Pericarditis in children is quite rare, but it can cause serious consequences, which means you need to be prepared to recognize the disease in a timely manner.
The risk of developing pathology exists even in newborns, and there are various reasons for this. Preventive measures can prevent the occurrence of this dangerous pathology, and the task of parents is to provide them.
Why do children develop pericarditis?
Pericarditis is an inflammatory lesion of the outer lining of the heart , which leads to pathological disorders. The development of pericarditis is associated with 2 mechanisms - the accumulation of a significant amount of exudative fluid in the pericardial cavity and a change in the structure of the membrane tissue (thickening or fusion of leaves).
Excessive pressure appears on the heart, and the possibility of its expansion during contraction is limited. As a result, serious disturbances appear in the circulatory system.
Most often, the inflammatory process has an infectious etiology. In childhood, the most common pathogens are viruses (influenza, adenoviruses, Coxsackie), but bacteria (staphylococci, streptococci, meningococci, tubercle bacilli) and fungi (candida, actinomycetes, toxoplasma) are also isolated.
The etiology of childhood pericarditis can also be aseptic in nature . In this case, the following causes are identified: allergic reactions, juvenile rheumatoid arthritis, congenital heart defects, renal pathologies and uremia, blood diseases, autoimmune disorders, chest injuries, taking certain medications (antibiotics, vaccines, serums), systemic diseases, sugar diabetes, polyserositis, toxic or radiation exposure.
Causes
The causes of pericarditis have not been sufficiently studied to date. According to the etiology, the disease can be of an infectious nature (tuberculous, viral, fungal) or non-infectious (aseptic pericarditis). Aseptic include:
- Uremic;
- Rheumatoid;
- Autoimmune;
- Allergic;
- Post-infarction;
- Pericarditis as a result of radiation exposure, etc.
If the nature of the disease is not determined, the patient is diagnosed with “idiopathic pericarditis.” Most scientists are confident that the causes of idiopathic pericarditis are viral.
Pathogens of infectious origin can be:
- Coxsackie viruses groups A and B;
- Influenza virus;
- ECHO viruses;
- Parotitis;
- Herpes simplex;
- Fungus;
- Various bacteria.
The problem of the etiology of this disease is described in the work of A.A. Gerke, where the object of study was clinical and sectional material. According to scientific research, the causes of inflammation of the pericardium are as follows:
- Rheumatism;
- Pneumococcal diseases;
- Strepto- and staphylococcal diseases;
- Tuberculosis bacillus;
- Injury.
In medical practice, metabolic causes of pericardial disease are also identified, such as gout, Dresler syndrome, thyrotoxicosis and others.
Common forms of the disease
According to the nature of the inflammatory process in children, the following forms of pericarditis differ:
- Exudative or exudative type. It usually develops as a result of an infectious lesion, and therefore accounts for more than 80 percent of childhood pericarditis.
A characteristic feature of the pathology is the gradual accumulation of exudate in the cavity.This variety is very dangerous for a child, because... leads to compression of the organ and disruption of blood flow. Failure to take action may result in death.
- Dry or fibrinous type. In contrast to the previous option, the pericardium dries out excessively, and fibrin (a thread-like protein) accumulates on the surface of the membrane in the form of villi. As a result, the shock-absorbing capabilities of the shell deteriorate and, accordingly, obstacles arise for normal heart contractions.
- Adhesive or adhesive type. It manifests itself in the form of thickening of the pericardial layers and their fusion with each other. The result is compression of the heart and organ dysfunction. A dangerous type is constrictive pericarditis, when thickened layers compress the atria and ventricles, impairing blood circulation.
- Purulent pericarditis. This is a dangerous infectious species caused by pathogenic bacteria. Purulent exudate accumulates in the cavity, which complicates the course of the disease.
- Tuberculosis type. It is excited by the tuberculosis bacillus and is typical for children with tuberculosis. However, it can also be detected in children whose tuberculosis tests are negative. This form of pericarditis is very dangerous and requires effective measures.
