What is a microreaction blood test?
8 minutes Author: Lyubov Dobretsova 1012
Syphilis is considered one of the most common diseases that are transmitted primarily through sexual contact. Every year, this disease affects millions of people around the globe, but accurate statistics regarding the number of cases are not kept.
Fortunately, modern medicine makes it possible to quite successfully combat syphilis in the early stages of its development, in particular, thanks to special diagnostic procedures. A place of honor among these is occupied by an analysis in which blood is donated for microreactions. It is called microprecipitation, microreaction to syphilis, and also abbreviated as MRP or MR.
Tell me, what does MRS analysis mean?
MRS, and MR magnetic resonance.
Magnetic resonance imaging (MRI) is one of the modern methods of radiation diagnostics, which allows non-invasively obtaining images of the internal structures of the human body. The most important advantage of MRI compared to other methods of radiation diagnostics is the absence of ionizing radiation and, as a consequence, the effects of carcinogenesis and mutagenesis, the risk of which is associated (albeit to a very small extent) with exposure to X-ray radiation.
Read more about microreactions to syphilis
It is worth noting that a hematological study is aimed at identifying not the causative agent of syphilis itself (i.e., Treponema pallidum), but at the body’s specific immune response to the presence of a harmful bacterium. Thus, treponema penetrates inside through small wounds on the mucous membranes covering the genitals from the inside, then begins to actively multiply, causing significant damage to human health.
Trying to protect itself from a dangerous guest, the body immediately produces antibodies - protein defense complexes that attack microscopic ill-wishers and restrain their further growth. The amount of antibodies is proportional to the number of syphilis pathogens.
A blood test for a microreaction registers antibodies linked to dangerous antigens, but not Treponema pallidum, so there is a low probability of obtaining a false result due to a similar protective reaction of the body to other forms of diseases that have nothing to do with syphilis.
As a rule, the bacterium is introduced through the genital tract, but in some cases, damage to the mucous membrane of the rectum or oral cavity can serve as a unique gateway for it. This phenomenon is mainly associated with non-traditional types of intimacy. The causative agents of syphilis are contained in the biological fluids of an infected person.
That is, the disease can be transmitted to healthy people through blood, saliva, vaginal secretions or semen. Therefore, a household route of transmission of treponema is likely. To test for syphilis, in many cases blood is required from a capillary, but sometimes it is taken from a vein. Quite rarely, cerebrospinal fluid (cerebrospinal fluid) appears as the material being studied.
Antibody analysis in the diagnosis of TORCH infections
The abbreviation TORCH appeared in the 70s of the last century, and consists of capital letters of the Latin names of a group of infections, the distinctive feature of which is that, while relatively safe for children and adults, TORCH infections during pregnancy pose an extreme danger.
The blood test for TORCH infection is a comprehensive study, it includes 8 tests:
— Determination of antibodies to herpes simplex virus type 1,2 IgM and IgG
— Determination of antibodies to cytomegalovirus IgM and IgG
— Determination of antibodies to the rubella virus IgM and IgG
— Determination of antibodies to Toxoplasma gondii IgM and IgG
Often, infection of a woman with TORCH complex infections during pregnancy (the presence of only IgM antibodies in the blood) is an indication for termination.
Types of analysis
In medical laboratories, syphilis is detected in three ways. Briefly about each:
- Microscopy. The antibodies produced by the body are quantified using a modern light microscope. No dyes are used.
- Macroscopy (Hoffmann reaction). After centrifugation, a little antigen with charcoal particles is added to the serum or plasma. If the patient's biological fluid contains antibodies produced as a result of the development of syphilis, then when interacting with the VDRL antigen they are converted into flakes. Thanks to coal, the sediment is colored and then examined visually by specialists without the use of additional medical devices.
- Quantification. The blood sample is diluted several times in a row with special reagents, and each new portion obtained is examined for the presence of sediment, which consists of antibodies linked to foreign antigens.
When identifying syphilis, doctors give preference mainly to the first two types of research. It must be remembered that this type of diagnosis as a general blood test is considered practically uninformative when trying to detect the causative agents of syphilis.
Types of analysis
Microreaction refers to non-specific (non-treponemal) research methods, because it does not reveal the pathogen, but cell damage. Their destruction can occur with other pathologies in the body. If the test result is positive, specific serological tests are prescribed, such as ELISA (enzyme-linked immunosorbent assay), RPHA (direct hemagglutination reaction), RIF (immunofluorescence reaction). They make it possible to directly detect the content of the syphilis pathogen.
Performing the test using a high-resolution microscope
There are several types of precipitation microreactions.
- Macroscopy test (rapid diagnosis of syphilis). Detection of a complex of antigens and antibodies is carried out without the use of equipment. For visualization with the naked eye, a chemical is added to the blood serum that combines with the complex. Use coal particles or red pigment.
- Microscopy test. To detect lipid antibodies, a light microscope is used, which eliminates the need for additional substances.
