Blood type is the genetic identifier of the human body. It is laid at the moment of fetal formation and does not change throughout life. Liquid tissue is classified according to the ABO system and Rh status (Rh). The most common group on the planet is the first. It is easier for its owners to help when the need for a transfusion arises. The other three 3 are less common. There is a table of the distribution of blood types by country, which also shows what the most common group is among Russian residents.
Systematization according to AB0
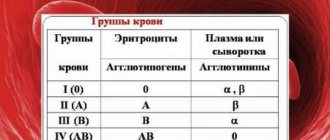
Antigen-antibody classification (agglutinogen-agglutinin) is the most common way to classify types of biofluids. It was invented by Jan Jansky, who proposed the following grouping principle:
| Common Designation | Jansky designation | Agglutinogen in erythrocytes | Agglutinin in plasma/serum |
| 0 | I | No | a and b |
| A | II | A | b |
| B | III | B | a |
| AB | IV | AB | No |
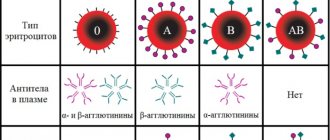
Agglutinogens are two types of antigens located on the membrane of red blood cells. They are encoded by genes A (antigen A), B (antigen B) and O (its absence).
Agglutinins are antibodies found in plasma in the form of immunoglobulins, i.e. components of immunity. In newborns they are not detected, because their immunity is not mature enough. But as the child grows and develops, they accumulate, reaching the norm by the time of puberty.
Interesting! A group is not a single indicator. The second most important is Rh status. It can be positive or negative.
If the antigen binds to agglutinin, agglutination occurs - the red blood cells settle. This occurs when A interacts with a or B interacts with b. That is why it is important to observe the same name of biological fluid when transfusing.
Rh factor
Today in the world the most common groups in humans are represented by the first (designated 0(I)), second (A(II)), third (B(III)) and fourth (AB(IV)).
Scientific research suggests several new groups that are not yet designated and are extremely rare. The separation occurs according to the criterion of the presence on the surface of erythrocytes (red blood cells) of special molecules - hemagglutinogens A and B.
It is also necessary to know about agglutinins - they are already contained in the blood plasma (there are hemagglutinins ά and β).
Accordingly, the following combinations exist:
- in the absence of hemagglutinogens on the surface of erythrocytes and the presence of both hemagglutinins in the serum, the group will be the first - 0 (I);
- the presence of only agglutinogen A and agglutinin β corresponds to the second - A(II);
- the presence of only agglutinogen B and agglutinin ά allows blood to be classified into the third group - B (III);
- if both agglutinogens and no agglutinins are found on the surface of the erythrocyte, the fourth AB(IV).
From these combinations it becomes clear that mixing hemagglutinogens and agglutinins of the same name is impossible (hemagglutinogen A with hemagglutinin ά or hemagglutinogen B with hemagglutinin β).
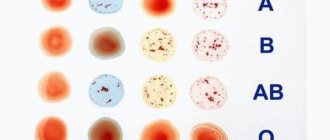
This is the basis for determining the blood group using various methods:
- The standard method uses human red blood cells and standard sera containing agglutinins ά and β. Mixing drops with the same hemagglutinogens and hemagglutinins causes agglutination (formation of flakes, clots). The decisive factor in the determination will be that mixing where agglutination does not occur, that is, there is a coincidence in hemagglutinogens and agglutinins.
- The cross-reaction method uses human serum and standard red blood cells (A (II) and B (III)). The results are assessed using special tables.
- One of the most reliable and accessible methods today is determination using zoliclones. Zoliclones are synthetic serum substitutes with agglutinins ά and β. In this method, zoliclones are mixed with human red blood cells and the result is evaluated using tables.
The Rh factor is also represented by a special molecule on the surface of red blood cells, the presence of which allows us to divide all variants into Rh positive (Rh) and Rh negative (Rh-) blood.
Determining the Rh factor is similar to determining the blood group, since in this case anti-Rh serum or monoclonal anti-D antibodies are used, which react with the Rh factor (agglutination occurs).