Based on the nature of the disease and the manifestation of symptoms, the following options are distinguished:
- acute has a characteristic sharp manifestation with pronounced symptoms for up to 7 days;
- subacute – develops over 3 months;
- chronic is diagnosed when the disease lasts more than 6 months.
Medical statistics indicate some features of childhood pericarditis. Until the age of 6, pathology is detected only in an acute form, and a purulent manifestation is often recorded.
Newborns are most often infected in the first days of life, in the maternity hospital. In infants, up to 90% of the pathologies under consideration are provoked by staphylococci and streptococci. Next, priority goes to viral pathogens.
After 6-7 years of age, the course of pericarditis in children is practically no different from that of adults . In etiology, acute respiratory viral infections and acute respiratory infections are especially distinguished. According to statistics, 15-22% of adolescents with pericarditis have the rheumatoid variety. In general, pericarditis occurs in 1 to 1.5 percent of children under 16 years of age.
Diagnostic methods
To identify pericarditis, they are guided by the patient’s complaints and examination data, and research data are used to confirm the diagnosis:
- There are signs of inflammation in the blood - an increased content of leukocytes, a high ESR, a shift in the leukocyte formula to the left.
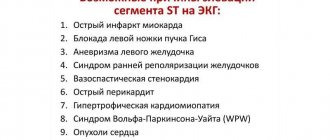
- ECG - the amplitude of the ventricular complex is reduced, the P and T waves can change polarity. In the acute stage, ST rises, then decreases to normal.
- PCG – murmur throughout the entire cardiac cycle, periodic clicks. Accent of 2 tones over the pulmonary artery.
- X-ray – the heart is in the form of a ball with exudative pericarditis; with the adhesive process, the superior vena cava is wide, the contour of the cardiac shadow is unclear, there are adhesions with the pleura.
- EchoCG is the main method for determining the amount of fluid in the cavity of the pericardial sac, disturbances in ventricular contraction, adhesions between the layers of the pericardium and with the pleura, and thickening of the outer lining of the heart.
- CT and MRI detect changes in the thickness of the pericardial layers.
Symptoms and signs
The manifestation of pericarditis in children depends on the type of pathology, its etiology and stage of development.
Quite often the disease is asymptomatic, which makes diagnosis difficult. The most pronounced symptoms of the disease are in the acute form. The following symptoms can be identified that are common to all types : pain in the chest area, frequent malaise and weakness, shortness of breath, tachycardia, non-productive (dry) cough, swelling of the lower extremities, increased size of the jugular vein, arterial hypotension, blue discoloration on the lips and ears, increased temperature bodies.
It is necessary to highlight some specific signs:
- Dry pericarditis in acute form. The onset is marked by pain and fever. The pain in children is concentrated in the navel area, and in adolescents - in the heart area with irradiation to the left shoulder. They intensify with deep inspiration. Parents may notice a reaction in babies such as crying and fussing.
- Exudative pericarditis in acute form . Constant dull pain occurs, which is why the child tries to take a “half-sitting” position with his head tilted forward. Characteristic additional symptoms are hiccups, wheezing, vomiting, and pain in the liver area. The progression of the disease causes an increase in intracranial pressure in children with swelling of the large fontanel.
- Constrictive pericarditis . Particularly noticeable is the swelling and pulsation of the neck veins. There is an unpleasant sensation in the hypochondrium on the right, the face swells. The development of the process leads to an enlargement of the liver.
The chronic form of the disease in adolescents is characterized by constant unpleasant sensations (periodically turning into pain) in the heart area. They intensify with physical activity. Quite often, slight cyanosis of the nail plates and ears appears.
Prognosis, complications
The prognosis for pericarditis is favorable if the disease is detected early and its treatment is started. Usually there is a complete restoration of working capacity or a slight loss of it. If the inflammation is purulent, the prognosis is unfavorable.
If a large volume of exudate accumulates during pericarditis, it begins to compress the heart. This is fraught with the development of tamponade. In this case, adequate heart contractions are impossible, so the child’s condition worsens sharply. If medical assistance is not provided in a timely manner, the outcome can be fatal.