- Test with a quantitative indicator. It is carried out under conditions of repeated dilution of the test material and identification of the number of complexes in each portion. The titer is the last dilution in which the antigen-antibody combination is determined.
The microreaction of precipitation got its name due to the small amount of the material being studied and the precipitation of complexes (precipitation) in the form of small flakes.
Indications for blood tests
Hematological testing for STDs should be urgently performed in patients with symptoms of syphilis. The most common warning signs are:
- painless chancre in the form of large, hard pimples with white heads or open sores;
- papules (multiple nodules on the skin);
- rashes of a crimson or pinkish hue (often they cover the feet and palms);
- swollen lymph nodes;
- grayish coating on the tongue;
- active hair loss on the head and the appearance of bald spots;
- retraction of the nasal bridge;
- nose bleed;
- gummas (painful dense formations with smooth pale pink edges and purple, dark brown depressions in the form of craters);
- perforation of the palate (formation of holes);
- acute body weight deficiency;
- aching joints and bones in the evening and at night;
- sensory disturbance;
- basal meningitis;
- meningomyelitis (inflammatory damage to the membranes of the spinal cord, its roots and substance);
- hydrocephalus;
- Bayle's disease (paralytic dementia);
- hallucinations.
All symptoms are arranged as syphilis develops from the first to the terminal stage. At the initial stage of this disease, poor appetite, muscle weakness, fever, insomnia and headaches sometimes make themselves felt.
During syphilis, women may suffer from burning and unpleasant pain in the genital area, and vaginal discharge takes on a strong, specific odor. Herpes appears. The chancre, which was discussed earlier, is observed mainly on the penis in men and on the labia in women, with further growth of ulcers to the pubis, thighs and abdominal cavity.
A laboratory test for syphilis is required:
- babies born to women who have been diagnosed with syphilis;
- people suffering from any other sexually transmitted diseases;
- persons living with sick relatives;
- patients to confirm the results of previous screening for syphilis.
- citizens who have had intimate relationships with unverified partners or those who suffer from STDs.
Blood testing for syphilis must be done during:
- bearing a child;
- preparation for IVF (artificial insemination) or surgery;
- inpatient treatment;
- examinations of prisoners in colonies, pre-trial detention centers and prisons.
Every year, during a routine examination, specialists prescribe such a blood test to healthcare workers, military personnel, the educational sector, medicine and public catering. If patients suffering from syphilis already adhere to the treatment developed by doctors, then microreaction analysis is carried out regularly in order to monitor the effectiveness of the chosen course of therapy.
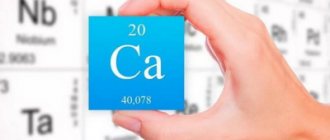
Analysis for potassium and magnesium: deciphering the main indicators
When assessing the results of tests for basic microelements (sodium, calcium, potassium and magnesium, chlorine, phosphorus, iron), possible reasons for a decrease or increase in their levels are taken into account. If necessary, patients are prescribed additional examination to clarify the diagnosis.
| Name and designation in the analysis | Reasons for the decline | Reasons for the increase |
| Potassium, K+ | Lack of nutrition (little greens, vegetables, fruits), blood loss, surgery, injury, childbirth, increased thyroid function, hormone treatment, overdose of insulin, diuretics, loss with vomiting, diarrhea, sweat, pancreatic tumor, adrenal gland disease, kidney disease | Administration of potassium (drips, tablets), breakdown of red blood cells, cancerous tumors, destruction of muscle tissue, burns, viral infection, blood acidification, renal failure, shock, blood flow disorders (tissue ischemia), taking potassium-sparing diuretics, blood pressure medications (ACE inhibitors) |
| Magnesium, Mg+ | Fasting, strict diets, diseases of the intestines, adrenal glands, kidneys, vomiting, diarrhea, infection with worms, tumors, diabetes, taking diuretics, antitumor drugs, excess parathyroid or thyroid hormones, lack of vitamin D, inflammation of the pancreas, alcoholism, toxicosis during pregnancy, long-term lactation | Administration of drugs with magnesium, including to reduce the acidity of gastric juice, decreased function of the thyroid gland, kidneys, adrenal glands, dehydration |
| Sodium, Na+ | Salt-free diet, diarrhea, vomiting, sweating, kidney, adrenal, thyroid failure, taking medications: diuretics, excess infusion solutions, diabetes insipidus, liver cirrhosis | Fluid loss (sweating, vomiting, diarrhea, severe shortness of breath), lack of water intake, increased adrenal function, hormone use |
| Chlorine, Cl- | Sweating, vomiting, diarrhea, kidney failure, overdose of diuretics, laxatives, blood acidification | Dehydration in diabetes mellitus and diabetes insipidus, increased synthesis of cortisol by the adrenal glands or treatment with its analogues (for example, hydrocortisone) |
| Calcium, Ca+ | Decreased function of the thyroid and parathyroid glands, vitamin D deficiency, severe kidney and liver diseases, acute inflammation of the pancreas, treatment with antitumor and anticonvulsants, blood transfusions | Increased formation of parathyroid hormones, thyroid glands, tumors of bones, breast, lungs, kidneys, ovaries, uterus, blood, bed rest for injuries, overdose of vitamin D, diuretics, decreased adrenal function, hereditary diseases with impaired calcium metabolism |
| Phosphorus, P- | Rickets, softening of bones, malabsorption in the intestines, diarrhea, vomiting, gout, insulin overdose, pregnancy, decreased growth hormone levels | Treatment with anticancer drugs, vitamin D overdose, parathyroid gland failure, kidney failure, bone tumors and their metastases, leukemia, decreased bone density, diabetes mellitus with ketoacidosis, liver cirrhosis |
| Iron, Fe+ | Iron deficiency anemia, acute and exacerbation of chronic infections, tumors, including blood, autoimmune diseases, blood poisoning, blood loss, vegan and vegetarian diet, pregnancy, lactation, adolescence, decreased thyroid function, liver disease, Aspirin use , hormones | Treatment with iron supplements, administration of blood, red blood cells, anemia with destruction of red blood cells, decreased formation of blood cells in the bone marrow, deficiency of B12, folic acid, kidney and liver disease, lead poisoning, use of contraceptives, antitumor |
Blood for bladder cancer: what is it and when is the test prescribed?
