Detailed description of the diagnostic method
Based on such data, one can draw conclusions not only about the electrical activity of this organ, but also about the structure of the heart muscle. This means that using an ECG it is possible to diagnose various heart diseases.
The functioning and contractile activity of the heart are possible due to the fact that spontaneous impulses constantly arise in it. Within normal limits, their source is localized in the sinus node, which is located next to the right atrium. The purpose of such impulses is to travel along nerve fibers through all parts of the heart muscle, causing them to contract. When the impulse passes through the atria and then through the ventricles, they alternately contract, which is called systole. During the period when impulses do not occur, the heart begins to relax and diastole occurs.
Consequences and complications
Coronary heart disease, in the absence of the required therapy, can lead to the formation of progressive heart failure. Muscle contractility weakens. As a result, the heart stops providing the body with the required amount of blood. Patients with cardiac ischemia become fatigued quickly and experience constant fatigue. If no measures are taken to treat the disease, the matter may result in disability or even death.
What is it based on?
ECG diagnostics is based on recording the conduction of electrical impulses that occur in the heart. For this purpose, an electrocardiograph is used, the principle of which is to record the difference in bioelectric potentials that arise in different parts of the organ at the time of contraction and relaxation. Such processes are recorded on heat-sensitive paper in the form of a graph, which consists of hemispherical or pointed teeth and horizontal lines in the form of spaces. An ECG for ischemic heart disease and angina pectoris is prescribed very often.
In order to record the electrical activity of the organ, it is necessary to fix the electrocardiograph electrodes on the legs and arms, as well as on the anterolateral surface of the sternum on the left. This allows you to register all directions of electrical impulses.
Each of the leads indicates that they record the passage of an impulse through a specific area of the heart, thanks to which doctors receive the following information:
- about the location of the heart in the chest;
- about the structure, thickness and nature of blood circulation of the atria and ventricles;
- about the regularity of impulses in the sinus node;
- about obstacles in the path of impulses.
How is the procedure performed?
An electrocardiogram is a safe and accurate method for determining ischemia of the heart muscle. All necessary operating parameters will be recorded within 10 minutes.
The procedure is carried out in the following order:
- The patient removes clothing from the chest and frees the leg area from the knee to the foot.
- The specialist conducting the examination lubricates the necessary areas with a special gel and secures the electrodes.
- The data will be transmitted through the electrodes to the sensor.
- The device displays the transmitted information on paper in the form of graphs.
- The specialist interprets the results obtained.
What is myocardial ischemia?
Let's find out what is ischemic heart disease (ICD-10 I20-I25), or coronary heart disease.
The heart is the most powerful muscle in the human body. It can pump up to 7000 liters of blood per day at a speed of 1.5 km/h, which can be compared to the operation of a pump. Along with this, the heart is highly sensitive to oxygen starvation, which often leads to damage to cardiac tissue. The main method in the study of heart diseases, including any form of coronary artery disease, is the ECG, which is a recording of electrical impulses carried out in all leads, which helps to detect even long-standing symptoms of myocardial ischemia. Patients who have previously experienced a lack of oxygen should be especially careful and undergo regular medical examination to prevent the recurrence of coronary artery spasms.
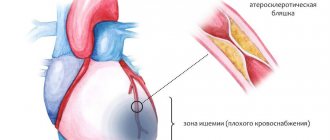
IHD (ICD-10 I20-I25) is a condition that occurs as a result of disturbances in the flow of arterial blood to the heart muscle due to blockage of the coronary vessels or their spasm, and occurs in a chronic or acute form. When the heart does not receive the volume of oxygen it needs, areas of connective tissue are formed in the lumens of the muscle fibers that have lost the ability to fully function. The process of damage to the heart muscle always occurs with the development of minor ischemia, which, without appropriate therapy, over time provokes the occurrence of a true heart attack.
What can be seen on an ECG with ischemic heart disease is of interest to many.
Classification
What is she like? Experts identify several forms of coronary heart disease:
- Primary cardiac arrest.
- Acute coronary insufficiency.
- Angina pectoris is a form of coronary artery disease characterized by squeezing and pressing discomfort.