One of the possible complications is myopericarditis. In addition to the pericardium, inflammation in this case affects the heart and myocardium.
A common complication of pericarditis is mediastino-pericarditis. In this case, not only the pericardium is inflamed, but also the mediastinal tissue. This disease often occurs against the background of oncology, infectious lesions of the respiratory tract and lungs, fungal infection, tuberculosis, allergic reaction, HIV.
After pericarditis, long-term cardiac conduction disturbances are possible. Because of this, attacks of arrhythmia periodically occur. With frequent episodes of this phenomenon, disability is possible.
With purulent pericarditis, the formation of fistulas is possible - this complication rarely occurs. Due to the destruction of tissue by pyogenic microorganisms, holes are formed, connecting two natural cavities of the body - the heart sac and the esophagus or pleural cavity. Treatment can only be surgical.
Course of the pathology
The onset of the disease is associated with infection in the pericardial cavity. Next, a toxic effect on tissue cells develops or an immune-mediated effect occurs. It is possible to combine these mechanisms.
Pathogenesis can be caused by contact inflammation, i.e. spread of the process from nearby organs. The aseptic reaction is caused by the action of toxicants.
The disease in children usually begins acutely. When the cardiac cavities are compressed, hypodiastole develops, which leads to stagnation of blood in the vena cava, hepatomegaly and edema.
Pain syndrome appears almost from the very beginning , and in children under 4-5 years of age it is felt in the navel area and is accompanied by active gas formation in the intestines.
The intensity of symptoms is largely determined by the accumulation of fluid (effusion) in the cavity. This phenomenon is evidenced by an increase in the area of cardiac dullness. Compression of the heart chambers disrupts their diastolic filling. With adhesive pericarditis in a child, the acute phase can be smoothed out, and pronounced symptoms appear only at the hypodiastole stage.
In infants (up to 1 year), intracranial pressure increases significantly with the manifestation of signs of neuralgia similar to meningitis.
At what age is it most common and how is it diagnosed?
Pericarditis can affect a child at any age. If up to 6-7 years only an acute form is possible, then after this age the disease can acquire chronic forms. The doctor makes a preliminary diagnosis after examination, palpation, percussion and auscultation of the child .
Upon examination, smoothness of the intercostal zone is revealed. In infants, the chest may protrude on the left side. There is no active phase of respiratory movement in the epigastric zone. An abnormal pulse with weak filling during inspiration, dullness of heart sounds, and expansion of the boundaries of the organ are detected.
The diagnosis is confirmed by conducting the following studies:
- General and biochemical blood tests to confirm the presence of an inflammatory process and determine its nature.
- ECG. The change in the amplitude and width of the teeth and the ST segment is established.
- Echocardiography reveals fluid accumulation and the appearance of fibrin.
- Radiography clarifies changes in organ size and reveals atelectatic foci.
- MRI and computed tomography provide complete information about the pathology.
In some cases, there is a need to use invasive diagnostic methods. Pericardial puncture (pericardiocentesis) is performed when there is a high risk of severe complications and surgical intervention is planned. We talked in more detail about the diagnosis of pericarditis in another article.
Diet
Cranberry juice will help replenish the fluid deficiency in the body of a child with pericarditis and saturate it with vitamins.
In case of an acute process or exacerbation of chronic pericarditis, it is recommended to provide the child with a complete, fortified diet. Products should replenish the child’s body with potassium, magnesium, selenium, fatty acids, and amino acids.
The diet will speed up the restoration of damaged tissues and recovery. The volume of fluid consumed and detailed recommendations on diet will be given by a cardiologist in each specific case. However, there are general recommendations:
- meals are fractional, 5-6 rubles. in a day;
- It is better to prepare dishes by boiling, stewing or steaming;
- Food should be prepared without salt, add salt to the plate, limiting the amount of salt to 5-6 g per day;
- The body should be provided with liquid in the form of fruit drinks (especially from cranberries, currants), freshly squeezed juices, compotes, rosehip decoction, herbal teas (in the absence of allergies, and agreeing with the doctor on a set of herbs, since tonic herbs are contraindicated).