There is a whole category of diseases that affect most areas of any person’s life, and even intimate ones. Doctors call one of the diseases of this type syphilis. It is worth noting that the disease is quite ancient and was known in ancient times. To diagnose this disease, a blood test is performed for bladder cancer.
Thanks to this test, which can be done in almost any clinic today, it is easy to detect syphilis and accurately diagnose it at the very beginning of the development of the disease.
After the main culprit of the disease, treponema pallidum, became known, it became easier to make a diagnosis such as syphilis, despite the fact that usually the main signs of the disease appeared only at the secondary stage, and the disease was already actively developing in the patient’s body. From the moment of infection to the appearance of a small ulcer located on the genitals, in practice it takes about 3 weeks. This process can take up to 3 months.
During this period of time, almost no one can notice a small and fairly quickly passing nodule, which, in principle, does not cause absolutely any inconvenience. After a couple of months, a terrible rash usually begins to appear, followed by a fever, which in most cases occurs with an increase in the size of the lymph nodes. At this stage, few people come to the conclusion that the cause is syphilis.
Due to the fact that chancre is sometimes located on the oral mucosa, many people mistake it for simple stomatitis and accordingly begin the wrong treatment process while the disease actively develops further. For this reason, it is important to diagnose it at an early stage of the disease using a blood test for bladder cancer.
What does it mean to donate blood for breast cancer?
Many people, having heard about this analysis, ask the question: Blood for bladder cancer - what is it? Is it necessary to take it in case of illness? The abbreviation RMP today is deciphered as follows: microprecipitation reaction. This is a special type of analysis. Doctors do not classify it as one of those that allows one to identify the causative agent of the infection.
The main effect of the research is to determine the various antibodies produced to one of the membrane components called cardiolipin. Typically, the production of these antibodies occurs during the initial stage of the onset of the disease, when about a week has passed since the very first day of the appearance of any rashes on clean skin, which served as a bell for the detection of the disease.
When and how is a test for syphilis done?
Analysis for syphilis is one of the most popular studies in venereology. There are several different methods that have one thing in common - the general material selected for diagnosis. This is blood. It is the presence of the pathogen in the human circulatory system that is a mandatory diagnostic marker for making a diagnosis of Syphilis, since the presence of a clinical picture is not always sufficient for this. Syphilis must be differentiated from other pathologies with similar symptoms, and in addition, there are periods of imaginary well-being with a complete absence of clinical picture.
Features of the course of infection
Decoding the diagnosis without laboratory testing is sometimes difficult, since the course of the disease is characterized by periods of complete absence of its obvious manifestations. Syphilis is caused by Treponema pallidum, a gram-negative spirochete, entering the human body. This is a spiral-like microorganism. Due to its complete immunity to any aniline dyes used for staining in bacteriology, the pathogen was called treponema pallidum.
The main mechanism of transmission is sexual, but due to the ability of the spirochete outside the host body to maintain viability and virulence for about four days, contact and household transmission is also possible. During pregnancy, the pathogen is freely transmitted from mother to child, therefore, the placental barrier is not a hindrance for it.
The average incubation period is about 3 weeks. After this, the first characteristic sign of a developing sexually transmitted infection appears - chancre. These are erosions that form on the surface of the skin or mucous membranes, that is, in the place where the pathogen was introduced. The ulcer is usually small, painless, with slight serous discharge. It can last up to one and a half months on average, and then disappears. This is followed by a period of two months, which is characterized by a complete absence of symptoms. At this time, a diagnosis can only be made if tested for syphilis.
Later, symptoms appear that are called “Secondary syphilis.” This is a general intoxication with increased body temperature, weakness and characteristic rashes. They also disappear after some time, and the disease enters the so-called latent period, which is characterized by the periodic appearance of secondary symptoms of the disease, and then their complete absence.