Typically, such manifestations are mainly localized behind the sternum. Painful sensations and discomfort may also radiate to the left arm, epigastric region, and jaw. This pathology usually develops as a result of physical activity. There are several forms: primary, progressive, vasospastic.
Pathogenesis of the disease on the ECG
The pathogenesis of IHD is as follows:
- Stable angina, which is characterized by pressing paroxysmal pain in the chest area, which occurs under the influence of physical activity and gradually disappears when stressful conditions are eliminated. Most often there is ischemic heart disease with rhythm disturbance.
- Unstable angina, which is an intermediate period between stable ischemia of the heart muscle and the development of various complications. Its main clinical symptom is chest pain, which develops even in a calm state and can provoke damage to heart tissue cells.
- Small-focal myocardial infarction, which is a rather insidious variant of coronary artery disease and is characterized by the absence of a pathological Q wave on the ECG, as well as microscopic foci of tissue death. Often these disorders go unnoticed because they are disguised as an acute attack of angina.
- Q-myocardial infarction. The most dangerous complication of myocardial ischemia is considered to be a large-focal infarction, which is characterized by transmural damage to the heart muscle with ST segment elevation and the formation of an additional Q wave, which persists even after complete replacement of necrotic areas with connective tissue.
This is how informative an ECG can be for ischemic heart disease.
Diagnosis using ECG
Diagnosis of coronary artery disease using an ECG does not require specific patient preparation. The examination does not depend on the time of day. Electrodes are placed on the patient's body, which are located on the chest and limbs. On average, the procedure lasts 5-10 minutes. Electrocardiography does not cause any adverse reactions, so it can be repeated if necessary.
Thanks to this study, the following ischemic changes on the ECG can be detected:
- rhythm disturbance;
- changes after a heart attack;
- myocardial hypertrophy;
- disruptions of the cardiac cycle.
In this case, the cardiogram is conventionally divided into several sections, each of which has its own description: myocardial ischemia (T wave), ischemic damage (ST segment) and myocardial necrosis (Q wave).
Additional examinations
Since the signs of ischemic processes in some subtypes of this disease are the same, a number of additional examinations have been installed to determine a heart attack. Early markers of cardiac muscle necrosis include creatine phosphokinase and myoglobin. For the most accurate diagnosis, after 7-9 hours it is advisable to examine the level of troponins, aspartate aminotransferase and lactate dehydrogenase. ST segment elevation is sometimes observed not only during the development of a heart attack, it often occurs with unstable angina, as a result of which it is necessary to take into account all visual changes in the waves on the electrocardiogram.
How to diagnose the disease?
Many people believe that IHD can be determined by an ECG. Signs of myocardial ischemia can also be established by performing the following examinations:
- Anamnesis collection. For this purpose, the doctor must ask the patient in detail about the nature of the pain, discomfort, and its location. The doctor will also find out whether the patient feels weak and has trouble breathing.
- Examination by a cardiologist. At this stage, the doctor should listen to the heartbeat for the presence of wheezing and murmurs. Also during the examination, the doctor measures your blood pressure level.
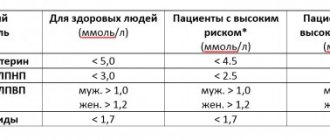
- General blood analysis. Allows you to identify the possible cause of ischemia. Experts evaluate indicators such as triglyceride and cholesterol levels. This is especially important for assessing the risk of vascular atherosclerosis. The level of troponins in the blood is also considered an important indicator. When heart muscle cells are destroyed, specific enzymes are released into the blood.
- Coagulogram. With coronary heart disease, blood clotting increases significantly.
- Electrocardiography. Allows you to identify excess size of the left ventricle and other specific characteristics. A doctor can easily identify signs of ischemia on an ECG.
- Echo ECG. With this type of examination, the structure and size of the organ are assessed, and the blood flow inside the heart, the functioning of the valves and the degree of vascular damage are also studied.
- Daily monitoring. With this method of examination, special equipment reads the electrocardiogram within 24-72 hours. This procedure allows you to objectively assess the patient’s condition and accurately determine the causes of symptoms of coronary heart disease.
