Pericarditis
This is a serious and dangerous heart disease that can become chronic and cause heart failure.
The pericardium is the outer lining of the heart that holds it in position and prevents it from enlarging in situations of overload. The pericardium consists of two membranes. There is liquid between them. It acts as a lubricant and prevents the membranes from rubbing against each other during intense stress on the heart.
The norm of fluid in the pericardial cavity is 20 ml. If the volume of liquid exceeds this figure, then we can talk about the development of some pathologies that are worth considering in more detail.
The causes of pericarditis are not well known to medicine. It is only known that an increase in fluid volume can be provoked by diseases such as scarlet fever, influenza, rheumatism, lupus, and various types of infections. The pathology can occur against the background of pleurisy, vitamin deficiency, or measles.
Acute form
Classification according to the type of course divides the disease into acute and chronic forms. Acute pericarditis is characterized by sudden development and rapid progression. It can begin after a viral infection or against the background of advanced rheumatism or tuberculosis. The pericardial sac becomes inflamed due to the pathogen entering it.
Diseases that often cause acute inflammation:
- sepsis;
- streptococcal sore throat;
- measles;
- helminthic infestation;
- fungus;
- staphylococcal infection;
- purulent process.
Often the acute form develops against the background of pneumonia, after suffering from an acute respiratory infection or influenza. The risk group includes people with a hereditary predisposition, as well as those suffering from autoimmune diseases.
Among all the types of pathology, there are those about which patients have the most questions.
Episthenocardiac variant
The development of pathology usually occurs within several hours or several days with acute myocardial infarction. Dry epistenocardial pericarditis is most often diagnosed, but an exudative course is also possible.
A typical symptom is pain in the heart, which intensifies with inspiration and during coughing. Pain during myocardial infarction has a different character: it is intense all the time.
Epistenocardial pericarditis often develops in patients with myocardial infarction.
This option is characterized by complications: thromboebolic syndrome, left ventricular aneurysm. This type of inflammation may indicate a not very good prognosis for myocardial infarction, but this is not always the case, depending on the period in which EP developed and how large the amount of fluid in the pericardial cavity is.
Pericardial effusion is observed in patients who have had myocardial infarction for the following reasons:
- myocardial rupture;
- anticoagulant therapy performed;
- fibrinolytic therapy.
When fluid accumulates quickly in the heart, tamponade can develop. The likelihood of this pathology is especially high if myocardial rupture occurs in the area of necrosis. The epistenocardiac variant of the disease may be accompanied by atrioventricular conduction disturbances and atrial fibrillation.
Tuberculous
More often, this type develops in men suffering from pulmonary tuberculosis: it is found in 10% of such patients. HIV carriers are also at risk.
Among the factors causing cardiac tamponade, constrictive and acute pericarditis, tuberculosis is also one of the leading ones: it causes the pathology in 7%, 6% and 4% of cases, respectively.
Tuberculous pericarditis develops due to the fact that pathogenic microorganisms penetrate with the lymphatic fluid or move directly from the lungs, bronchi, pleura or lymph nodes .
Less commonly, lesions can be localized in bone structures, joints and the genitourinary system. As a rule, the disease occurs in an acute form. Symptoms and processes are similar to those observed in acute fibrinous pericarditis, with the exception of pain - it is not so pronounced.
Exudate accumulates in large quantities; after removal, the pericardial effusion continues to flow, but this does not always entail cardiac tamponade.
Tuberculous pericarditis is manifested by the following symptoms:
- sudden weight loss;
- ascites;
- profuse sweating, especially during sleep;
- poor appetite;
- coughing up blood;
- low-grade fever;
- calcification of the lining of the heart;
- hepatomegaly.
This form of inflammation progresses slowly.
Adhesive
Pericarditis of various etiologies can develop into adhesive pericarditis. When the underlying disease passes from the acute stage to the chronic stage, a tissue structure forms in the cavity, which gradually turns into a scar. At the same time, another process occurs - adhesion of the pericardial sheets , accompanied by the formation of adhesions. Adhesive pericarditis often develops after heart surgery.