In the absence of proper treatment, syphilitic damage to internal organs occurs, that is, the disease develops into a tertiary form of infection. Patients with this disease are dangerous to others at any stage of the infectious process, and due to the presence of stages of asymptomatic carriage of the pathogen, it can only be detected by testing for syphilis.
When analysis is required
Since this venereal pathology is the most common to date, populations are identified that are subject to mandatory examination for the presence of Treponema pallidum in the body. These include the following groups:
- Mandatory annual preventive examination of certain groups. These are surgical doctors, teachers of any educational institutions and kindergarten teachers, workers in food enterprises and the food industry.
- The analysis is mandatory for women planning a pregnancy or who are already pregnant.
- Patients with a disease of unknown etiology with rash symptoms, pain symptoms in the joints and bones, with enlarged regional lymph nodes, etc.
- When ulcerations and characteristic discharge from the genitals appear.
- Donors.
- Any patient undergoing surgical treatment.
- If a child is suspected of having a congenital syphilitic infection.
- Contact with a patient with syphilis.
Features of laboratory diagnostics
Blood as a material for finding the causative agent of Treponema pallidum in a patient is the most universal culture. It can be taken for research at any stage of the disease, even in the complete absence of symptoms. Of course, during the period of appearance of eroded surfaces, Treponema pallidum can also be found in the discharge from chancres, but a blood test is a universal research method.
The technique was called the Wasserman reaction. It is based on the formation in the body of infected individuals of special antibodies, which, when combined with antigens of the diagnosticum, form a specific reaction, inherent only to a person with syphilis. During the study, in those who are not infected with this infection, hemolysis of red blood cells occurs, that is, their destruction. If this does not happen, a positive answer is given. In addition, by the nature of the hemolytic reaction, the stage of the infectious process can be determined. For the study, venous blood is taken on an empty stomach.
What is blood for bladder cancer: preparation and interpretation of results
The procedure is usually performed quickly; after just a few hours, you can receive examination results confirming the presence of the disease or its absence.
You can often hear from patients in the clinic the question of what is blood for bladder cancer and what method of donation is provided? The doctor knows the answers to these questions; he will tell you in detail what it is and how to properly prepare for the procedure.
Speaking of the practical aspect, the procedure is absolutely no different from any blood sampling from a person. If you have to take this test, keep in mind that the procedure must be performed on an empty stomach. You can drink water in the morning, but not carbonated water, and without any additives or sweeteners. The day before the analysis, you should not drink alcoholic beverages or eat fried or spicy foods. Otherwise, the accuracy of the analysis performed will noticeably decrease.
If you take any medications on a regular basis, you must also inform your doctor about this before taking the test. Otherwise, this fact may also have a negative impact on the quality of the analysis performed. If you are used to an active lifestyle, it is better to refrain from intense exercise before donating blood for analysis. Most doctors advise trying not to be nervous.
It is really difficult to remain calm when your lifestyle depends on the results of the analysis. But if you get nervous, the situation will only get worse and you will need to donate blood again. The simplest, most affordable way to calm down right before taking tests is to drink a glass of plain water.
A sufficient amount of water in the body almost instantly helps stabilize normal health. So, a sample of his blood is taken from the patient.
Subsequently, various manipulations are carried out: the necessary antigens are added, which, in the case of a disease, simply lead to hemolysis occurring, all red blood cells are destroyed. For the patient himself, the procedure will not differ from a simple blood draw required for a general analysis.
Decoding
Having thought about what blood is for bladder cancer, first of all you need to know that the interpretation of this analysis demonstrates that the result for you can be positive or negative.
In the first case, donating blood demonstrates that the person’s body has the prerequisites for the disease. In the case of a low antibody titer, the result is a false positive.
In practice, these types of results indicate one of the following diseases:
- diabetes;
- the presence of various formations that are dangerous for the patient, of a malignant type;
- leprosy;
- presence of developing HIV infection;
- measles;
- tuberculosis;
- viral type hepatitis;
- pregnancy in exceptional cases and so on.
If, based on the results of the test, a negative result was obtained, then in this case it is possible in most cases to reliably assert the fact that the patient does not have syphilis. However, it is necessary to be careful in diagnoses, since in practice there are cases when such a result was already the first stage of the development of pathology.
In any case, this study is the initial one in diagnosing the disease and in case of a positive result, the doctor will definitely prescribe a number of additional tests to determine the presence or absence of the disease.
False result
In practice, both positive and false blood results are equally common. Most often, this situation occurs if other diseases, such as leprosy or chicken pox, have been detected in the body.
After a person takes a blood test, the transcript often shows a negative result during the incubation period or at a late stage of the disease. In conclusion, it is worth noting that as soon as the slightest suspicion of a disease such as syphilis appears, it is important to immediately contact specialists to receive an official referral to undergo the necessary tests to identify the causative agent of the disease.
Medicine offers many different drugs that will help in treating the disease. First of all, today doctors suggest turning to antibiotic therapy using several penicillins.