- Radiography. Used to detect left ventricular dilatation. This pathology may be a consequence of aortic dissection. This type of examination also allows us to identify other complications.
What to do if cardiac ischemia was detected on the ECG? As a rule, to make an accurate diagnosis, the doctor uses a whole list of additional examinations. These include stress tests, X-ray contrast examination, computed tomography, Doppler sonography, electrophysiological examination, etc.
Manifestations of ischemia on the electrocardiogram
It is quite difficult to answer unequivocally what the ECG results for IHD will look like on film. When hypoxia of the heart muscle occurs, the movement of electrical potentials slows down slightly, potassium ions leave the cells, which negatively affects resting potentials. At the same time, compensatory processes are launched, the heart begins to overstrain, pressing pain develops behind the sternum, and the patient is disturbed by an unpleasant feeling of lack of air.
Characteristic ECG signs in chronic ischemic heart disease and oxygen starvation of cardiac tissues are:
- Oblique or horizontal depression of the ST segment.
- Reduction of the T wave, or its movement below the horizontal line.
- Widening of the T wave due to slower ventricular repolarization.
- The appearance of a pathological Q wave with the development of large-focal necrosis.
- The dynamics of changes in the electrocardiogram, which is a sign of the “freshness” of the pathological process.
ECG signs of ischemic heart disease should not be ignored. Additionally, the image may show signs of arrhythmias and blockades, which arise as a complication of ischemic processes. In most cases, with the development of ischemia of the heart muscle on the ECG, the QRS complex retains its normal shape, since oxygen deficiency primarily affects the restoration (repolarization) of the ventricles, which completes the cardiac cycle within normal limits.
Clinical recommendations for ischemic heart disease will be given below.
ECG changes in various types of angina
Variant angina
This is a difficult type of angina to identify based on the symptoms that appear. Therefore, the most effective method is an ECG. In a variant form of angina pectoris attack, the ST segment rises and returns to the isometric line only after pain is eliminated. Holter monitoring and ECG with physical activity are performed.
New-onset angina pectoris
It is possible to recognize new-onset angina pectoris using an electrocardiogram mainly at the time of an angina attack. There is a displacement of the segmental portion of the ST (can rise or fall above/below the isoline) and deformation of the T wave (positive or negative phase, increased or decreased amplitude). Rhythm and conduction disturbances are also observed.
Progressive angina pectoris
Signs of progressive exertional angina:
- negative direction of the T and U waves;
- increase in Q waves;
- ST segment depression.
Spontaneous angina (Prinzmetal angina)
It manifests itself on the ECG as a rise in the ST segment, which turns into a positive T wave. The curve is monophasic. The opposite wall of the heart muscle has changes of a reciprocal nature.
Microvascular
An electrocardiogram for microvascular angina reveals a slight decrease in the R-ST segment and a nonspecific change in the T wave.
Localization of the area of ischemia on the ECG
The endocardium (inner layer) is most susceptible to oxygen deficiency, since the blood flow into it is much worse than into the epicardium, as a result of which it receives significantly greater blood pressure, which fills the ventricles.
ECG results may vary significantly depending on the volume and location of damaged cardiomyocytes. Oxygen starvation of the myocardium is often indicated by changes in the ST segment; for example, this may consist of depression more than 0.5 mm deep in two or three adjacent leads. Such depression can be horizontal or downward.
ECG changes in coronary artery disease can be directly related to the site of ischemia. In this case it is observed:
- damage to the anterior wall of the left ventricle in the endocardial area, which is characterized by a high T wave and its sharp end, which is distinguished by visible symmetry;
- hypoxia of the anterior part of the left ventricle with damage to the transmural form of myocardial tissue, which is one of the most dangerous types of oxygen starvation, in which a smoothed down T wave is observed;
- subendocardial ischemia, which is localized near the endocardium of the posterior part of the left ventricle; in this version of the ECG, the T wave will be almost flat and reduced;
- subepicardial ischemic disorders on the ECG at the anterior wall of the left ventricle are indicated by a negative T wave with a sharp apex;
- lesions of the posterior part of the left ventricle of the transmural type are characterized by a high positive T wave with a sharp apex placed symmetrically.
