The 21st century is a time that requires strict control over your health. Due to polluted environment, poor diet, and stress, people increasingly began to seek help from a doctor. Blood type and Rh factor are those basic characteristics of the body on which human life in some cases depends (transfusion, organ transplantation, pregnancy and childbirth). Can BG change during life?
This question is periodically raised on the Internet, but getting a definite answer is not easy. Some users write that this cannot be, while others are sure that changing the group is possible. Which one is right?
Blood type: what's the point?
Before you figure out whether a person’s group is capable of changing throughout his life, it’s worth understanding what the essence of group classification is.
Human blood is a unique biomaterial, which differs from person to person. Its characteristics are determined in the womb.
With blood we receive the set of genetic material that is passed on to us by our father and mother. Direct group determination is a process that detects the presence or absence of specific antibodies in the blood. They are called agglutinins and agglutinogens.
Important! Antibodies are compounds that are created to stick together (agglutinate) various bacteria and viruses in the blood. These are original “fighters” that prevent the development of foreign bodies in the body. It is from this function that their name comes.
HA is a set of special antibodies that is present or not in plasma and cells. Red blood cells - erythrocytes - are capable of producing these substances. The main trigger for the production of antibodies is the presence of antigens. They are divided into two types - A and B. It is these substances that affect the group, which is taken as the basis for the AB0 group classification system. Due to their different combinations, scientists were able to identify four groups.
- 1 or 0 group. There are no agglutinogens in its composition, but at the same time, this type of blood has type A and B antibodies (agglutinins) in the blood plasma.
- Group 2 is designated “A”, this is due to the content of type A antigen. And there must be antibodies b in the plasma.
- Group 3 – antigen B and group A antibodies.
- Group 4 is a combination of two types of antigens - A and B, while there are no antibodies in it.
This classification is recognized throughout the world, but sometimes people simply have a poorly developed A-form. It is this fact that leads to the erroneous definition of the group.
Important! The group is not capable of changing throughout life, since it is a genetically embedded material that a person receives in the womb of his mother.
This feature can lead to accidents if compatibility is not checked in time. To correctly and accurately determine the group, doctors use special reagents to diagnose blood.
Why change is possible
Group affiliation can be established by gluing red blood cells. A small amount of serum containing agglutinins or antibodies - A and B, α and β - is poured onto a sterile glass. After this, a blood sample is added to the reagent, the volume of which should be 10 times less than the amount of serum. The red blood cell agglutination reaction is observed for 5 minutes under a microscope. As a result, you can identify your blood type:
- the absence of adhesion indicates group I, in which antibodies on red blood cells are completely absent;
- in the presence of a positive reaction with agglutinins A and α+β, group II is determined;
- the combination of B and α+β indicates type III;
- the absence of α+β and the presence of antibodies A and B indicate form IV.
Important information: What blood type cannot have an abortion and is it possible to terminate the first pregnancy with a negative Rh factor?
A change in blood group is possible only due to weak bone marrow formation of red blood cells or lack of antigen production. If group affiliation has changed, then this phenomenon indicates the presence of pathological processes, including:
- malignant neoplasms, leukemia, hematosarcoma;
- Cooley's anemia and other hematopoietic pathologies;
- infections affecting the bone marrow;
- pregnancy and pathological conditions characterized by increased synthesis of red blood cells.
In such situations, laboratory research methods cannot determine the type of agglutinins. Therefore, when deciphering the results, the blood group indicator may change to false for a short time. This does not indicate a complete change in group affiliation.
In some infectious diseases, pathogenic microorganisms begin to synthesize bacterial enzymes that transform the structure of agglutinin A like antigen B. As a result, the volumes of proteins by which the blood group and rhesus are determined change. This phenomenon leads to false interpretation of the results.
In clinical practice, a single case was recorded in Australia when genetic indicators simultaneously changed. After a liver transplant, the patient's immune system parameters changed.
Rh factor
Can the Rh factor change throughout life? It is worth remembering that the Rh factor is an inherited element that cannot change. Only those people who do not know what Rhesus is have an erroneous opinion about this blood feature.