Since the sensitivity of spirochetes to drugs of this type is quite high, the chances of a quick recovery are high to say that it is an understatement. The only negative may lie in the importance of inpatient treatment, since it will be necessary to observe the timing of the injections, and according to the recommendations of specialists, they should be given every three hours if there are no contraindications.
Preparing for the examination
Improper preparation affects the quality and outcome of the study. Before submitting the ionogram, you must complete the following steps:
- Do not eat food 6 hours before the test.
- The day before, exclude physical activity, stress, drinking alcohol, visiting the sauna, bathhouse.
- 2-3 days before donating blood, eat as usual.
- Stop taking medications containing K, Na, Ca and other ions several days before the expected examination.
- Tell your doctor about the use of any medications - diuretics, cardiac glycosides.
- Stop smoking 1.5-2 hours before the test.
- Immediately before submitting, sit quietly for 10-15 minutes.
How is a blood test performed?
To carry out a general blood test, no special preparation is required, but shortly before the examination you should not eat fatty foods or drink alcohol. Usually the analysis is carried out in the morning, on an empty stomach or after two hours after eating. Blood is taken from a finger, collected in a special vessel and sent for examination.
After receiving the results, the doctor interprets the blood test. There are also special hematology analyzers that can automatically determine up to 24 blood parameters. These devices are capable of producing a printout with a transcript of the analysis almost immediately after blood sampling.
Methodology and evaluation of results
For the study, capillary blood is taken from a finger, venous blood from the ulnar vein on an empty stomach, or cerebrospinal fluid is obtained. The analysis is carried out on a sterile, defatted glass, into which a classic reagent (antigen), a drop of serum or plasma is placed. After thoroughly mixing the ingredients and adding coal particles, the results of the reaction are monitored under macroscopy.
Blood serum and laboratory antigen are mixed on a sterile Petri dish
- Positive reaction. It is characterized by the formation of flocs in the sediment when antibodies to lipids of destroyed cell membranes are detected. It indicates the disease with any form of syphilis, as well as the preservation of the titer in a small group of people after treatment of the disease.
- Negative reaction. It is characterized by the absence of formation of characteristic flakes; the blood does not contain specific proteins. This means that syphilis has not been detected or is at a late stage. In some cases, the examination is carried out in the early stages of the primary form of the disease, when antibodies have not yet formed or their number is negligible.
- Questionable reaction. A slight precipitation is detected, which indicates a low content of antilipid antibodies. In such cases, observation, repeated tests, and the appointment of additional examination methods are necessary.
The ability to detect immune complexes using microprecipitation reactions occurs a month after infection. As the disease progresses, the concentration of antibodies increases. With latent form and late syphilis, the titer may be low and sometimes give negative reactions.
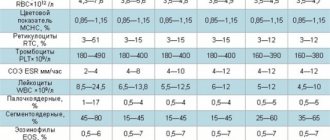
General blood test - interpretation, norms
To decipher blood test indicators, it is not enough to know their normal values. It is also necessary to have an idea of how each indicator affects the properties of blood and under the influence of what factors it can take values below or above normal. Here are descriptions of the general blood test indicators:
- Red blood cells - perform the most important function, which is to deliver oxygen to the tissues of the body and remove carbon dioxide from them. Their reduced level indicates that the body does not receive enough oxygen. When the level of red blood cells exceeds the norm, there is a high risk of blood cell sticking together (thrombosis).
- The width of the distribution of red blood cells - this indicator determines the difference in size of red blood cells. When deciphering blood test results, a high distribution width can be detected if there are both small and large red blood cells in the blood. This may indicate anisocytosis (a sign of iron deficiency or other types of anemia).
- Red blood cell volume - information about the average size of red blood cells. A low volume of red blood cells may indicate iron deficiency or microcytic anemia, and an increased volume occurs when there is a lack of folic acid or vitamin B12 in the body (megaloblastic anemia).
- The content of hemoglobin in the erythrocyte - a reduced indicator may indicate iron deficiency anemia, an increased indicator may indicate megaloblastic anemia.
- The concentration of hemoglobin in the erythrocyte - a value below normal can occur with iron deficiency anemia or thalassemia (congenital blood disease). Exceeding the norm for this indicator is observed in extremely rare cases.
- The erythrocyte sedimentation rate allows us to indirectly estimate the protein content in the blood plasma. An excess of this parameter may indicate probable inflammatory processes in the body, malignant tumors and anemia, and a decrease indicates an increased content of red blood cells (rare).
- Hemoglobin is a protein responsible for transporting oxygen to tissues and organs. Its decrease indicates anemia (oxygen starvation). An increase in hemoglobin can occur when the body is dehydrated or has a high red blood cell count.
- Hematocrit - indicates how much blood is contained in red blood cells. An increase in hematocrit may be a sign of erythrocytosis (increased red blood cell count) or dehydration. A low hematocrit can be observed with anemia or be evidence of an increase in the amount of fluid in the blood.