ST segment elevation in ischemic heart disease
ST segment elevation is associated with transmural or subepicardial ischemia.
Look at Chart 4, which shows two typical types of ST elevation: concave and convex. IHD is characterized by convex elevation.
Diagram 4. Concave and convex ST elevation
Schema source.
In coronary artery disease, ST segment elevation can occur with a heart attack with ST elevation, with Prinzmetal's angina, as well as with post-infarction ventricular aneurysm.
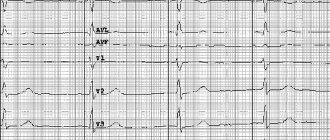
ECG 4 shows an example of ST elevation in leads I, aVL, V2-V6, indicating myocardial infarction in the region of the anterior and lateral walls of the left ventricle. In addition to elevation, the cardiogram shows ST depression in the inferior leads (III, aVF). These are reciprocal (i.e., mirror) changes, reflecting the same process as ST elevation in I, aVL, V2-V6, but in leads located on the other side of the infarction area. In general, if the cardiogram shows ST depression, characteristic of ischemia, in a large number of leads, then this indicates subendocardial ischemia. And if such depression is recorded in a limited number of leads, as in ECG 4, then these are, as a rule, reciprocal changes associated with ST elevation infarction.
In addition, ECG 4 recorded pathological Q waves (in this case, QS complexes) in leads V2-V4. Pathological Q is a sign of necrosis.
ECG 4. Increased ST segment during myocardial infarction
ECG source.
Severe tachycardia
When an oblique ST segment is observed on the image, this can be characterized by the presence of severe tachycardia in the patient. In such a case, after eliminating the stress factor and tachycardia, the results of the electrocardiogram, as a rule, show normal. If the patient was able to undergo an electrocardiographic examination during a heart attack in the acute stage, then the image can visualize depression of the ST segment of an obliquely ascending type, turning into “coronary waves” of T, which are characterized by a significant amplitude.
ECG interpretation for ischemic heart disease should be carried out by a qualified specialist.
Treatment
The entire course of treatment for coronary heart disease is based on several principles.
These include:
- Regular cardio training (walking, swimming, gymnastics). The amount and duration of training should be determined by a doctor.
- Special diet. A patient suffering from coronary heart disease should not eat salty or fatty foods.
- Emotional peace.
Also, the patient’s condition can be maintained through the use of pharmacological drugs.
Signs of ischemia on the ECG depending on the type of disease
The severity of myocardial oxygen starvation on the ECG depends largely on the severity and type of coronary heart disease. In cases of mild hypoxia of the heart muscle, this phenomenon can be detected exclusively during physical activity, when clinical symptoms are not significantly expressed.
Examples of ECG depending on the complexity of the pathological process:
- If the patient has mild ischemia, which occurs only during physical activity, the test result will be normal at rest. With the onset of an attack during training, ST segment depression will be observed in lead D, indicating true ischemia. At the same time, in leads A and I, the amplitude of the T wave may increase, which indicates the normal course of the repolarization process. At approximately 10 minutes of rest in lead D, ST depression persists and a deepening of the T wave is noted, which is a direct sign of myocardial hypoxia.
- With stable angina, attacks of pain may occur after just 15 minutes of walking. At rest, the ECG of such patients is normal in most situations. After mild exercise, downward-sloping ST depression will be noticed in certain precordial leads (V4-V6), and the T wave will be negative in three standard leads. The heart of such a patient quickly reacts to the load, and disturbances become noticeable almost immediately. What other forms of IHD are there?
- Unstable angina provokes a high risk of a heart attack and, as a rule, is clearly visible on the cardiogram. In the presence of hypoxic disorders during ischemia, the following changes develop in the anterolateral part of the left ventricle: oblique depression of the ST segment and a negative T wave in aVL, I, V2-V6. Often single extrasystoles are noted on the ECG.