Prognosis and treatment vary depending on the patient's condition. If the heart is of normal size, physiological abnormalities usually do not occur. In some cases, pathological processes in the pericardium can impede blood flow, for example, by squeezing the heart and preventing its contractions. Adhesive pericarditis, which developed as a consequence of an infectious disease, may be accompanied by fever, weakness, chills, and fever.
Kinds
Like any other disease, pericarditis should be distinguished:
- According to the clinical manifestation: fibrinous pericarditis (dry) and exudative (effusion).
- According to the nature of the course: acute and chronic.
Pericarditis may be accompanied by an inflammatory process, resulting in the deposition of lime in the cardiac lining. In this situation, the volume of liquid can reach one liter, which will cause fatal complications in the body.
Only a specialist can determine whether the fluid in the pericardium is normal or not.
Types of disease
The normal amount of fluid in the pericardium in adults is less than twenty milliliters, but this volume often increases. The following pathologies may be the reason for this:
- autoimmune diseases;
- injuries, in particular chest wounds;
- parasites, fungi, bacteria and various viruses;
- diabetes mellitus, Addison's disease, myxedema;
- tumors or metastases of the pericardium;
- idiopathic pericarditis, the causes of which are unknown to science to this day;
- lung diseases, transmissible myocardial infarction, aortic aneurysm.
It is worth noting that the amount of fluid in the heart can increase greatly (exudative pericarditis), increase slightly with an increase in protein in it (fibriosis pericarditis), or decrease (dry pericarditis).
General symptoms
Each type of pericarditis is characterized by certain symptoms, they are different. But there are primary signs of pericarditis that are common to all types of the disease:
- Headache.
- General weakness.
- Weakness and muscle pain.
- Dyspnea.
- Dry cough.
- Irregular heartbeat.
- Fever.
- Friction noises in the pericardial area.
Often the patient does not seek help from a specialist because he confuses these symptoms with other less serious diseases. After taking antipyretic and painkillers that do not bring the desired result, the patient goes to the doctor. Unfortunately, for many people at this moment the pathology takes on a chronic form, the treatment of which is a rather long and labor-intensive process.
Causes
There are many causes of this disease:
- microorganisms that parasitize connective tissue (tuberculosis bacilli, pathogens of tick-borne borreliosis, chlamydia, treponemes of syphilis, bacteria that cause brucellosis);
- serum sickness;
- bacterial infections (streptococci, pneumococci, staphylococci);
- mycoplasmas, influenza viruses, adenoviruses, helminths, etc.;
- lupus, scleroderma, rheumatoid arthritis.
Currently, medicine is quite developed and successfully treats heart pathologies. Previously, when doctors did not have the necessary equipment, the presence of normal fluid in the pericardium of the heart was determined by listening. A large amount of liquid can be heard, it is accompanied by noise and hum that can be heard at a distance.
In addition to the above-mentioned causes of pericarditis, myocardial infarction, pneumonia, and pleurisy can lead to abnormal fluid levels in the pericardium in adults.
Why is it dangerous?
One of the most serious complications of pericarditis can be cardiac tamponade. This is a dangerous disease in which compression of the organ occurs. The patient feels shortness of breath when walking. After the accumulation of a large amount of fluid and strong compression of the heart, shortness of breath appears even at rest. There is a decrease in cardiac output, as the myocardium of the left ventricle does not have enough blood.
If this disease is detected, the doctor is obliged to hospitalize the patient. Treatment consists of directly pumping out the accumulated fluid.
Treatment methods
To cure the patient, use:
- Conservative therapy:
- antibiotics (if microorganisms are present in the pericardial fluid);
- anti-inflammatory drugs;
- cytostatic drugs (in the presence of a tumor).
- Operative methods:
- pericardial puncture (to evacuate excess fluid);
- surgical correction (excision of cysts, tumors);
- pericardotomy (to remove excess fluid and provide access to the heart);
- pericardectomy (“separation” - separation of the hardened bag with an armored heart).
Dry and exudative
With the development of dry pericarditis, the patient experiences a dull pain in the heart area, which only intensifies over time. The use of nitroglycerin is useless. This is worth paying attention to. The pain symptom intensifies when taking a horizontal position and decreases when bending forward. Coughing and inhaling only intensifies the pain.