If we talk about the Rhesus system, then there are two of them – positive (Rh( )) and negative (Rh(-)). The Rh factor is influenced by the presence of a special protein in the membranes of red blood cells. If it is present, then the Rh factor is positive.
Blood type and Rh factor directly affect the patient's health during transfusion. It is prohibited to transfuse plasma with different Rhesus values. This can be fatal.
At the beginning of the 20th century, scientists developed a conditional classification into groups from 1 to 4, each of which is divided into two subtypes - negative or positive - depending on the Rh factor.
The difference lies in the content of specific proteins on the surface of red blood cells - agglutinogens A and B, whose presence affects the belonging of a particular person’s plasma to a certain group.
If the D antigen is present, then Rh is positive (Rh); if antigen is absent, it is negative (Rh-). This separation allowed for safe transfusion, but previously the procedure often ended in death due to the patient’s body’s refusal to accept the donor material.
The content of red blood cells and proteins affects a person’s blood group. The agglutination reaction—the detection of antigens A and B in the test plasma using sera—determines whether the plasma belongs to one group or another according to the accepted classification system (AB0).
In Russia the following designation applies:
- the first – 0 (zero), or I, no antigen;
- the second - A, or II, contains only antigen A;
- the third - B, or II, there is only antigen B;
- the fourth is AB, or IV, both antigens A and B are present.
The blood type is determined at the genetic level by passing on antigens A and B to offspring.
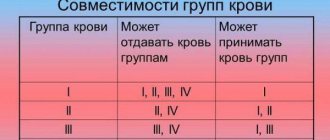
Compatibility
In standard situations, only similar blood is used. The concepts of “universal donor” and “universal recipient” are interpreted a little differently today:
- The first is a universal donor material: erythromass, because There are no antigens on the surface of these formed elements.
- The fourth is universal donor plasma, because It does not contain antibodies to a-, b-agglutinogens (subject to negative Rhesus).
The whole mixture is used only in two cases. This is done in the event of the development of Rh conflict and in the case of using one’s own blood, which was collected from cavities during surgery, as well as collected and prepared using the dilution method.
0 (I)
Carriers 0 (Rh -) are potential universal donors of red blood cells for any person, then 0 positive - for a recipient with any positive group. With the use of biomaterial in these patients, everything is different. For type I, it is permissible to transfuse only the first. Moreover, if the rhesus is negative, it is permissible to infuse 0 (Rh -), and if the rhesus is positive, the rhesus of the transfused fraction is not important.
A (II)
It suits few people. Transfusions can only be given to patients in the same group or IV (Rh+). A recipient with type II negative blood is allowed to receive only I and II negative blood transfusions. In the presence of Rh II positive, the infused groups do not matter.
B (III)
Blood III (Rh+) can be transfused III positive and IV (Rh+). And to the third negative one it is permissible to add only a similar one.
AB (IV)
Patients with the fourth negative can receive plasma of any negative group. But you can donate blood, regardless of the type of rhesus, only to carriers of the fourth group.
| Recipient | Donor | |||||||
| 0 (I) (-) | 0 (I) (+) | 0 (II) (-) | 0 (II) (+) | 0 (III) (-) | 0 (III) (+) | 0 (IV) (-) | 0 (IV) (+) | |
| 0 (I) (-) | + | |||||||
| 0(I) (+) | + | + | ||||||
| A(II) (-) | + | + | ||||||
| A(II) (+) | + | + | + | + | ||||
| B(III) (-) | + | + | ||||||
| B(III) (+) | + | + | + | + | ||||
| AB(IV) (-) | + | + | + | + | ||||
| AB(IV) (+) | + | + | + | + | + | + | + | + |
The value of “golden” blood for society and science
Although such blood is called golden, in fact it is not. It would not be bad if absolutely all people on the planet had such blood. This would help save many more lives than one can imagine. And that makes it incredibly valuable. Such blood is considered universal because it can be used for transfusion to all people, regardless of their Rh factor (85% of people have positive blood and 15% have a negative Rh factor).
The antigens found in this blood type are expressed with two proteins: RhD and RhCE. For their proper functioning, the body requires a glycoprotein (labeled RhAG). These proteins, in combination with a glycoprotein, glycophorin, are capable of forming another protein that is able to penetrate the red blood cells through the membrane.