- Platelets - these blood cells prevent blood loss when blood vessels are damaged. An increased level of platelets, detected during a general blood test, is observed after removal of the spleen and in a number of blood diseases. If this indicator is below normal, this may indicate cirrhosis of the liver, idiopathic thrombocytopenic purpura, aplastic anemia, congenital blood diseases, etc.
- Leukocytes are responsible for protecting the body from bacteria, viruses and other infections. In the presence of infection, their levels increase. A decrease in the level of white blood cells may indicate blood diseases, and is also observed when taking a number of drugs.
- Granulocytes - the number of these cells can be increased during inflammatory processes, and a decrease in granulocytes can be a consequence of taking a number of medications, aplastic anemia and systemic lupus erythematosus.
- Monocytes are a type of white blood cell that turns into macrophages (cells whose task is to absorb bacteria and dead body cells). A high level of monocytes in the blood is observed in blood diseases, infectious diseases, and rheumatoid arthritis. A decrease in monocytes usually occurs under the influence of drugs that suppress the immune system, as well as after severe operations.
- Lymphocytes are a type of white blood cell responsible for fighting viruses and germs, as well as for developing immunity. An increased level of lymphocytes can be a sign of some blood diseases and infectious diseases; a decreased level is observed in conditions of immunodeficiency (renal failure, taking drugs that suppress the immune system, AIDS).
Each of the given indicators is important when deciphering a blood test, however, a reliable result of the study consists not only of comparing the data obtained with the norms - all quantitative characteristics are considered together, in addition, the relationship between various indicators of blood properties is taken into account.
Decoding the results
After 8-24 hours. After undergoing the analysis, the patient can receive study results that are easily deciphered. In addition to the patient’s surname, initials and date of birth, the document indicates the exact amount of immunoglobulins on the date of the study.
The IgM level normally ranges from 0.2 to 3.6 g/l with fluctuations depending on gender and health status. An immunoglobulin level of less than 0.2 g/l indicates a reduced level of antibodies.
An antibody level above 3.5 g/l indicates an increased level of the substance. The level of immunoglobulin M in the blood is affected by the patient’s age and medication use, so it is better to consult a doctor for a deciphering of the patient’s analysis for further diagnosis.
How is enzyme immunoassay performed and what does it show?
Enzyme-linked immunosorbent assay (ELISA) is a laboratory diagnostic method that allows the detection of specific antibodies and antigens in a wide variety of pathologies.
ELISA is one of the most common and accurate methods for detecting sexually transmitted infections, in particular HIV, HPV, and hepatitis B.
In order for the test results to be as reliable as possible, it is necessary to properly prepare for their delivery.
Special offers, discounts and promotions will help you save significantly on medical examinations.
Quality control of laboratory tests, carried out according to international standards, is an additional guarantee of the accuracy of test results.
Modern diagnostics in medicine is unthinkable without highly sensitive laboratory tests. Previously, to establish the causes of certain symptoms, doctors were forced to rely on indirect signs of the disease, as well as conduct multi-stage microscopic examinations in an attempt to detect the causative agent of the infection. Today, a single test—such as an enzyme-linked immunosorbent assay—is sufficient to confirm or refute the initial diagnosis.
Indicators and their standards
Norm of microelements in the blood:
| Name | Minimum level | Maximum level | ||
| Calcium | 2.05 | 2.5 | ||
| Chlorine | 96 | 111 | ||
| Potassium | 3.2 | 5.1 | ||
| Sodium | 132 | 147 | ||
| Iron | women 7.2 | Men 10.7 | women 25.9, | men 28.6 |
| Phosphorus | 0.87 | 1.34 | ||
| Magnesium | 0.67 | 1.1 | ||
When deciphering the results of the ionogram, first of all, the possible reasons for deviations from the stated standards are taken into account. If necessary, patients are prescribed additional studies to clarify the results obtained.
Basic concepts and principle of enzyme immunoassay method
Enzyme-linked immunosorbent assay (ELISA) is a laboratory diagnostic method based on the antigen-antibody reaction, which allows the identification of protein substances (including enzymes, viruses, bacterial fragments and other components of biological fluids).
To understand how an enzyme immunoassay works, let’s try to understand the essence of the “antigen-antibody” reaction. An antigen is a molecule foreign to the body, usually of protein origin, which can enter the human body along with an infectious agent. Particles of someone else's blood (if it does not match our group) are also antigens. In the body, antigens are capable of causing an immune response aimed at protecting the integrity of the internal environment from foreign substances. Therefore, our body synthesizes special substances - antibodies (immunoglobulins), capable of combining with antigens using the “key to lock” principle, linking them into an immune complex (this process is called the “antigen-antibody” reaction). Such immune complexes are more easily recognized and destroyed by immune cells.
There are several types of antibodies, each of which comes into action at a certain stage of the immune response. Thus, the first to be synthesized in response to the penetration of an antigen into the body are class M immunoglobulins (IgM). The content of these antibodies is highest in the first days of the infectious process.