The specialist can observe the following picture: the patient is sitting, leaning forward, he is shivering, and there is an increased body temperature. When listening to the heart, a creaking sound similar to the grinding of snow is observed. The patient needs to hold his breath so that the doctor is convinced of the correctness of the diagnosis. The fact is that such a creaking can be confused with friction of the pleura. But the creaking with dry pericarditis is constant and does not stop when you hold your breath.
With exudative pericarditis, symptoms may not be very noticeable. The accumulation of exudate provokes divergence of the pericardial layers, which helps reduce the pain symptom. Sometimes the pain may disappear completely, but not for long. After some time, heaviness appears in the heart area, and the patient experiences shortness of breath. Shortness of breath is observed first during physical activity, and then at rest. The pericardium, swollen with fluid, begins to compress organs close to the heart, accompanied by hiccups, a strong barking cough, and weakness in the voice.
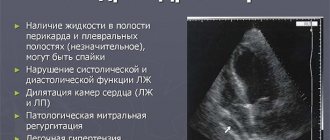
Pericarditis in the practice of a rheumatologist
Etiology The leading etiological role in the development of pericarditis is played by a variety of infectious agents, primarily viruses: Coxsackie A9, B 1–4, ECHO 8, mumps, chickenpox, rubella, human immunodeficiency, Epstein–Barr, cytomegalovirus, parvovirus B 19, etc. (Table 1). Among the non-infectious causes of pericarditis, systemic inflammatory rheumatic diseases (RDs) occupy an important place, in which the incidence of pericardial involvement in the process can reach 50–80%. Clinical manifestations Depending on the clinical picture, the following types of pericarditis are distinguished [2]: • acute (duration less than 6 weeks): – dry or fibrinous, – exudative (serous-fibrinous, hemorrhagic and purulent); • subacute and chronic (duration more than 6 weeks): – exudative, – adhesive (non-constrictive), – constrictive. The main complaint of patients with acute dry pericarditis is a dull pressing pain in the heart area radiating to both shoulders, the trapezius muscle area, and the neck. It intensifies with deep breathing and may be accompanied by shortness of breath, dry cough, chilling, which makes the clinical picture similar to that of acute left-sided pleurisy. Important features of pain during pericarditis, in contrast to angina attacks, are: gradual increase, duration from several hours to several days, lack of effect from taking nitroglycerin, temporary subsidence when taking narcotic analgesics. The leading symptom of dry pericarditis is a pericardial friction rub, which can be one-, two-, or three-component. It is heard above the zone of absolute dullness of the heart and is characterized by poor conductivity (“dies in the same place where it appears”). In contrast to valvular heart defects, all components of the pericardial friction noise are similar in nature and intensity (“locomotive rhythm”). The earliest ECG changes (phase I) include an increase in the ST segment in standard leads II–III and in leads V2–6 with a reciprocal decrease in ST only in leads aVR and V1. At the same time, a decrease in the PR segment is observed in the inferolateral leads (II, III, aVF , V5–6). After about 1 week (phase II), the ST and T segments return to the isoline. After this, T wave inversion occurs in most leads (phase III). Subsequently, the ECG returns to the original one or (with chronic inflammation) the T waves remain negative (phase IV). In contrast to myocardial infarction, pericarditis is characterized by: 1) absence of changes in the QRS complex, 2) rapid dynamics of ECG changes with T wave inversion during the first two days, 3) T wave inversion ahead of the decrease to the ST segment isoline. In acute pericarditis, the following changes in laboratory parameters are possible: leukocytosis, ESR, increased levels of C-reactive protein, a2- and g-globulins, a moderate increase in parameters reflecting the inflammatory process in the heart muscle (creatine phosphokinase and its MB fraction, aspartic and alanine transaminases, lactate dehydrogenase). Depending on the suspected cause, it is also advisable to carry out the following studies: tuberculin skin test, blood culture for blood culture (for infective endocarditis), virological studies, tests for antibodies to HIV, serological tests for fungi, determination of antinuclear factor, rheumatoid factor, circulating immune complexes, antibodies to cardiolipin, antistreptolysin-O titers (for systemic RD), cold agglutinins (for mycoplasma infections), heterophilic antibodies (for mononucleosis), etc. With exudative pericarditis, the dynamics of development and severity of symptoms are primarily determined by the rate of fluid accumulation in the pericardial cavity. In cases of slow fluid accumulation, patients may not have cardiac complaints for a long time. With a fairly rapid accumulation of effusion, shortness of breath appears and increases during physical activity, and then at rest, which can decrease in a sitting position with the torso tilted forward. A dry cough occurs due to the pressure of the