The main group of these cells is capable of transporting oxygen and carbon dioxide through the blood. At the same time, the normal spherical structure of red blood cells is maintained, which means saturating the body with the energy necessary for functioning.
What is the most common blood type?
However, type and Rh factor are not the only indicators. About a dozen additional characteristics have been discovered and there are 30 types of biofluid. But only two of them are used to determine blood type.
The most common blood group in the world is 0 Rh+. This is explained by the absence of antigens in the red blood cells.
Interesting! It is believed that other groups descended from the first due to the occurrence of mutations as the type of food, lifestyle and place of residence changed. In addition, with the development of transport and increased migration opportunities, the number of interethnic marriages has increased, which also affected the mutation of genes encoding the composition of biofluids.
Table: Prevalence of blood groups by country in percentage terms with positive and negative Rhesus
| A country | Blood groups | |||
| 0 (I)Rh+/ 0 (I)Rh-, % | A(II)Rh+/ A(II)Rh-, % | B (III)Rh+/ B (III)Rh-, % | AB (IV)Rh+/ AB (IV)Rh-, % | |
| Australia | 40/9 | 31/7 | 8/2 | 2/1 |
| Austria | 30/7 | 33/8 | 12/3 | 6/1 |
| Belgium | 38/7 | 34/6 | 8,5/1,5 | 4,1/0,8 |
| Brazil | 36/9 | 34/8 | 8/2 | 2,5/0,5 |
| Great Britain | 37/7 | 35/7 | 9/2 | 3/1 |
| Germany | 35/6 | 37/9 | 9/2 | 4/1 |
| Denmark | 35/6 | 37/7 | 8/2 | 4/1 |
| Canada | 39/7 | 36/6 | 7,6/1,4 | 2,5/0,5 |
| China | 40/0,31 | 26/0,19 | 27/0,14 | 7/0,05 |
| Israel | 32/3 | 34/4 | 17/2 | 7/1 |
| Ireland | 47/8 | 26/5 | 9/2 | 2/1 |
| Iceland | 47,6/8,4 | 26,4/4,6 | 9,3/1,7 | 1,6/0,4 |
| Spain | 36/9 | 34/8 | 8/2 | 2,5/0,5 |
| Netherlands | 39,5/7,5 | 35/7 | 6,7/1,3 | 2,5/0,5 |
| New Zealand | 38/9 | 32/6 | 9/2 | 3/1 |
| Norway | 34/6 | 42,5/7,5 | 6,8/1,2 | 3,4/0,6 |
| Poland | 31/6 | 32/6 | 15/2 | 7/1 |
| Russia | 23/4,5 | 33/4,5 | 20/3 | 8/1 |
| Saudi Arabia | 48/4 | 24/2 | 17/1 | 4/0,23 |
| USA | 37,4/6,6 | 35,7/6,3 | 8,5/1,5 | 3,4/0,6 |
| Türkiye | 29,8/3,9 | 37,8/4,7 | 14,2/1,6 | 7,2/0,8 |
| Finland | 27/4 | 38/6 | 15/2 | 7/1 |
| France | 36/6 | 37/7 | 9/1 | 3/1 |
| Estonia | 30/4,5 | 31/4,5 | 20/3 | 6/1 |
| Sweden | 32/6 | 37/7 | 10/2 | 5/1 |
| Japan | 33/6,1 | 42/7,3 | 8,3/1,2 | 3,5/0,6 |
| Total | 36,44/4,33 | 28,27/3,52 | 20,59/1,39 | 5,06/0,4 |
In Russia, group II is common, followed by I, III and IV. There are much more people with positive blood - almost 85%. It is believed that all people initially had the D antigen, but under the influence of some factors a mutation occurred and it disappeared. Therefore, only 15% of negative blood is a small amount, as with any mutations.
Does blood type change?
The type of biological fluid cannot change. False results that tests sometimes show in pregnant women or cancer patients are a mistake. Changes in hormonal levels or the presence of tumor markers disrupt biochemical parameters. Usually, when re-diagnosis is carried out, the “former” constant group is determined.