Following them, the immune system releases class G immunoglobulins (IgG) into the blood, which help destroy antigens until the infection is completely defeated, and also continue to circulate through the vessels in the future, providing immunity to re-infection. Vaccination is based on this phenomenon: thanks to vaccinations containing weakened antigens of microbes and viruses, a large amount of IgG appears in our blood, which, upon contact with a real threat, quickly suppresses the infection - before it causes harm to health.
There are also class A immunoglobulins (they are found in large quantities in the mucous membranes, protecting the “approaches” to the body), E (they fight parasitic infections) and others. In laboratory diagnostics, the objects of interest most often are IgM, IgG and IgA: by their concentration, you can assess what stage the infectious process is at, and also find out whether a person has ever had a particular illness (for example, rubella or chickenpox).
How to find out which antigens or antibodies are present in the human body? When a doctor suspects that a certain infection is the cause of a disease, or wants to measure the concentration of a certain hormone, he prescribes an enzyme immunoassay for the patient.
Indications
The ionogram is shown in the following situations:
- hematopoietic disorder;
- diseases of the immune system;
- systemic pathologies of connective tissue;
- lack of vitamins and microelements in the body;
- hormonal disbalance;
- labor activity;
- kidney and liver diseases;
- major blood loss, burns regardless of degree;
- convulsions and regular loss of consciousness;
- pathologies of an infectious nature;
- long-term use of hormone-containing, antihypertensive medications and cardiac glycosides;
- hypertension and crisis;
- patients in the intensive care unit.
The results of the study will help determine the stage, intensity of the pathology and draw up a treatment regimen.
What is a false positive result and what causes it?
It is worth understanding that testing for MOP does not show the presence of the pathogenic bacterium itself in the body, but only traces of its presence. An MOP test can detect and calculate the approximate amount of antibodies in the blood serum that the immune system begins to produce in response to infection.
In some cases (no more than 5%), testing shows a false positive result, which is associated with certain human conditions. A false positive reaction can be provoked by:
- autoimmune system diseases;
- inflammatory process in the body;
- pregnancy or recent childbirth;
- infectious and viral diseases;
- dysfunction of the endocrine system.
Testing may also show a false positive result if a person has recently had syphilis but has undergone treatment. This is due to the fact that a small amount of antibodies will remain in the blood serum in any case.
Testing gives a false positive for syphilis if the patient has HIV, hepatitis or leprosy. If the doctor suspects the presence of syphilis, but the test shows a negative result, it is recommended to repeat the test in a few weeks.
How long does it take to perform an oncological blood test?
The study is prescribed if the patient exhibits pronounced signs of the development of oncological pathologies. Testing for tumor markers takes from one to ten days. Depends on the location of the tumor and the degree of its development. Thanks to the oncology analysis, the attending physician will confirm or reject the assumptions and prescribe a course of treatment according to indications.
Research is most often carried out in private medical laboratories, where the necessary equipment and instruments are available for analysis.
Norms for tumor markers
Blood for HIV infection: how many days does the test take?
In this case, it is more correct to say not how long it will take for the blood test to be ready, but how long it will take to decipher it. For private clinics - a week. The municipal medical institution will need 14 days.
AIDS research is confidential information, so the answer is provided on an individual basis. When anonymous submission is expected - without names and surnames, you can find out the results by calling the phone number left in advance or by email.
Test to determine HIV infection
For public clinics, all clinical studies, including analysis for the human immunodeficiency virus, are free. In a private establishment - payment from 300 to 9,000 rubles. The pricing policy depends on the type of research and the speed of determining the result.
What is coronary insufficiency?
Coronary insufficiency can have extremely negative consequences and even lead to death if comprehensive treatment is not started in a timely manner.
It is very important to correctly assess the severity of this pathological condition and proceed to active actions under the supervision of a cardiologist in order to correct the situation, as far as possible in a particular case. Modern treatment methods can significantly improve the condition of patients with coronary insufficiency and prevent the development of complications such as heart failure.
general information
Coronary insufficiency develops due to partial or complete blockage of blood flow in the coronary vessel, which supplies the myocardial tissue with nutrients and oxygen. The development of coronary insufficiency may have the following reasons:
- spasm;
- thrombolytic stenosis;
- atherosclerosis;
- fibrosis of vessel tissue;
- coronary artery dissection;
- tumor;
- adhesions due to compression of the vessel;
- inflammatory process;
- entry of an air bubble into the bloodstream;
- aortic aneurysm;
- anaphylactic shock;
- congenital heart defects.
Coronary insufficiency can occur in both acute and chronic forms. The acute version of the disease is characterized by a rapid increase in symptomatic manifestations. Often this variant of coronary insufficiency develops within 1-2 days. Often there is a complete blockage of the artery, as a result of which the supply of oxygen and nutrients to the myocardial tissue is stopped, which leads to the development of an ischemic process. Acute coronary insufficiency is an extremely life-threatening condition and, without urgent treatment, often leads to death.