- Small focal infarction resembles angina pectoris and often goes unnoticed, and a specific troponin test and careful study of ECG results help diagnose non-Q infarction. Necrotic lesions of the heart muscle are indicated by ST depression in leads V4-V5 and in V2-V6 - a negative T wave with an amplitude in the fourth lead.
It is clear that ECG results for ischemic heart disease vary depending on the type of pathology.
Methods of conducting
Physical stress test
Stress testing allows you to evaluate the effectiveness of treatment and determine the risks of myocardial infarction. The tests are based on a gradual increase in physical activity, which increases the myocardial oxygen demand. The frequency and regularity of contractions of the heart muscle is recorded. At the same time, blood pressure is constantly measured.
It is prohibited to carry out physical exercise methods in case of unstable angina.
Physical stress tests are divided into the following types:
- Master-Oppenheimer test (dosed physical activity is used). To carry out the procedure, the patient must go up and down the steps for 2-3 minutes.
- Bicycle ergometry involves the use of an exercise bike, which clearly records disturbances in the functionality of the myocardium. This is specialized equipment that has load settings.
- Static samples . The patient must hold objects with his lower limbs and clench and unclench his hands.
- Treadmill involves the use of an electric motor treadmill.
Psycho-emotional test
In many cases, medicine takes into account not only the physical condition of the patient, but also the psycho-emotional one, since the sympathetic nervous system directly affects angina attacks. The psycho-emotional test includes computer manipulation, the ability to remember numbers in a certain order, count silently, and the like.
At the beginning of testing, an ECG is done, after which the test is performed, and an electrocardiogram is performed again. The diagnosis is established after comparing the ECG results.
Electrical pacing
Electrocardiostimulation is carried out to provoke paroxysmal ischemic heart disease. During the procedure, electrodes are inserted into the heart cavity or esophagus through a catheter, thereby influencing the electrical activity of the myocardium.
Hyperventilation test
This technique is necessary for diagnosing the vasospastic type of angina. The procedure involves preliminary recording of an electrocardiogram, hyperventilation and repeated ECG.
The patient is placed on his back and asked to take 30 deep and frequent breaths in 30 seconds. Thanks to such actions, the level of carbon dioxide and potassium in the blood fluid decreases, the concentration of oxygen increases, that is, hypocapnia or alkalosis occurs.
Pharmacological tests
Pharmacology involves the use of drugs that are injected into the veins. The active ingredients of medications contribute to certain reactions that occur with angina pectoris.
Cold testing
A cold study makes it possible to identify the tendency of the coronary vessels to a spastic reaction. Cold affects the nerve endings of the skin. To do this, the patient must immerse his upper limbs in ice water.
Other techniques
Not only electrocardiography can detect an angina attack. In parallel with it, the following methods are used:
- Holter monitoring throughout the day . Electrode sensors are installed on the patient, which record all changes and heartbeat readings. In this case, the patient must lead a normal lifestyle - rest, sleep, exercise, eat food, etc.
- Ultrasound of the myocardium and coronary vessels . The location of the lesion, the cause of the impaired blood supply, and the condition of the walls of the circulatory system are identified.
- Coronary angiography detects narrowed areas in the vessels and identifies the cause of angina.
- Scintigraphy using a radioactive substance - waist. The location of the impaired blood circulation is determined.
- X-rays indicate the causes of angina attacks - the presence of blood clots, hypertrophy of the heart muscle, etc.
- It is necessary to donate blood for general and biochemical analysis.
Indications for EGC in patients with ischemic heart disease
Indications for diagnosis are characteristic symptoms observed at different stages of pathology development. And this symptomatology looks like this:
- Blood pressure, blood sugar and cholesterol levels are increased.
- Persistent exertional angina develops (periodic manifestations of pain syndromes in the chest, which intensify with stress and physical exertion).
- Complications arise in the form of pulmonary edema or cardiac asthma.
- Chronic fatigue appears even without exercise.
- Swelling appears in the lower leg area.
- Sudden attacks of dizziness, causing nausea and vomiting.
- Consciousness is clouded: a panicky feeling of fear and anxiety appears.
- There is increased sweating.