exudate on the trachea and bronchi. With a significant amount of exudate, percussion determines the expansion of the area of cardiac dullness in all directions. Some patients experience dullness to percussion and bronchial breathing in the area of the lower angle of the left scapula (Evart's symptom). The pericardial friction noise heard earlier (during the development of the process from the stage of dry pericarditis) may change with a change in body position, but, as a rule, does not disappear. The ECG shows a decrease in the voltage of the QRS complexes and T waves, depression of the PR segment, a change in the ST interval, as well as the phenomenon of electrical alternans. On radiography, significant effusion into the pericardial cavity appears as cardiomegaly with clear boundaries (water bottle configuration). A weakening of the pulsation of the cardiac shadow is characteristic. At the same time, a clear pulsation of the aorta is preserved. The main method for diagnosing exudative pericarditis is echocardiography (EchoCG), which detects the divergence of the pericardial layers with an effusion volume exceeding 15–35 ml. The following gradations of effusion severity are used: 1) small (divergence of pericardial layers <10 mm); 2) moderate (>10 mm posteriorly); 3) large (>20 mm); very large (>20 mm plus symptoms of cardiac compression). When pericardial fluid accumulates in a volume that impedes blood flow into the ventricles, cardiac tamponade may develop. More often it develops gradually, clinical symptoms are similar to those of heart failure. The most important sign of cardiac tamponade is “paradoxical pulse”: a decrease in systolic blood pressure by more than 10 mm Hg. during inspiration with constant diastolic blood pressure. The diagnostic algorithm for cardiac tamponade is presented in Table 2. A rare but extremely severe consequence of chronic inflammation of the pericardium, leading to impaired filling of the ventricles of the heart and a decrease in their function, is constrictive pericarditis, the diagnostic signs of which are presented in Table 3. Pericarditis in rheumatic diseases Contrary to popular belief, involvement in the pericardial process in acute rheumatic fever (ARF) is rare. It should be emphasized that currently, in accordance with WHO recommendations, the main criterion for rheumatic carditis is valvulitis, possibly in combination with myocarditis or myopericarditis (pancarditis). According to the Institute of Rheumatology, the incidence of pancarditis in ARF is 2.5–4.6% in adults [3,4] and 6.6% in children [5]. Heart damage such as myopericarditis in the absence of valvulitis is regarded as unlikely for ARF. This requires a thorough differential diagnosis with myopericarditis of another etiology, primarily viral. In patients with rheumatoid arthritis (RA), the incidence of pericardial damage ranges from 15–35% (according to echocardiography) to 50% (at autopsy). Clinically manifest pericarditis occurs in only 2-4% of cases, usually in young men with fever, subcutaneous nodules, high titers of rheumatoid factor (RF), moderate anemia and a significantly accelerated ESR. The relationship between the incidence of pericardial pathology and the duration of RA has not been established. All types of pericarditis (from dry to constrictive) have been described in RA. In some patients, pericardial damage may be the first manifestation of the disease. In the pericardial fluid, leukocytosis, high levels of protein and cytokines are detected, sugar and complement levels are usually reduced, immune complexes and rheumatoid factor may be detected. Compared with other types of exudative pericarditis (bacterial, tumor), in RA, high values of g-globulins and LDH in combination with low glucose levels are much more often detected. Most authors emphasize the clear effect of prescribing glucocorticoids (GC) and biological agents [6,7,8]. In patients with systemic lupus erythematosus (SLE), pericarditis is the most common form of heart damage, reflects the high activity of the inflammatory process and is included (along with pleurisy) in the category of classification criteria for the disease. During clinical and instrumental examination it is detected in 25–50% of cases, during autopsy - in 80%. The most common is dry pericarditis (>20%). In some patients, significant effusion into the pericardial cavity is observed, up to cardiac tamponade. LE cells, antinuclear antibodies, immune complexes, and low levels of complement are found in the pericardial fluid. With a long course of SLE and recurrent pericarditis, massive adhesions develop. This group of patients, even without an exacerbation of SLE, is characterized by persistent pain in the chest, in the side, aggravated by laughing and sneezing; Pericardial friction rub can be detected for a long time. Constrictive pericarditis requiring surgical treatment is extremely rare [6,9,10]. Pericardial lesions in systemic scleroderma (SSc) are much more often detected during sectional examination (50–70%). EchoCG detects changes in 40% of patients. The clinical symptoms of scleroderma pericarditis are scant and often absent due to the characteristics of the lesion, a small amount of