The child should receive lean meat, fish, cereal porridge, lactic acid products, fruits (fresh, dried fruits), vegetables, and eggs (soft-boiled or scrambled eggs).
There are also foods that a child should not eat:
- strong broths;
- fried foods;
- legumes;
- baked goods;
- mushrooms;
- seasonings and sauces;
- canned food (including homemade);
- caviar, salted and smoked fish;
- coffee and strong tea;
- chocolate and cocoa.
The following products will provide the necessary vitamins:
- vitamin C, necessary for strengthening the vascular wall and the body’s immune defense, preventing blood clots, is found in sea buckthorn, citrus fruits, black currants, and rose hips;
- vitamin A, which helps normalize cholesterol and muscle contractility, is found in pumpkin, carrots, and milk;
- vitamin E, which prevents blood clots and provides protection to red blood cells that supply the heart with oxygen, is found in meat, cereals, fresh vegetables, and olive oil;
- vitamin PP, which strengthens capillaries, is found in black currants, chokeberries, and citrus fruits;
- Cereals, eggs, milk, and meat are rich in B vitamins necessary to prevent arrhythmia.
It is advisable to avoid eating foods that cause bloating.
Clinical guidelines
To unify approaches to the diagnosis and treatment of children's pericarditis, the Ministry of Health of the Russian Federation has developed Federal clinical recommendations for the provision of medical care to children with pericarditis. They were approved by the Congress of Pediatricians on 02/14/15. Treatment priorities are based on the grades of recommendations and levels of evidence based on decisions of the European Society of Cardiology.
Federal clinical guidelines for the provision of medical care to children with pericarditis can be downloaded here.
Treatment and prognosis
The main difference in the tactics of treating pericarditis in children from the treatment of adults is mandatory hospitalization, the use of invasive methods only in extreme, especially severe cases, the prescription of drugs taking into account age restrictions and strict control of the treatment process and the development of the disease.
Conservative methods include the establishment of a special regime and diet, etiotropic, anti-inflammatory and symptomatic therapy .
Basic therapy is aimed at eliminating the inflammatory response. The drugs prescribed are Ibuprofen, Aspirin, Diclofenac, Indomethacin. At the same time, the root cause of the disease is affected. Most often, antibiotics are prescribed (Penicillin, Ampicillin, Amoxicillin).
For rheumatoid pericarditis, glucocorticoids (Prednisolone) are used. If a pathology of the tuberculosis type is detected, then an injection of Streptomycytin is performed.
Long-term active therapy requires gastroprotection, for which antacids and proton pump inhibitors are prescribed. Colchicine is used to eliminate the risk of relapse.
The prognosis for the recovery of children with timely initiation of treatment is favorable . The greatest concern is advanced adhesive or constrictive pericarditis and especially the complication of cardiac tamponade.
With a mild course of the disease, symptoms can persist for 14-16 days, and the effusion is removed in 9-12 days without complications.
Purulent processes are especially dangerous for infants. In this case, there is a risk of death, and the probability of chronicity of the process is estimated at 15-18%.
Possible consequences
Pericarditis in children is dangerous due to its complications. The progression of exudative type pathology with excessive accumulation of effusion can cause cardiac tamponade . Severe cardiac dysfunction appears, venous and intracranial pressure increases.
Tamponade is characterized by swelling of the face and neck, acrocyanosis, cold sweating, and severe shortness of breath. If the fluid is not removed immediately, it can be fatal.
In the case of adhesive type pericarditis, the development of the process inevitably leads to heart failure , which is a clear threat to life. Liver damage should be considered as a late complication. There are signs of false cirrhosis.
In some cases, the disease is asymptomatic and therefore cannot be detected in a timely manner. Despite the absence of external manifestations, structural changes occur that are irreversible. The pathology gradually becomes chronic.
With age, under the influence of a number of factors, this process can significantly worsen the quality of life. A person cannot be exposed to significant physical activity and may partially lose working capacity. This leads to disability of the patient.