Symptoms of IHD
If visual diagnostics show that the patient has the listed symptoms, the doctor will immediately send him for an ECG in order to confirm the correctness of the diagnosis.
Changes in the T wave during ischemia
When myocardial ischemia develops, all bioelectric processes slow down significantly. This is due to the fact that potassium leaves the cells. But no changes are recorded in the myocardium itself. Doctors say that ischemia most often occurs in the endocardium, since its cells are much less well supplied with blood. The repolarization process slows down, which is recorded on the ECG in the form of a normal, but slightly expanded T wave.
The normal T wave amplitude is 1/10 to 1/8 the height of the R wave amplitude. But it will vary depending on where the ischemia is located. If the anterior wall of the left ventricle is damaged, the tooth will be high and symmetrical, the sharp end will be positive (directed upward from the axis). When ischemia occurs in the epicardium of the anterior wall of the left ventricle, the T wave is negative. It is also symmetrical and has a sharp apex. It will have the same appearance if damage occurs in the epicardial zone, with transmutal ischemia of the anterior wall of the left ventricle, or myocardial infarction.
If the electrode is placed in the peripheral zone from transmutal ischemia, the T wave will appear biphasic and smoothed. Subendocardial ischemia will also appear if it is localized on the wall opposite the fixed electrode.
It is important to remember that all changes in the T wave do not clearly confirm the presence of ischemia. They can be observed in its absence, which will indicate other disturbances in the functioning of the heart.
) lies stenosis of the coronary arteries, which develops as a result of their damage by atherosclerosis. With chronic, mildly expressed stenosis, patients at rest usually do not complain.
If stenosis
reaches 50% of the artery lumen or more, symptoms of angina pectoris appear due to a discrepancy between the myocardial need for oxygen and its delivery with the coronary blood flow; At first, symptoms appear only during physical activity (stable angina), and later, as the stenosis progresses, also at rest (unstable angina).
, myocardial infarction develops when a coronary artery is blocked.
(MI) and, possibly, sudden death (unstable angina and MI are combined into the concept of “acute coronary syndrome”).
In the pathogenesis of coronary stenosis
An important role is played by damage to the endothelium of the coronary arteries under the influence of various cardiovascular risk factors. Macrophages, consuming lipid deposits in the intima of the artery, turn into foam cells, which participate in the formation of early atherosclerotic changes.
Subsequently, a fibrofatty plaque forms
, and then a fibromuscular plaque, which narrows the lumen of the artery. As a result of intimal tears and rupture of the plaque, as well as hemorrhage into it and thrombus formation, partial or complete blockage of its lumen occurs. Clinically, plaque hemorrhage and coronary artery thrombosis manifest as ACS.
From cardiovascular risk factors
that contribute to arterial stenosis, the following should be noted: Age Hypertension High levels of low-density lipoprotein cholesterol and low levels of high-density lipoprotein cholesterol Elevated levels of triglycerides Smoking Metabolic syndrome Diabetes mellitus Genetic predisposition Physical inactivity Psycho-emotional stress
Risk of coronary artery disease
increases if several risk factors are present simultaneously. The process of stenosis of the coronary arteries can be slowed or even stopped through lifestyle changes (for example, stopping smoking, correcting excess body weight), improving diet (limiting the intake of saturated fat), and prescribing drug therapy (for example, statins - drugs that block cholesterol synthesis) .
Under IHD
Currently, a number of coronary syndromes are understood, differing in the severity of clinical manifestations. The vast field of cardiology deals with the treatment of patients with coronary artery disease. IHD is primarily divided into acute and chronic forms. Chronic ischemic heart disease, or ischemic heart disease in the narrow sense of the term, refers to stable angina. The acute form of IHD is designated as ACS.
Further articles on the site will discuss individual coronary syndromes
and their characteristic ECG changes, and in some cases, depending on the coronary syndrome, the clinical picture is discussed in more detail.
Educational video ECG for angina and types of ST segment depression
You can download this video and view it from another video hosting on the page: .