fluid and the gradual protracted development of the disease; hemodynamic changes as a result are also rare. The need for pericardial puncture occurs in isolated cases. The total protein content in the pericardial fluid is less than in the blood serum, the ratio of globulin fractions (electrophoresis) is similar. It is believed that the basis of pericardial damage in SSc is the phenomena of serous-fibrinous polyserositis, as well as pericardial fibrosis with impaired transudation processes. ECG – symptoms of pericardial damage are often absent. Changes in the pericardium occur more often in patients with scleroderma nephropathy and other systemic manifestations of the disease (damage to the lungs, gastrointestinal tract, Sjogren's syndrome, etc.). It is believed that the presence of pericarditis in patients with SSc reflects the systemic nature and severity of the pathological process [6]. The frequency of pericardial lesions in other RDs is presented in Table 4. From a practical point of view, it is necessary to note the possibility of developing pericarditis at the onset of the disease, the variety of forms and variants of the course of pericardial pathology (up to tamponade and constriction), as well as in most cases a good response to GC therapy ( including megadoses). Differential diagnosis of pericarditis of various origins is presented in Table 5. Treatment The basic principles of treatment of pericarditis are reflected in Table 6. In most cases, hospitalization is required to clarify the etiology, conduct differential diagnosis, timely identify cardiac tamponade and evaluate the treatment started. The basis of treatment for acute pericarditis is non-steroidal anti-inflammatory drugs (NSAIDs) – ibuprofen 1200–2400 mg/day. and diclofenac 150 mg/day. orally, prescribed for an average of 3 weeks until the pericardial effusion disappears. In patients with ulcerative lesions of the gastrointestinal tract, NSAIDs related to selective cyclooxygenase-2 inhibitors (meloxicam, nimesulide) can be used. If NSAIDs are ineffective and the process progresses, they begin (after clarifying the etiology!) treatment with prednisolone at a dose of 1–1.5 mg/kg/day. for 5–7 days, followed by a reduction of 2.5 mg every 5 days until discontinuation. The total duration of the course of hormone therapy is at least 3 months. With the development of pericarditis as part of a systemic connective tissue disease, the dose of GCs and the duration of treatment with these drugs is determined by the severity and activity of the underlying rheumatic pathology. In most patients with viral pericarditis, rapid positive dynamics are observed against the background of anti-inflammatory therapy and, as a rule, specific treatment is not required. In case of purulent pericarditis, it is necessary to drain the pericardial cavity and rinse it with saline solution in combination with antimicrobial therapy. The course of antimicrobial therapy should be continued until the febrile syndrome, other clinical signs of the disease are eliminated and the number of peripheral blood leukocytes is normalized. Pericardiocentesis is indicated for clinical symptoms of cardiac tamponade, a suspected diagnosis of purulent or tuberculous pericarditis, a large volume of effusion (pericardial divergence in diastole on EchoCG >20 mm), persisting for more than 1 week, despite drug therapy. Pericardiectomy is necessary in patients with dense adhesions, localized effusion, recurrent tamponade, persistent infection, and progressive compression of the heart. Perioperative mortality with pericardiectomy in combination with antibiotics is 8%. To treat patients with tuberculous pericarditis, various combinations of drugs are used, which should be prescribed only with a confirmed diagnosis. According to a meta-analysis that included patients with effusion and constrictive tuberculous pericarditis, treatment with tuberculostatic drugs in combination with GC is associated with lower mortality and less need for pericardiocentesis and pericardiectomy. If the decision to prescribe prednisolone is positive, the drug is used in relatively high doses (1–2 mg/kg/day), because Rifampicin enhances its metabolism in the liver. On days 5–7 of treatment, the dose of prednisolone begins to be gradually reduced until discontinuation after 6–8 weeks. If compression of the heart develops, pericardiectomy is performed [15]. The prognosis for acute viral pericarditis is usually favorable. In case of cardiac tamponade, emergency pericardial puncture improves the prognosis. The 5-year survival rate of patients with constrictive pericarditis after pericardiectomy is 75%, the 10-year survival rate is 57% [2]. In chronic obstructive pulmonary disease, the velocity of mitral blood flow decreases by almost 100% during inspiration and increases during expiration. In this case, the E value is maximum at the end of exhalation (with constrictive pericarditis, the E value is maximum immediately at the beginning of exhalation). In addition, blood flow through the superior vena cava in chronic obstructive pulmonary disease increases during exhalation, while in constrictive pericarditis does not change significantly during breathing.
