let's look at the analysis results highlighted in red.
Hematocrit
Hematocrit
-
the proportion of blood volume accounted for by the formed elements of blood
(erythrocytes, platelets and platelets).
Since there are many more red blood cells (for example, the number of red blood cells in a unit of blood exceeds the number of white blood cells by a thousand times
), then in fact the hematocrit shows what part of the blood volume (in%) is occupied by
red blood cells
.
In this case, the hematocrit is at the lower limit of normal, and other indicators of red blood cells are normal, so a slightly reduced hematocrit can be considered a normal variant
.
Lymphocytes
In the above blood test, 45.6% lymphocytes
.
This is slightly higher than normal values (18-40% or 19-37%) and is called relative lymphocytosis
. It would seem that this is a pathology? But let's count how many lymphocytes are contained in a unit of blood and compare them with the normal absolute values of their number (cells).
The number (absolute value) of lymphocytes in the blood is: (4.69 × 109 × 45.6%) / 100 = 2,14
× 109/l.
We see this figure at the bottom of the analysis; reference values are indicated nearby: 1.00-4.80
. Our result of 2.14 can be considered good, because it is almost in the middle between the minimum (1.00) and maximum (4.80) level.
So, we have relative lymphocytosis (45.6% greater than 37% and 40%), but no absolute lymphocytosis (2.14 less than 4.8). In this case, relative lymphocytosis can be considered a normal variant
.
Neutrophils
The total number of neutrophils is calculated as the sum of young (normally 0%), band (1-6%) and segmented neutrophils (47-72%), their total 48-78%
.
Stages of granulocyte development
In the blood test under consideration, the total number of neutrophils is equal to 42,5%
. We see that the relative (%) content of neutrophils is below normal.
Let's count the absolute number of neutrophils
per unit of blood: 4.69 × 109 × 42.5% / 100 =
1.99
× 109/l.
There is some confusion regarding the proper absolute number of lymphocyte cells.
1) Data from the literature.
Leukocyte content
in adults it is normal:
| Relative amount (in%) | Absolute count (cells × 109/l) | |
| Neutrophils (total): | 48-78% | 2.04-5.8 |
| band neutrophils | 1-6% | 0.04-0.3 |
| segmented neutrophils | 47-72% | 2.0-5.5 |
| Eosinophils | 0.5-5.0% | 0.02-0.3 |
| Basophils | 0-1% | 0-0.065 |
| Lymphocytes | 19-37% | 1.2-3.0 |
| Monocytes | 3-11% | 0.09-0.6 |
2) Reference values for the number of cells from the analysis of the Invitro laboratory
(see blood test):
- neutrophils: 1.8-7.7
× 109/l.
3) Since the above figures do not coincide (1.8 and 2.04), let’s try to calculate the limits of normal cell number values ourselves.
- The minimum acceptable number of neutrophils is the minimum of neutrophils ( 48%
) of the normal minimum of leukocytes (4 × 109/l), that is,
1.92
× 109/l. - The maximum acceptable neutrophil count is 78%
of the normal maximum white blood cell count (9 × 109/L), that is,
7.02
× 109/L.
In patient analysis 1.99
× 109 neutrophils, which in principle corresponds to normal cell numbers.
below 1.5
× 109/L
is considered clearly pathological neutropenia
). A level between 1.5 × 109/L and 1.9 × 109/L is considered intermediate between normal and pathological.
Should we panic that the absolute number of neutrophils is around
the lower limit of the absolute norm?
No. With diabetes
(and also with alcoholism), a slightly reduced level of neutrophils is quite possible.
To make sure that fears are unfounded, you need to check the level of young forms: normally young neutrophils
(metamyelocytes) are 0% and
band neutrophils
are from 1 to 6%. The commentary to the analysis (does not fit in the figure and is cropped to the right) states:
A blood test using a hematology analyzer did not reveal any pathological cells. The number of band neutrophils does not exceed 6%.
For the same person, the indicators of a general blood test are quite stable: if there are no serious health problems, then the results of tests done at intervals of six months to a year will be very similar. The subject had similar blood test results several months ago.
Thus, the considered blood test, taking into account diabetes mellitus, stability of results, the absence of pathological forms of cells and the absence of an increased level of young forms of neutrophils, can be considered almost normal
.
But if doubts arise, you need to observe the patient further and order a repeat
general blood test (if an automatic hematology analyzer is not able to identify all types of pathological cells, then the analysis should be additionally examined under a microscope manually, just in case).
a bone marrow puncture
is taken to study hematopoiesis .
Reference data for neutrophils and lymphocytes
Neutrophils
The main function of neutrophils is to fight bacteria
by
phagocytosis
(absorption) and subsequent digestion.
Dead neutrophils make up a significant part of the pus
during inflammation.