Interesting! In theory, the blood can change after a bone marrow transplant operation. But for this to happen, the native bone marrow must completely die, and the donor had a different group. However, for such a major operation, the donor must have an antigen profile that is as similar as possible to that of the recipient.
Rejection may occur because other tissues of the patient have their own antigens. In this case, blood group antigens are also taken into account, so changes in blood during a bone marrow transplant are impossible in practice.
How does blood type affect a person’s character?
The connection between the composition of liquid tissue and temperament has not been scientifically proven. However, in Japan it is given great importance, comparable in popularity to the zodiac signs in the West. In the country, horoscopes are drawn up, compatible partners are looked for, and even hired for certain positions, based on the results of the analysis. Sometimes it comes down to scientific racism. How is personality type interpreted by blood type:
- 0 (I) – leader, organizer, prone to causeless aggression – the most popular blood type among the Japanese.
- A (II) – balanced, sensitive, stubborn, purposeful.
- B (III) – creative personality, mobile, depressed.
- AB (IV) – soft-spoken, has a good imagination, a peacemaker.
In the Russian Federation, most people are sensitive and purposeful, because the second group is common. Perhaps it is precisely because of this that Russians are famous for their “broad souls.”
The predominance of the first blood group on the planet is explained by the absence of antigens in it. This increases the chances of survival in various conditions and rapid adaptation to changing environmental factors. Blood transfusion centers are always in demand, especially rare blood. You need to know your blood type in order to receive or provide high-quality, timely medical care if necessary.
The most precious blood in the world
Walter recalled that another friend of his had recently undergone open-heart surgery in the United Arab Emirates for only $20,000. He called the hospital and got permission to operate on Franziska. Father Akata's parishioners in the United States and Nigeria raised money, and three months later Francis Akata flew to the UAE for surgery.
However, a few days after her arrival, doctors informed the woman that she had a rare blood type: it matches only 0.2% of all people belonging to the Caucasian race. This blood type is called Lutheran B-negative. To complicate the situation, Franziska's blood also belongs to the first negative blood group - this is an infrequently encountered, but not officially considered a rare blood type, which many have even heard of. It occurs in approximately 5% of the world's population. However, this combination meant that Franziska's blood was so rare that finding a donor for her would be very difficult, if not impossible.
Since there was no suitable blood available in the UEA or other Gulf countries, Ms Akata had to fly home and wait until suitable blood was found. The hospital launched its own search but was unable to find anything over the next two weeks.
Walter requested the results of Francisca's blood tests from the hospital and began searching for compatible blood in the United States. He applied to one blood center after another until he was sent with a request to Philadelphia, where a database of all American donors with rare blood types is located. Finally, he managed to find a number of suitable donors.
However, the joy was short-lived: the rules for crossing borders are much more complicated for blood than for people. As Peyrard explains, sometimes sending blood from one country to another can be a bureaucratic nightmare. Walter learned, for example, that hospital rules in the UAE prohibited it from accepting blood donations from outside the Gulf states. This meant that Francis would not be able to use the blood he found in America.
The situation looked bleak, but during a chance conversation with a colleague, Father Akata learned about a small hospital in Cameroon, neighboring Nigeria, where a cardiac surgery department was opened with funding from the Catholic Church. Walter contacted the hospital and they confirmed that they could carry out the operation if he could arrange for suitable blood to be supplied.
The American Rare Donor Program reached out to the South African National Blood Service and found four suitable donors on its list. However, one of them could not be contacted, another could only donate blood after several months, and two more received a doctor’s ban on donating blood. These are all common concerns when it comes to rare blood donors. There are limits on how often people can donate blood. In addition, keeping track of donors can also be difficult - some get sick or die, others move without informing the blood transfusion service.
A South African frozen rare blood storage facility has two packs of matching blood, but frozen blood has a shelf life of just 48 hours compared to four weeks for fresh blood. If the blood bags had been held up by customs or for any other reason, the blood would have been unusable by the time it reached the hospital in Cameroon. To use the frozen South African blood, Francis would have to perform the operation in South Africa. Options were running out.