References 1. Maisch B, Seferovic PM, Ristic AD, et al. Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology.// Eur Heart J. 2004 Apr;25(7):587–610. 2. Gogin E.E. Pericardial diseases. In the book: Rational pharmacotherapy of cardiovascular diseases. M., Litterra, 2004: 465–482.. 3. Asadov A.G. Physical performance of patients with rheumatic carditis. Author's abstract. Dissertation of Candidate of Medical Sciences. M., 1984. 22 p. 4. Dzhuzenova B.S., Kotelnikova G.P., Mikhailova I.N., Nasonova V.A. Acute rheumatic carditis in young men. Ter. archive.1992;4: 58–62. 5. Medyntseva L.G. Physical performance of children with rheumatism at the stage of medical examination. Author's abstract. dissE. Ph.D. honey. Sci. M, 1990. 24 s. 6. Sigidin Ya, A., Guseva N.G., Ivanova M.M. Diffuse connective tissue diseases (systemic rheumatic diseases): a guide for doctors. M., Medicine, 2004. 640 p. 7. Guedes C., Dianchi-Fior P., Cormier B. et al. Cardiac manifestations of rheumatoid arthritis: A case–control transesophageal echocardiography study in 30 patients. Arthritis Care Res. 2001; 45(2): 129–135. 8. McRorie ER Wright RA, Errington ML, Luoqmani RA Rheumatoid constrictive pericarditis. Br.J.Rheumatol.1997; 36: 100–103. 9. Kahl LE. The spectrum of pericardial tamponade in systemic lupus erythematosus. Report of ten patients. Arthritis Rheum. 1992 Nov;35(11):1343–9. 10. Moder KG, Miller TD, Tazelaar HD. Cardiac involvement in systemic lupus erythematosus. Mayo Clin Proc. 1999; 74(3):275–284. 11. Pagnoux C., Guillevin L. Cardiac involvement in small and medium-sized vessel vasculitides. Lupus. 2005; 14: 718–722. 12. Efthimiou P, Paik PK, Bielory L. Diagnosis and management of adult onset Still's disease. Ann Rheum Dis. 2006; 65(5):564–572. 13. Drout MH, Hachulla E., Houvenagel E. et al [Cardiac complications in adult onset Still disease: from periarditis to tamponade as manifestations. Rev Med Interne. 1994; 15(11): 740–743. 14. Gyongyosi M., Pokorny G., Jambrik Z et al. Cardiac manifestations in primary Sjogren syndrome. Ann Rheum Dis 1996; 55(7): 450–454. 15. Mayosi BM, Nisekhe M, Volmink JA et al. Interventions for treating tuberculous pericarditis. Cochrane Database Syst Rev 2002; (4): CD000526
Pericarditis in children
How much fluid is normal in the pericardium in children? Many parents ask this question. In children, the amount of fluid in the pericardium is normal if it does not exceed twenty milliliters.
The disease in children is accompanied by the following symptoms:
- the pain symptom is more developed in the abdominal area, the child does not feel pain in the heart;
- sleep disturbance, with the child lying on his stomach because he cannot sleep on his back;
- nausea, vomiting, regurgitation.