Chronic coronary insufficiency develops due to a gradual decrease in blood flow to myocardial tissues. Often, this condition develops over 2-3 years, and only then can it begin to manifest itself with severe symptoms. The main reasons for the development of the chronic form of the disease are atherosclerosis, as well as changes in the properties of the blood, that is, its thickening.
Symptoms
Symptoms of coronary insufficiency, as a rule, begin to appear quite intensely only when the active process of myocardial death begins. That is, the first manifestations in the acute form of coronary insufficiency may appear within a few days, and in the chronic form after several years. In acute cases, sudden coronary death may occur. If ischemia increases relatively slowly, the following signs of a problem may appear:
- dyspnea;
- pale skin;
- stiffness due to physical overexertion;
- cardiopalmus;
- shallow breathing;
- nausea;
- vomit;
- burning pain in the region of the heart.
Symptomatic manifestations during the development of coronary insufficiency may initially appear only occasionally. Then angina attacks may increase. In the absence of targeted therapy, a significant deterioration of the condition is observed, which often leads to the death of the patient.
Types of analysis
Microreaction refers to non-specific (non-treponemal) research methods, because it does not reveal the pathogen, but cell damage. Their destruction can occur with other pathologies in the body. If the test result is positive, specific serological tests are prescribed, such as ELISA (enzyme-linked immunosorbent assay), RPHA (direct hemagglutination reaction), RIF (immunofluorescence reaction). They make it possible to directly detect the content of the syphilis pathogen.
Performing the test using a high-resolution microscope
There are several types of precipitation microreactions.
- Macroscopy test (rapid diagnosis of syphilis). Detection of a complex of antigens and antibodies is carried out without the use of equipment. For visualization with the naked eye, a chemical is added to the blood serum that combines with the complex. Use coal particles or red pigment.
- Microscopy test. To detect lipid antibodies, a light microscope is used, which eliminates the need for additional substances.
- Test with a quantitative indicator. It is carried out under conditions of repeated dilution of the test material and identification of the number of complexes in each portion. The titer is the last dilution in which the antigen-antibody combination is determined.
- when hospitalized in a hospital;
- prisoners in places of deprivation of liberty;
- before surgery;
- persons undergoing military service;
- during medical examinations for employees of education, medicine, and catering;
- blood or organ donors.
The microreaction of precipitation got its name due to the small amount of the material being studied and the precipitation of complexes (precipitation) in the form of small flakes.
The study is carried out to identify the causative agents of syphilis among large groups of the population. The main goal of the analysis is to carry out a screening test on a large scale for subsequent diagnosis in case of positive results.
Blood for microreaction is prescribed:
The method is widely used to monitor the effectiveness of treatment. The microreaction of precipitation is one of the reliable methods of recovery from syphilis. In addition, the quantitative test helps to adjust the dosage of drugs or replace them. It is worth noting that specific serological tests do not carry such information and give positive results after the pathogen is destroyed in the body.
Blood serum test for sugar: speed of obtaining results
The study involves establishing blood glucose levels. Blood sampling is done from a finger in the morning on an empty stomach. Some experts recommend not brushing your teeth the day before. Indeed, in this case the answer may turn out to be distorted.
Blood glucose levels
Doctors prescribe such an analysis to a patient with prerequisites for diabetes, and for people over forty years of age, the analysis is always done during a medical examination.
You can find out the results of the answer the next day.
How long does it take to perform an ORS blood test for syphilis?
To detect syphilis or to determine the Wassermann reaction, you can use two methods:
- Detection of treponema.
- Indirect signs of her presence.
Biomaterial is collected for analysis from an ulcer or infected organ. In any case, the study will show effectiveness at the first signs of the disease.
But there is a nuance here: serological analysis should be carried out 8-9 days after infection. There is no point in doing this immediately after intercourse.
Dark-field microscopy is a quick and reliable way to find out whether a person has syphilis or not. The result is known within a day. But during severe inflammatory processes, with bleeding (bleeding) and an external treatment course, it is unrealistic to find treponema.
Methodology and evaluation of results
For the study, capillary blood is taken from a finger, venous blood from the ulnar vein on an empty stomach, or cerebrospinal fluid is obtained. The analysis is carried out on a sterile, defatted glass, into which a classic reagent (antigen), a drop of serum or plasma is placed. After thoroughly mixing the ingredients and adding coal particles, the results of the reaction are monitored under macroscopy.
Blood serum and laboratory antigen are mixed on a sterile Petri dish
The ability to detect immune complexes using microprecipitation reactions occurs a month after infection. As the disease progresses, the concentration of antibodies increases. With latent form and late syphilis, the titer may be low and sometimes give negative reactions.
What to do if you test positive for MOR
If testing shows a positive or strongly positive antibody reaction to Treponema pallidum, the patient is prescribed repeated testing to confirm the diagnosis. It is recommended that tests be carried out in different laboratories, which will help eliminate errors and false positive results.
After submitting the biomaterial, while the results are being prepared, the patient must contact the treating venereologist, who will draw up a suitable treatment regimen. If the presumptive diagnosis is confirmed, the patient will be prescribed complex therapy.