General information
Phlebitis is an inflammatory process in the wall of a venous vessel. Pathology can develop under the influence of certain factors, but most often phlebitis is a complication of varicose veins of the lower extremities . Rarely does the disease occur in isolation. The inflammatory parietal process changes the structure of the venous wall, which can lead to the formation of a blood clot and a complication such as thrombophlebitis. In the age group over 50 years old, 0.7% of men and 1% of women suffer from phlebitis.
Possible complications
If a vein in your leg is inflamed, what you cannot do is self-medicate. It must be remembered that all medications must be prescribed by a doctor, and traditional methods are intended only to make you feel better, but they will not get rid of the root cause of the disease.
Ignoring pathology is also unacceptable. This can lead to the following pathologies:
Thus, if a vein in the leg becomes inflamed, a specialist should indicate what to do. This is the only way to avoid the development of complications.
Classification
According to the nature of the flow:
- Acute phlebitis . Accompanied by severe pain, fever and weakness.
- Chronic phlebitis. For a long time it is practically asymptomatic; symptoms appear only during exacerbations.
By location of the lesion:
- Phlebitis of the superficial veins.
- Phlebitis of deep veins.
According to the location of inflammation in the vein:
- Endophlebitis. The inflammatory process is localized in the inner lining of the vein.
- Periphlebitis. The inflammatory process affects the outer lining of the vein.
- Panphlebitis. All membranes are involved in inflammation: internal and external.
Classification based on the cause of phlebitis:
- Allergic phlebitis. Associated with allergic response .
- Post-injection phlebitis. It is formed as a result of the aggressive effects of drugs administered by injection (after a dropper). The post-injection variant may be associated with mechanical trauma.
- Cerebral phlebitis. Against the background of purulent inflammatory processes and infectious diseases, the veins of the brain are affected.
- Painful phlebitis. It is acute, accompanied by severe pain and most often develops in the postpartum period.
- Migrating phlebitis. The disease is more often observed in young males and is associated with a long-term inflammatory process in the veins of the lower extremities. Characterized by a recurrent course and spread to the arterial walls.
- Phlebitis of the penis. The pathology is based on an infectious disease ( gonorrhea ) or varicose veins. Characteristic is the appearance of a voluminous cord-like compaction on the dorsal surface of the penis, accompanied by severe swelling of the adjacent tissues.
- Phlebitis of the portal vein (pylephlebitis). Formed after complications associated with inflammatory processes in the abdominal cavity (peptic ulcer of the digestive tract, appendicitis, inflammation of hemorrhoids, purulent inflammation of the genital organs, liver abscess , purulent infections of the umbilical vein in a newborn, dysentery , etc.). Very often ends in death.
Inflammation of a vein in the arm
Varicose veins are not typical for the upper extremities, so the inflammatory process in the arm develops for other reasons:
- changes in blood clotting ;
- tendency to increased thrombus formation, including genetic predisposition;
- decreased immunity ;
- decrease in blood flow speed in pathology of the cardiovascular system.
The trigger for the development of phlebitis on the arm is damage to the walls of a blood vessel or the entry of an infectious agent.
Inflammation of the veins in the legs
The lower extremities are characterized by varicose veins. Inflammation of the veins in the legs can also be acute or chronic. Phlebitis of the lower extremities very often develops on varicose veins of the legs.
Decoctions and infusions for oral use
Simultaneously with local treatment, you can take medicinal agents orally. If a vein in your leg becomes inflamed, what to do:
It is important to remember that any medicinal plant is a potential allergen. Often, while taking decoctions and infusions, an allergic reaction occurs. If alarming signs appear, treatment of phlebitis with folk remedies must be completed.
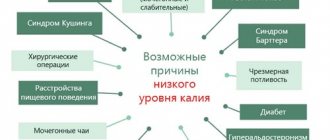
Causes
Inflammation of the venous wall can occur under the influence of certain factors. Most often, the cause lies in varicose veins, less often in infection of the vascular wall. Inflammation can be caused by various pathogenic microorganisms, the first among which is streptococcus . The pathology begins to progress as a complication of purulent wounds, abscesses and infectious diseases.
The vascular wall can become inflamed after mechanical damage as a result of:
- injuries;
- chemical burn of a vein after injection of certain drugs with an aggressive effect;
- venous puncture during intravenous infusion or blood sampling.
Phlebitis can also manifest itself as an allergic reaction due to the entry of allergens into the patient’s body. In the postpartum period, there is prolonged stagnation of blood in the lower half of the body, which can also lead to the development of phlebitis.
Factors influencing the development of the disease:
- physical inactivity, sedentary lifestyle;
- obesity , excess weight;
- long-term bed rest;
- limb immobilization after traumatic injury;
- pregnancy;
- excessive physical stress.
Symptoms of phlebitis
Symptoms of phlebitis depend on the type and form of the disease and are characterized by great diversity.
Symptoms of phlebitis of the lower extremities with damage to the superficial veins
Damage to the superficial veins is typical for the lower extremities and can be caused as a complication after injections. Signs characteristic of an acute inflammatory process:
- redness of the skin;
- pain syndrome during inflammation of the vein;
- tension;
- local increase in temperature;
- skin thickening;
- the appearance of red stripes along the inflamed vessel.