Neutrophils are “ simple soldiers
” in the fight against infection:
- there are a lot of them
(every day about 100 g of neutrophils are formed in the body and enter the bloodstream, this number increases several times during purulent infections); - they do not live long
- they circulate in the blood for a short time (12-14 hours), after which they are released into the tissues and live for several more days (up to 8 days); - many neutrophils are released with biological secretions - sputum, mucus;
- The complete development cycle of a neutrophil to a mature cell takes 2 weeks
.
Normal neutrophil
in the blood of an adult:
- young (metamyelocytes)
neutrophils - 0%, - band
neutrophils - 1-6%, - segmented
neutrophils - 47-72%, - total
neutrophils - 48-78%.
Leukocytes containing specific granules in the cytoplasm are classified as granulocytes
.
Granulocytes are neutrophils, eosinophils, basophils
.
Agranulocytosis
- a sharp decrease in the number of granulocytes in the blood until they disappear (less than 1 × 109/l of leukocytes and less than 0.75 × 109/l of granulocytes).
The concept of neutropenia is close to the concept of agranulocytosis
(
reduced number of neutrophils
- below 1.5 × 109/l).
Comparing the criteria for agranulocytosis and neutropenia, one can guess that only severe neutropenia will lead to agranulocytosis
.
To give the conclusion “ agranulocytosis
”, a moderately reduced level of neutrophils is not enough.
Causes
decreased number of neutrophils (
neutropenia
):
- severe bacterial infections,
- viral infections (neutrophils do not fight viruses. Cells affected by the virus are destroyed by certain types of lymphocytes),
- inhibition of hematopoiesis in the bone marrow ( aplastic anemia
-
a sharp inhibition or cessation of the growth and maturation of all blood cells in the bone marrow
), - autoimmune diseases ( systemic lupus erythematosus, rheumatoid arthritis,
etc.), - redistribution of neutrophils in organs ( splenomegaly
- enlarged spleen), - tumors of the hematopoietic system:
- chronic lymphocytic leukemia
(a malignant tumor in which the formation of atypical mature lymphocytes occurs and their accumulation in the blood, bone marrow, lymph nodes, liver and spleen. At the same time, the formation of all other blood cells is inhibited, especially those with a short life cycle - neutrophils); - acute leukemia
(a bone marrow tumor in which a mutation of a hematopoietic stem cell occurs and its uncontrolled reproduction without maturation into mature forms of cells. Both the common stem cell-precursor of all blood cells and later varieties of precursor cells in individual blood sprouts can be affected. The bone marrow is filled with immature blast cells, which displace and suppress normal hematopoiesis); - deficiencies of iron and some vitamins ( cyanocobalamin, folic acid
), - effect of medications ( cytostatics, immunosuppressants, sulfonamides
, etc.) - genetic factors.
An increase in the number of neutrophils in the blood (above 78% or more than 5.8 × 109/L) is called neutrophilia
(
neutrophilia, neutrophilic leukocytosis
).
4 mechanisms of neutrophilia
(neutrophilia):
- increased
neutrophil formation:
- bacterial infections,
- inflammation and tissue necrosis ( burns, myocardial infarction
), - chronic myeloid leukemia
(
a malignant bone marrow tumor in which there is an uncontrolled formation of immature and mature granulocytes - neutrophils, eosinophils and basophils, displacing healthy cells
), - treatment of malignant tumors (for example, with radiation therapy),
- poisoning (exogenous origin - lead, snake venom
, endogenous origin - uremia, gout, ketoacidosis),
- active migration
(early exit) of neutrophils from the bone marrow into the blood, - redistribution
of neutrophils from the parietal population (near blood vessels) into the circulating blood: during stress, intense muscular work. - slowing down
the release of neutrophils from the blood into tissues (this is how
glucocorticoid
, which inhibit the mobility of neutrophils and limit their ability to penetrate from the blood into the site of inflammation). - development of leukocytosis
- an increase in the total number of leukocytes (above 9 × 109/l) mainly due to
neutrophilia
- an increase in the number of neutrophils; - shift of the leukocyte formula to the left
- an increase in the number of young [
young + band
] forms of neutrophils. The appearance of young neutrophils (metamyelocytes) in the blood is a sign of a severe infection and evidence that the bone marrow is working under great strain. The more young forms (especially young ones), the greater the stress on the immune system; - the appearance of toxic granularity
and other
degenerative changes in neutrophils
(
Dele bodies, cytoplasmic vacuoles, pathological changes in the nucleus
).