Diagnostic methods
Upon admission to the hospital, an ECHO-CG must be urgently performed and the degree of impairment assessed. Then a puncture is performed and the person is further examined for the etiological factor in order to prescribe treatment and prevent relapse. In less severe cases, there is time for some research.
List of events:
- Oral survey.
- Anamnesis collection. Past pathologies, chest injuries, bad habits, and other issues.
- Measurement of blood pressure and heart rate.
- Echocardiography. Basic technique. The anatomical condition of the shell is assessed. A typical violation is detected. The separation of the pericardial layers is normally 3-5 mm. With dropsy, the indicator increases to 10-20 mm or more, which is the absolute basis for a puncture.
As part of an extended diagnosis aimed at determining the origin of the problem, a general blood test (hemoglobin, ESR, red blood cells are subject to evaluation), biochemistry, and testing for thyroid and adrenal hormones are indicated.
Chest X-ray. If injuries are suspected, it is prescribed at the first moment.
Also ultrasound of the abdominal cavity and kidneys. Evaluation of urine allows us to talk about the degree of preservation of the functional state of the excretory tract.
After the puncture, the obtained sample from the pericardium is examined. According to its characteristics, it is a transudate. It differs from exudate in its low density and low protein content. Based on these data, it is possible to draw some conclusions about the nature of the root cause.
Causes of childhood pericarditis
The causes of childhood pericarditis can be the following diseases:
- dysfunction of the thyroid gland;
- lack of vitamins;
- heredity;
- various blood diseases;
- tumors of the heart, pericardium;
- hormonal disbalance;
- use of certain medications.
In newborns, the disease can be caused by streptococci, staphylococci, tonsillitis, etc. In rare cases, pericarditis can cause a disease such as nephritis. It is worth remembering that identifying pericarditis in children is much more difficult than in adults. Specialists use a cardiovisor to establish a more accurate diagnosis.
Pericarditis in children is treated with antibiotics and anti-inflammatory medications. When prescribing therapy, the patient's age must be taken into account. The duration of the treatment course depends on the severity of the pathology in the child.
Diagnosis of the disease
As mentioned above, the rate of fluid in the pericardium in ml should not exceed twenty units. Otherwise, we are talking about obvious pathology.
Previously, pericarditis was diagnosed only by auscultation. Currently, medicine has the ability to diagnose the disease using the following research methods:
- Ultrasound examination makes it possible to make an accurate diagnosis of effusion of pericarditis, since the splitting of the pericardial layers and the accumulation of fluid are clearly visible on the device;
- exudative pericarditis can be determined by taking a puncture and subsequent examination;
- an x-ray may show an increase in the cardiac shadow;
- effusion pericarditis can be determined using an ECG procedure.
Treatment of pathology in adults
Treatment of any type of pericarditis is accompanied by mandatory hospitalization. To avoid the onset of tamponade, the patient needs constant supervision of medical workers. Therapy is prescribed according to the type and severity of the disease. The patient is discharged only when LDH and pericardial effusion fluid are normal.
Surgical interventions are used quite rarely, only in extreme cases when the patient’s life is in danger. Basically, conservative treatment is carried out for fluid in the pericardium of the heart, the causes of which must be identified in advance.
The most popular drugs are:
- anti-inflammatory non-steroidal drugs together with gastroprotectors (for example, Ibuprofen, Indomethacin);
- drugs for arrhythmia;
- antibiotics that suppress the infectious agent;
- indirect anticoagulants, which help prevent the formation of blood clots;
- glucocorticosteroids.
Surgery involves opening the pericardial cavity and pumping out the fluid. Laser surgery has been successfully used and has been showing positive results for a long time. After this type of intervention, the amount of fluid in the pericardium decreases to normal.
If achieving the desired effect using the methods described above is impossible for some reason, cardiac intervention is used, in which the cardiac membrane is removed.
Hydropericardium: causes, signs, diagnosis, treatment
Causes
An increase in the volume of transudate in the pericardium is often provoked by edematous syndrome, which can be observed with:
- congenital diverticulum of the left ventricle;
- heart failure;
- kidney pathologies;
- stagnation;
- with direct communication between the peritoneal and pericardial cavities;
- inflammatory diseases;
- allergic reactions;
- injuries;
- anemia;
- exhaustion;
- anorexia.