In the acute period, severe weakness, dizziness and elevated body temperature often appear. In a chronic course, the symptoms are erased, obvious signs are noted only during the period of exacerbation. During remission, there may be a slight increase in body temperature and seemingly unreasonable weakness.
Phlebitis of deep veins (acute and chronic form)
Damage to the veins of the lower extremities is typical. Symptoms of inflammation of a vein in the leg:
- swelling;
- pain syndrome;
- the skin becomes milky white;
- local hyperthermia, redness and thickening are not observed;
- severe weakness;
- increase in body temperature.
Quite often, acute phlebitis of the deep veins in the leg and arm is complicated by thrombophlebitis . In a chronic course, all the above-described symptoms appear only during the period of exacerbation of the disease.
Phlebitis of the penis
Characteristic symptoms:
- redness and pain in the area of compaction;
- painful and weight-like formation on the back of the penis;
- swelling;
- the penis is semi-erect;
- spread of edema to the scrotum and foreskin.
When cicatricial complications form, the penis may remain swollen, but most often the disease responds well to therapy and goes away almost without a trace.
Cerebral phlebitis
With inflammation of the veins of the brain, specific symptoms are noted:
- increased blood pressure;
- severe, intense headache;
- neurological symptoms: sleep disturbances, confusion, fainting, speech disorders, etc.;
- weakness throughout the body.
Pylephlebitis
Inflammation of the portal vein is accompanied by clear signs of purulent intoxication: increasing weakness;
- a sharp deterioration in general health;
- jaundice;
- headache;
- gagging;
- hectic fever ;
- cramping pain in the area of the hepatic system;
- severe chills and drenching sweat.
Pylephlebitis often leads to death, and when the pathology becomes chronic, the patient develops liver or kidney failure.
Compresses
The disease requires an integrated approach to treatment. It is recommended to alternate rubbing with compresses, and the latter can be done at night. This will allow you to achieve maximum therapeutic effect.
If a vein in the leg is inflamed, how to treat the disease at home using compresses is described below:
The minimum duration of compress application is 30 minutes. But it is better to carry out the procedure at night.
Tests and diagnostics
Typically, the diagnosis of phlebitis of both superficial and deep veins does not cause difficulties. A phlebologist may suspect a disease based on complaints from patients and examination data. To identify other forms and causes of inflammation of the veins and prevent the development of inflammation, a comprehensive examination is carried out.
Laboratory and instrumental research methods:
- ultrasound duplex scanning of blood vessels;
- blood tests: C-reactive protein, prothrombin index, coagulogram , CBC, thrombelastogram;
- phlebography;
- Ultrasound of vessels of adjacent organs.
More accurate instrumental diagnostic methods carried out for suspected thrombophlebitis:
- CT phlebography with contrast;
- phlebomanometry;
- Phleboscintigraphy.
Care and prevention of phlebitis of veins
Phlebitis lasts from 10 days to 2-6 weeks in the case of the superficial type and from three to six months in the case of deep vein phlebitis. As a rule, this condition does not require hospitalization, with the exception of severe cases.
So, let's see what remedies should be used to prevent phlebitis of the superficial and deep veins.
Natural remedies and protection
Non-pharmacological therapy for phlebitis, both superficial and deep, aims to reduce symptoms and dissolve the resulting blood clot.
- Bandage: An elastic bandage is used to treat phlebitis of deep and superficial veins and is wrapped around the affected part for effective compression. This reduces the swelling that occurs as a result of inflammation and therefore reduces pain, redness and swelling. In addition, the elastic bandage helps normalize the speed of blood flow. Bandages can be impregnated with zinc oxide, which has an anti-inflammatory and disinfectant effect, and also accelerates the healing process.
- Elastic stockings: used as support therapy and have different levels of compression, which are chosen in accordance with the recommendations of the doctor. It works on the same principle as an elastic bandage.
- Vascular physiotherapy: This is a set of techniques that use drainage and pressure therapy to improve blood circulation and lead to the dissolution of clots.
- Keep your legs elevated: Elevating your legs while you lie down helps stimulate venous circulation and avoid blood stagnation. This is a remedy that is also considered valid for the prevention of thrombophlebitis.
- Application of compresses: You can support blood circulation with local therapy through the use of compresses on the affected areas, alternating hot and cold compresses (for example, alternating a heating pad and an ice pack).
- Diet: The diet of those suffering from phlebitis should contain many antioxidant components such as tomatoes, red fruits, citrus fruits and all foods containing flavonoids and vitamin C. These elements help strengthen the walls of the veins and are natural anti-inflammatory agents. Among the foods that should be avoided are fats of animal origin, such as butter or meat, because they cause the accumulation of fat at the level of blood vessels, worsening the problem.
- Herbal medicine: plants are mainly used to treat superficial phlebitis, in particular, hawthorn and holly are actively used.