Contrary to the established name, these changes are not caused by the “ toxic effect
” of bacteria on neutrophils, but
by impaired cell maturation
in the bone marrow. The maturation of neutrophils is disrupted due to a sharp acceleration due to excessive stimulation of the immune system by cytokines, therefore, for example, toxic granularity of neutrophils appears in large quantities during the disintegration of tumor tissue under the influence of radiation therapy. In other words, the bone marrow prepares young “soldiers” to the limit of their capabilities and sends them “into battle” ahead of schedule.
For purulent bacterial infections
characteristic:
Drawing from the site bono-esse.ru
Lymphocytes
Lymphocytes
are the second most numerous leukocytes in the blood and come in different subtypes.
Brief classification of lymphocytes
Unlike neutrophils, the “soldiers,” lymphocytes can be classified as “officers.” Lymphocytes “learn” longer (depending on the functions they perform, they are formed and multiply in the bone marrow, lymph nodes, spleen) and are highly specialized cells ( antigen recognition, initiation and implementation of cellular and humoral immunity, regulation of the formation and activity of cells of the immune system
). Lymphocytes are able to leave the blood into the tissues, then into the lymph and with its current return back to the blood.
To decipher a general blood test, you need to have an idea of the following:
- 30% of all peripheral blood lymphocytes are short-lived forms (4 days). These are the majority of B lymphocytes and T suppressor cells.
- 70% of lymphocytes are long-lived
(170 days = almost 6 months). These are other types of lymphocytes.
Of course, with a complete cessation of hematopoiesis, the level of granulocytes in the blood first drops
, which becomes noticeable precisely by the number
of neutrophils
, since
there are normally very few
eosinophils and basophils of red blood cells
(live up to 4 months) and
lymphocytes
begins to decrease . For this reason, bone marrow damage is detected by severe infectious complications, which are very difficult to treat.
Since the development of neutrophils is impaired earlier than other cells ( neutropenia
- less than 1.5 × 109/l), then blood tests most often reveal
relative lymphocytosis
(more than 37%), and not absolute lymphocytosis (more than 3.0 × 109/l).
Causes
increased level of lymphocytes (
lymphocytosis
) - more than 3.0 × 109/l:
- viral infections,
- some bacterial infections ( tuberculosis, syphilis, whooping cough, leptospirosis, brucellosis, yersiniosis
), - autoimmune connective tissue diseases ( rheumatism, systemic lupus erythematosus, rheumatoid arthritis
), - malignant tumors,
- side effects of drugs,
- poisoning,
- some other reasons.
Causes
reduced level of lymphocytes (
lymphocytopenia
) - less than 1.2 × 109/l (according to less strict standards 1.0 × 109/l):
- aplastic anemia,
- HIV infection (primarily affects a type of T lymphocyte called T helper cells
) - malignant tumors in the terminal (last) phase,
- some forms of tuberculosis,
- acute infections,
- acute radiation sickness,
- chronic renal failure (CRF) in the last stage,
- excess glucocorticoids.
Treatment
It is not lymphocytosis itself that should be treated, but the disease that caused it. Because, as stated above, pathology is not an independent disease.
Pediatric physiological lymphocytosis does not require therapy. In other cases, the doctor will prescribe treatment after diagnosis.
For infectious diseases, depending on the indications, antibiotics, antiviral and anti-inflammatory drugs, sulfonamides are prescribed; for viral infections, drugs based on M2 channel blockers and interferon are prescribed. Antifungal medications may be prescribed. It is recommended to drink plenty of fluids and take medications that relieve intoxication, eliminate pain and reduce body temperature.
For tuberculosis – special specific therapy DOTS + therapy.
For a malignant tumor - fungicides, immunosuppressants, antibiotics and cytotoxic drugs, chemotherapy, and in some cases, bone marrow transplantation.
Folk remedies for the treatment of lymphocytosis
Treatment of an increased number of lymphocytes is possible only under the supervision of a doctor using special medications for adults and children, as well as folk remedies. One of such effective drugs is an infusion of caranthus flower leaves.
To prepare the tincture, take dried inflorescences and vodka in a ratio of 1:20. The ingredients are thoroughly mixed and infused for about ten days, after which the strained tincture should be taken ten drops in a glass of water for three weeks. This folk remedy relieves clinical symptoms and normalizes the composition of the bloodstream.
Prevention
To prevent the occurrence of lymphocytosis, it is necessary to systematically carry out measures to strengthen the immune system:
- normalization of work and rest schedules;
- avoiding excessive use of tobacco and alcohol;
- compliance with personal hygiene rules;
- systematic physical activity;
- proper nutrition, rich in selenium, zinc, potassium, magnesium, vitamins;
- annual preventive examinations;
- During seasonal illnesses, you need to avoid crowded places, wash your hands after each visit to such places, and take a course of vitamin supplements.
If, during a medical examination, a blood test showed a shift in the leukocyte formula, one or a complex of symptoms was discovered with weakness that a person cannot explain, a constant temperature, you should consult a doctor. Early detection of the disease increases the chances of a quick recovery.