In world history, only a single case was recorded when a young 15-year-old girl had a change in Rh.
This happened after a liver transplant. She managed to find out about this change in blood only 6 years after the organ transplant. The girl suffered from an immune disease, during the treatment of which a change in Rh was revealed.
Doctors say that this could only happen for one reason - the donor’s liver contained stem cells that entered the girl’s bone marrow. Her body accepted these substances and launched new immune processes. An additional factor that influenced the change in Rh could be the fact that the donor was a young guy. His blood had a low number of white blood cells.
Can the Rh factor change? The answer for most scientists remains the same - no. This is a genetic trait that cannot change in a healthy person.
Rhesus conflict - what is it?
Rh positive or negative is an individual trait for each person. It does not affect your well-being in any way, but for a woman this fact is quite important if she plans to get pregnant.
The mother's body perceives the child as a foreign body, and therefore begins active actions to reject it. Antibodies are synthesized in the blood of a pregnant woman, which are aimed at destroying the red blood cells of the child.
At this moment, the level of bilirubin in his body increases, which negatively affects the formation and functioning of the brain. At the same time, the liver and spleen enlarge, since these organs of the child are forced to neutralize and utilize a huge number of dead cells. As a result of the destruction of red blood cells, the child suffers from oxygen starvation, which leads to death if treatment is not started in time.
Attention! The threat of Rh conflict arises only if the mother is Rh- and the father is Rh+. The probability of a conflict developing is 75%. In this case, the first child of this couple is often born healthy, but it is important that the woman does not have contact with positive blood before this.
If there was a miscarriage after a Rh conflict, then Rh sensitization is possible in 3-4%; with normal childbirth, the percentage increases to 10-15.
Causes of errors in analyzes
The blood test for the group is based on the fact that α agglutinin glues red blood cells containing agglutinogen A, and β glues B. The patient’s blood is sequentially mixed with serum containing α, β and both agglutinins and looked under a microscope to see whether red blood cells stick together or not, therefore The sign determines the presence or absence of certain agglutinogens.
In some diseases, the number of red blood cells also increases, while the number of agglutinogens decreases so much that the gluing of red blood cells containing them will not occur. In this case, the analysis will show blood group I, although in reality the patient has II, III or IV.
Some pathogenic microbes secrete enzymes that change the molecular composition of agglutinogens A, as a result of which they become similar to B, and then the analysis will show blood group III instead of II. After recovery, everything will return to normal. Distortions are also possible with blood cancer.
Thus, the blood type cannot change during life, but in some diseases and during pregnancy, conditions arise that make it difficult to establish the blood group and lead to errors in the analysis.
Recently, an acquaintance told me that his wife, while undergoing tests during pregnancy, “changed” her blood type. Was the third, became the first. The logical question is: HOW? After all, the blood type is genetically determined... And it can only change in a spider-man. But, nevertheless, it is a fact: there was a third blood group (according to documents, tests were carried out more than once), but it became the first (a characteristic reaction to the first blood group). Therefore, the question still remains: can blood type change?
By the way, as a survey of friends showed, this is not an isolated case. There is another documented change, but this time in the Rh factor. How? Why? For what?
We will try to answer in this article, which is not in vain placed in the ““ section.
Can your blood type change? What’s most interesting is that if you ask a search engine about this question, you will find a LOT of forums where this issue is discussed. Usually the forum begins like this: “ My blood type has changed... Why?
»
This is followed by two different types of responses:
- this can never happen (I swear by Mendel!) - the doctors made a mistake (about 50% of answers)
- and my/my friend’s blood type has changed (about 50% of answers).
According to reports, the statistics are as follows:
- blood type changes are most often recorded in women
- This mainly occurs during pregnancy.
Undoubtedly, the possibility of medical error exists; This is why a compatibility test MUST be done when receiving a blood transfusion. So as not to guess, but to be sure. But a mistake is a mistake, and facts are facts: there was one blood type, but it became another. Why?
To answer, let's first understand blood groups.
To make it clear what can or cannot change in a blood group.
So, did you know that not the well-known 4 groups, but hundreds of billions of blood group combinations are possible? And just like that. Why is this so? Everything is very simple.