Holly is an evergreen plant that contains active ingredients such as camphor essential oils, anethole, resins, flavonoids and linalyl acetate. These active substances have an anti-inflammatory effect, strengthen capillaries and counteract the development of varicose veins, therefore, are useful in the treatment of phlebitis because they help improve blood circulation.
- Spa treatments: You can use the benefits of thermal waters to improve venous blood circulation. However, this remedy is not suitable for all types of phlebitis, so before going for a spa treatment, consult your doctor to avoid worsening the problem.
Hawthorn is a perennial plant that contains active ingredients such as tannins, vitamin C, oxalic acid and its derivative terpenes. Acts on peripheral blood circulation - stimulates and improves it, therefore, helps cure phlebitis.
Using medications to treat phlebitis
Drug therapy is suitable for the treatment of both superficial phlebitis and deep vein phlebitis. It is used to reduce symptoms and speed up healing.
In particular, the following medications are used:
- Anti-inflammatory and pain relievers: serve to reduce inflammation and fight pain. The most commonly used are ibuprofen and paracetamol. In the case of superficial phlebitis, it is sufficient to use an ointment with anti-inflammatory components.
- Anticoagulants: used to improve free blood circulation and have an antiplatelet effect on platelets. The most commonly used are heparin and warfarin.
- Fibrinolytic: drugs that cause fibrin clots to dissolve and therefore they help dissolve the clot. Among them are tissue plasminogen activator, streptokinase and urokinase.
- Antibiotics are used to prevent infections. One of the most commonly used is amoxicillin, which has a wide spectrum of action.
Attention: the choice of the type of drug used, combination of drugs, dosage and duration of therapy are determined solely by the doctor, depending on the individual situation.
If drug therapy does not bring the expected effect, then surgical methods are used.
Surgery – surgery in severe cases
If drug therapy and non-pharmacological treatment do not produce results, or in the case of severe phlebitis, surgery is resorted to:
- Varicose vein removal: In case phlebitis occurs in one or more varicose veins, the doctor may decide to remove these veins to permanently solve the problem. The intervention is performed on an outpatient basis, and full recovery occurs within a few weeks.
- Placement of a venous filter: This intervention is performed when the patient cannot take anticoagulants, involves installing a filter in the cavity of a large vein, such as the abdominal vena cava, which will prevent the blood clot from passing to vital organs such as the brain, heart and lungs. It is performed with hospitalization under ordinary local anesthesia.
- Bypass surgery: In more severe cases, bypass surgery may be necessary to restore normal blood circulation.
Treatment of phlebitis
Treatment of phlebitis of the lower extremities
If superficial veins are affected, treatment can be carried out on an outpatient basis, but for other forms of pathology hospitalization is necessary. Inflammation of the veins of the lower extremities requires complete rest of the affected limb, which is given an elevated position.
Treatment of inflammation of the vein in the leg is conservative and includes:
- taking medications;
- physiotherapeutic procedures;
- adherence to a certain regime.
Treatment of inflammation of a vein in the arm caused by puncture of a vessel or catheterization is based on the use of pain relief therapy only.
Treatment for phlebitis of a vein in the arm is the same as for damage to a vessel in the lower limb.
Treatment at home: rubbing
Even at the very beginning of the development of the pathological process, a person’s quality of life deteriorates significantly. All he cares about is how to relieve the pain of an inflamed vein in his leg. It is important to know that the use of alternative medicine is acceptable, but they cannot be considered as the main method of treatment. Traditional methods help relieve pain, but do not eliminate the root cause of the development of pathology.
Rubbing is effective for phlebitis. The most effective are the following recipes:
These remedies, according to reviews, are extremely effective if a vein in the leg is inflamed. How to treat an illness at home if signs of an undesirable reaction occur? It is important to remember that all medicinal plants are potential allergens. If alarming signs appear, treatment must be completed or another method must be chosen.
Medicines
Drug therapy involves taking the following medications:
- non-steroidal anti-inflammatory drugs: Ibuprofen , Ketoprofen , Diclofenac ;
- antibiotics (for infection);
- drugs that reduce blood viscosity: Cardiomagnyl , ThromboASS ;
- drugs that improve microcirculation: Pentoxifylline , Vazaprostan , Actovegin , Reopoliglyukin ;
- local remedies: Troxevasin , Heparin ointment , Voltaren , Venobene ;
- antihistamines: Pipolfen , Suprastin , Cetrin ;
- drugs that reduce prothrombin levels: Dicumarin , Phenylan .
The choice of a specific drug, dose selection and determination of the duration of therapy is determined by the attending physician, taking into account the severity and form of the disease, as well as the individual characteristics of the patient.
Prevention
Prevention methods to prevent the development of recurrent phlebitis depend on the location, cause of occurrence and individual characteristics of the patient:
- maintaining a healthy lifestyle;
- smoking cessation;
- adequate physical activity;
- timely treatment of infectious and purulent diseases;
- prevention of complications after injections;
- prevention of infectious diseases;
- for varicose veins, regular preventive courses using Heparin ointment and wearing compression stockings;
- strengthening the immune system;
- dispensary observation by a phlebologist;
- regular use of antiplatelet agents for prophylactic purposes at the risk of developing thrombophlebitis.