In addition, the doctor can rule out diseases in principle and prescribe preventive procedures, and the level of lymphocytes will return to normal.
Types and characteristics of lymphocytes
Lymphocytosis is an excess of the norm of lymphocytes in the blood, which occurs against the background of the development of an inflammatory or infectious disease in the body. Lymphocytosis has no specific symptoms.
Detection of an increased level of lymphocytes in the blood occurs through a general analysis, during which not only the number of leukocytes is assessed, but also the combination of their existing types.
Normally, white cells in the blood of an adult make up 19–37% of the total number of leukocytes.
If there are minor deviations in the blood from the given indicators, then this condition is not considered a pathology.
Currently, there are three types of lymphocytes in the blood:
- T-lymphocytes - the volume of T-cells in the blood of the total number of lymphocytes is approximately 80%, these cells develop in the thymus, due to which they are called thymus-dependent;
- B-lymphocytes - cells mature and develop in the bone marrow, their number in the peripheral blood is approximately 15% of the total number of lymphocytes;
- NK lymphocytes - their number from the total number of white cells in the blood is 10 - 15%; the peculiarity of antibody-independent cells is their ability to kill malignant tumor cells.
T cells are divided into killer, helper and suppressor cells. The first ones find and kill foreign and infected cells in the blood, which helps prevent the spread of infection throughout the body.
Helper cells transmit a signal to cellular immunity about the penetration of foreign agents into the body.
Suppressor cells are able to recognize the body's own cells and agents that suppress autoimmune processes.
B cells represent the cellular basis of humoral immunity, the purpose of which is to destroy bacteria living in the extracellular space and blood.
Formed in the bone marrow, B lymphocytes are transported to the lymphoid peripheral organs for final maturation.
Under the influence of helper cells, they transform into plasma cells and begin to produce antibodies called immunoglobulins.
The purpose of the latter is to neutralize viruses, bacteria and toxin molecules in the blood, after which toxic agents destroy leukocyte-phagocyte cells.
READ What are the reasons for an increase in red blood cells in a child’s blood?
There are the fewest natural killer cells or NK lymphocytes in the peripheral blood - only 10% of the total number.
NK cells have cytotoxicity - a defense mechanism that can kill the pathogen from within its cell.
In addition, NK lymphocytes can recognize their own cells that have been infected with a virus or formed with the growth of an oncological tumor.
Lymphocyte cells acquire immunity and form it, after which, upon repeated infection with the same type of virus, a strong and rapid immune response from the body to the invasion of the pathogen follows.
Symptoms
Relative lymphocytosis is common, as many factors can influence the reduction of other white blood cells. This symptom occurs more often in adults and children under two years of age.
The reasons for such a blood test can characterize various diseases:
- viral infections;
- inflammation with pus;
- rheumatism;
- typhoid fever;
- brucellosis;
- Addison's disease;
- pathology of the thyroid gland.
If relative lymphocytosis is detected, then in order to bring the number of cells back to normal, it is necessary to identify the main causes of this phenomenon. Therefore, you need to undergo a comprehensive examination. To confirm the results, you need to take a blood test again and compare the clinical picture. After all, laboratory results often come back false.
Typically, lymphocytosis does not manifest itself in any way, and it is diagnosed during a blood test, but sometimes symptoms of the underlying disease may appear. These signs are often complained to the doctor.
The infection is characterized by fever, enlarged tonsils and lymph nodes, and weakness and nausea. A rash and redness of the skin may appear on the patient's skin. Fever, chills, and rapid weight loss often occur. Sometimes the liver or spleen becomes enlarged.
Therefore, it is important, in addition to the main symptoms, to check all indicators and conduct additional examinations to make the correct diagnosis. In this case, the treatment will be effective and the lymphocyte parameters will return to normal.
Factors provoking lymphocytosis and its symptoms
A condition in which the percentage of white blood cells in the peripheral blood increases is caused by the following reasons:
- infections of various types;
- serious diseases such as HIV infection;
- after blood transfusions caused by large blood losses;
- irregular meals, diets, fasting;
- long-term use of medications that change the composition of the blood;
- avitaminosis;
- abuse of bad habits;
- disorders of the central and peripheral nervous system causing mental illness.
It cannot be said that the condition of lymphocytosis has certain symptoms. It is discovered rather by chance, during examinations to identify the underlying disease. In adults, it is possible to suspect a similar condition if, during a non-severe illness, the acute period, characterized by a febrile state and elevated temperature, lasts up to 7-9 days.
But infectious lymphocytosis in a small child is quite pronounced. At the beginning of the infectious process, along with the characteristic symptoms of this disease, respiratory tract pathology develops, shortness of breath appears, and heavy breathing is observed.