Certain substances are responsible for blood type, they are called “antigens”.
Why such a strange name “antigens”? It's just an acronym: anti
body-
gen
erating, antibody manufacturer. Antigens are signal beacons for the immune system that it is time to produce antibodies. Antibodies are special molecules whose task is to bind and neutralize antigens. Antibodies LITERALLY bind to antigens, they act like a kind of adhesive mesh. That's why many of them are called agglutinins, adhesives.
Antigens can be external or internal. The most dangerous antigens are parts of the membranes of bacteria and viruses (usually they come from outside). Consequently, as soon as familiar antigens appear in the blood (= attack by microorganisms), antibodies neutralize them. Also an example of antigens are substances that cause allergies.
For each antigen there is its own antibody. If the body has never had a certain antigen, then there will be no corresponding antibodies. The antigenic mechanism of immunity is the body's memory of diseases. This is protection for the future. This is how vaccinations work. For new diseases for which there are no antibodies, there are other immune mechanisms.
In connection with blood group, we are interested in internal antigens. These are substances that are attached to the membrane of red blood cells, red blood cells, oxygen/carbon dioxide carriers.
Since there are HUNDREDS of antigens in the blood, hundreds of billions of possible combinations (= blood groups) can be constructed. But in connection with the well-known blood groups (1, 2, 3, 4 and Rh factor), we are only interested in antigens A, B and Rh.
So, in a simplified form, 4 cases are possible:
- There is antigen A on the membrane of red blood cells. Blood group is second (denoted A). There are β antibodies in the blood
- There is antigen B on the membrane of red blood cells. Blood group is third (denoted B). There are α antibodies in the blood
- The membrane contains both A and B. Blood group is fourth (designated AB). There are no α and β antibodies in the blood
- There are no these antigens on the shell. Blood group first (denoted O). There are both α and β antibodies in the blood
Plus two options:
- There is an Rh antigen on the membrane of red blood cells. Rh factor is positive (because the substance is present)
- There is no Rh antigen on the membrane of red blood cells. The Rh factor is negative (since there is no antigen).
What does this give us? This gives knowledge about the presence of certain antibodies in the blood. And also the ability to predict what will happen if the blood of one group is mixed with the blood of another group. Roughly speaking: there will be adhesion, blood clotting, or not.
So, we remember: for each antigen there is a “personal” antibody that will stick this antigen together.
Hence:
- A + α = × (axe head)
- B + β = × (axe head)
- A, B + α = × (axe head)
- A, B + β = × (axe head)
- A + α, β = × (axe head)
- B + α, β = × (axe head)
- A, B + α, β = × (axe head)
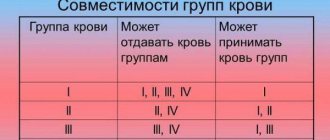
Accordingly, if there is already, say, antibody α in the blood, then there SHOULD NOT BE antigen A in the infused blood. Otherwise, there will be agglutination and agglutination. In general, trouble. All patterns with A, B, etc. can be expressed as a table:
| recipient (to whom) | ||||||
| antibodies | α, β | β | α | 0 | ||
| antigens | blood type | 1 | 2 | 3 | 4 | |
| donor (from whom) | 0 | 1 | + | + | + | + |
| A | 2 | × | + | × | + | |
| IN | 3 | × | × | + | + | |
| AB | 4 | × | × | × | + | |
Or, which is much simpler, with a drawing:
With the Rh factor it’s the same story; the given table simply becomes 2 times more complicated. But this does not scare us; it is important for us to simply understand the antigens. We have tried to illustrate their functions and presence through a description of blood transfusion. We hope we succeeded.
By the way, an interesting question: why do some people have antigens and others don’t?
There is no answer to this question. But there is an assumption: these may be the remains of symbiotic microorganisms (for example, viruses), which during the process of evolution gradually “dissolved” in the body. So, did you know that mitochondria (the energy stations of cells that have their own DNA) are most likely bacteria that long ago, in ancient times, entered into symbiosis with nuclear cells? And like this