An electrocardiogram (ECG) is the result of recording the work of the heart muscle using a special device, expressed in graphical form. During this procedure, the difference in electrical potential that occurs during the functioning of the heart muscle is recorded and recorded. At the moment, this is the most common method for diagnosing pathologies of the heart and blood vessels.
The study reveals signs of coronary heart disease (CHD). Among them are left ventricular hypertrophy and other forms of the disease.
The signs characterizing IHD directly depend on the type of disease. In addition, in some cases it is asymptomatic. This can complicate the diagnostic process.
The following signs are distinguished:
- pressing pain that intensifies due to stress or physical activity;
- the appearance of shortness of breath even after minor exertion;
- heart rhythm disturbances;
- general weakness, fatigue;
- swelling of the legs;
- sudden fear of death.
An ECG for coronary heart disease allows you to assess the location, distribution and depth of disorders in the myocardium.
An ECG for ischemic heart disease, depending on the form, contains the following data:
- The appearance on a graphical reflection of coronary teeth with sharp ends, characterized by symmetry and significant amplitude. This is due to insufficient blood supply and hypoxia of cardiac tissue. As a result, the rate of repolarization of organ cells decreases. Depending on the location of the area affected by coronary artery disease, coronary waves can be either positive or negative.
- Signs of ischemia on the ECG, expressed in T-waves with further displacement of the ST segment for 15–30 minutes, occur with acute myocardial infarction. However, in some cases they indicate the development of other diseases (alcoholic cardiomyopathy, vagotonia, etc.).
- Signs of ischemic heart disease on the ECG, reflected in the form of a shift of the ST segment above or below the isoline, are recorded during ischemic damage. In this case, a deviation of less than or equal to 0.5 millimeters is within the normal range.
- In case of ischemic damage, a characteristic sign on the ECG is the occurrence of the phenomenon of reverse changes. The first signs of coronary heart disease with subepicardial damage, according to the readings of the electrodes located above the affected area, are ST segment elevation. Electrodes recording readings from the opposite side of the heart muscle will determine the depression of this segment.
- The ECG conclusion for coronary artery disease, indicating myocardial infarction, is based on identifying Q waves that have values above normal. A gradual increase in the amplitude of the R waves is also detected.
These are not all the signs that can be read from an electrocardiogram. However, a detailed assessment of the research data must be entrusted to a specialist.
Signs of ischemia on the ECG
How does ischemia occur?
Coronary heart disease (CHD) occurs due to impaired blood flow in the myocardium. To determine all the signs of the disease and make an accurate diagnosis, a diagnostic method such as an electrocardiogram is used. Myocardial ischemia is clearly visible on the ECG, which allows for a timely diagnosis.
The danger of developing ischemia lies in its suddenness. Therefore, it can cause death. Most often, men suffer from coronary artery disease. This is due to the fact that the female body produces special hormones that can prevent the development of atherosclerosis. But the onset of menopause completely changes the hormonal picture. Therefore, the development of coronary disease is most common in older women and men.
Doctors call five forms of coronary heart disease, each of which can be detected using an electrocardiogram:
- No pain syndrome. This form is often called “mute”. Symptoms may be absent due to a high pain threshold.
- Heart failure. Death occurs due to sudden cardiac arrest. The cause of a heart attack in this case is often ventricular fibrillation. There are two possible scenarios: successful resuscitation of the patient or death.
- Angina pectoris. Accompanied by severe pressing pain in the chest area. Often this form of the disease is provoked by strong emotional experiences or physical stress.
- Myocardial infarction. Characterized by stopping the blood supply to the heart. Cells are deprived of oxygen and nutrients and eventually begin to die.
Cardiosclerosis. The disease develops over a long period of time, and scars from dead cells begin to form on the heart. Manifestations of hypertrophy of individual areas of cardiac tissue lead to disruption of the normal number of myocardial contractions.
The main cause of the disease is oxygen starvation of the body. Oxygen stops flowing through the blood vessels, as a result, cell nutrition is reduced. All this together disrupts the normal functioning of the heart. A harbinger of ischemia is atherosclerosis of blood vessels. The lumens of blood vessels begin to narrow, and cholesterol plaques form more and more often.