In more rare cases, hydropericardium is provoked by tumors of the mediastinum, myxedema, taking vasodilators or radiotherapy. Hydropericardium can also be observed in pregnant women or in the elderly (in isolated form).
The types of hydropericardium are:
Signs
When a large amount of fluid accumulates in the pericardium, the patient develops signs of cardiac dysfunction, which are caused by compression of the heart and difficulty in its functioning:
- constant shortness of breath;
- discomfort in the chest (when bending forward);
- chest pain;
- attacks of suffocation;
- swelling of the lower extremities;
- puffiness of the face and hands;
- decrease in systolic pressure;
- increased heart rate;
- increased venous pressure.
When listening to heart sounds, their weakness and deafness are noted. In the area of the jugular veins, they are depressed and overflowing.
If the pericardial cavity is significantly overfilled, cardiac tamponade may develop, that is, its chambers cannot relax normally and pump the required volume of blood. The patient develops acute heart failure:
Without immediate medical attention, cardiac tamponade can lead to acute heart failure, shock, cardiac arrest, and death.
Hydropericardium in the fetus
To prevent this congenital malformation of the heart of the unborn child, a pregnant woman needs constant monitoring by a doctor and fetal cardiography. In some cases, spontaneous disappearance of fluid from the pericardial cavity is possible, but more often it is necessary to perform pericardiocentesis (pericardial puncture) in the fetus. This manipulation is difficult to perform and is performed under ultrasound control, since it is accompanied by a high risk of injury to the fetus and the expectant mother.
Diagnostics
To identify hydropericardium, the doctor needs to collect a medical history and conduct a series of diagnostic examinations:
- Echo-CG;
- chest x-ray;
- clinical urine and blood tests;
- blood chemistry.
A quantitative assessment of the volume of transudate is also carried out:
- minor – up to 100 ml;
- moderate – up to 500 ml;
- large – more than 500 ml.
When the pericardial layers are separated by more than 20 mm, the patient must undergo a pericardial puncture under the control of Echo-CG or radiography. The transudate shows signs of its difference from exudate:
- relative density – less than 1.016;
- protein level is less than 1-3%.
Microbiological and cytological laboratory tests of the transudate obtained during pericardial puncture are also carried out.
With a small amount of fluid in the pericardial sac, patients are not bothered by any symptoms, and such hydropericardium does not require special therapy and goes away on its own. In such situations, it is necessary to identify the cause of a significant accumulation of transudate and eliminate it.
https://doctor-cardiologist.ru/gidroperikard-prichiny-priznaki-diagnostika-lechenie
Prevention and rehabilitation
Prevention of pericarditis consists mainly of preventing diseases that can cause an increase in the amount of fluid in the pericardium.
In cases where pericarditis has already manifested itself, the patient is limited in physical activity. After completing a course of treatment, a course of rehabilitation is necessary, which is preferably carried out in sanatoriums under the supervision of specialists. If the patient does not have such an opportunity, it is worth paying attention to special training and selection of a suitable place of work that does not involve heavy physical labor.
Patients who have had pericarditis may be assigned a disability group. It is determined by doctors according to the severity of the person’s disease.
Treatment
On an emergency basis. Its essence lies in puncture of the cavity of the pericardial sac and drainage of the anatomical structure. This is the main help and at the same time a symptomatic measure.
But no one can guarantee the absence of relapse and further well-being. Therefore, further examination is indicated, identifying the cause, and then eliminating it using medicinal or surgical methods.
Defects such as ventricular septal defects and others require radical intervention. Valve replacement or valve replacement is indicated. Other situations can be corrected with medications if possible.
As part of maintenance therapy after puncture, the following is prescribed:
- Antihypertensive. If your blood pressure is high. Critically low levels are normalized only in the first moments; Atropine or Epinephrine (adrenaline) is used in an adequate dose.
- Arrhythmias such as extrasystole and ventricular fibrillation are corrected with Amiodarone. Tachycardia is eliminated with beta blockers, such as Anaprilin in a single dosage of a maximum of 50 mg.
- Restoring metabolic processes requires taking Mildronate.
Further methods are determined by specialists. One cardiologist is often not enough. High-quality comprehensive care can only be obtained in a hospital.