A large number of medical patients come across the term “reference value”, and many are confused by it.
Scary pictures immediately appear in your head, thoughts appear that everything is bad and something urgently needs to be done about your health.
But in reality, everything is completely different; treating doctors have long stopped using the word “normal” and replaced it with another that is more suitable and fully describes the essence of the situation.
That is why all values within the normal range began to be called reference or otherwise reference.
Indications for analysis
Medical workers, employees of cosmetology and dermatology offices, and food workers are required to donate blood for RV. Other indications for a specific test are:
- pregnancy planning;
- preparation for operations;
- unprotected sex (especially with a new partner);
- suspicion of sexually transmitted infections;
- blood or sperm donation;
- the appearance of an incomprehensible rash on the mucous membranes and skin, discharge from the genitals, disruption of the menstrual cycle in women;
- visible enlargement of lymph nodes (especially in the groin area).
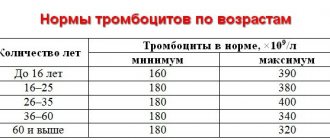
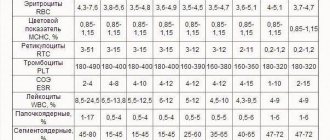
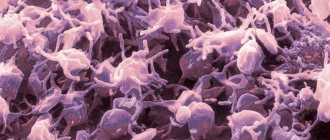
Platelets
(TC)
– the most important element of blood clotting. They store the protein thromboplastin in themselves and, if necessary to urgently stop bleeding, they explode and throw it into the blood. A lack of TC indicates a possible increased bleeding, a threat of bleeding, an excess indicates a tendency to thrombosis. Both are bad. The norm ranges from 180 thousand to 320 thousand. The number of TC in the analysis strongly depends on the state in which the person took the test - nervous, smoked before donating blood, or took alcohol the day before. A deviation from the norm of 10% is acceptable.
Preparation
Before the analysis, the use of any medications is prohibited. Coffee, tea, alcohol and juices cannot be drunk at least 12 hours in advance, only water is allowed. If you need to take a vital drug, notify the laboratory technician. Antibiotics should be stopped one week before the test. The day before the test, it is better to exclude fatty, smoked, pickled, flour and spicy foods.
The nontreponemal test has a fairly high probability of obtaining a false negative test result. Therefore, before carrying out it, it is important to prepare properly. You can get tested for biochemistry and ORS on an empty stomach, and for a few days you can avoid eating fried, fatty foods, as well as alcohol.
Laboratory studies are a group of diagnostic methods based on biochemical and biological methods for determining abnormalities in the composition of the patient’s tissues and biological fluids.
General clinical laboratory tests;
Biochemical blood test;
Determination of antibodies to viral infections (ELISA);
Determination of infection Enzyme-linked immunosorbent assay (ELISA);
Taking tests to determine avidity;
Taking tests to determine the Varicella Zoster virus (VZV);
Taking tests for tumor markers;
Testing for hepatitis markers;
Taking tests to determine antibodies using ELISA (HIV, ORS, RW);
Taking tests to determine the immune status of the body (immunological examination);
Testing stool for occult blood (scraping, bacteriological examination, etc.);
Microbiological studies: cultures;
PCR diagnosis of bacterial infections (polymerase chain reaction method);
Histological examinations (histology, cytology, flora smear, spermogram, etc.)
You can find a complete list of laboratory tests in the adult department at the link: Laboratory tests for adults, prices
You can find a complete list of laboratory tests in the adult department at the link: Laboratory tests for children, prices
Other factors influencing research results
Laboratories usually report your test results using reference values for your age and gender. Your doctor then interprets the results for you based on his personal knowledge of your health and the drug therapy you are using. It is necessary to take into account that the results of the study may be influenced by many additional factors: consumption of coffee, tobacco, alcohol, vitamins, natural and artificial dyes, etc.; your diet (for example, vegetarian or meat), stress or pregnancy. Even your posture when the biomaterial is taken from you can affect some of the results, as well as the physical activity preceding the test.
When is it carried out?
ORS is prescribed to medical specialists for several indications:
- Admission to a medical hospital or an appointment with a specialist from a polyclinic institution, regardless of the profile.
- Preparation for surgical intervention, performance of invasive diagnostic procedures, as well as before therapeutic and surgical dental treatment by a dentist.
- Periodic screening study in people of certain professions (medical workers, kindergarten teachers, employees of public catering establishments).
- Preventive examination of couples when planning pregnancy, as well as in the early stages of its course.
Also, the analysis can be carried out at the request of a person in special anonymous examination rooms for the purpose of diagnosing infectious diseases characterized by sexual transmission.
Qualitative and quantitative characteristics
A qualitative characteristic is simply indicated by the words positive or negative result shown by the analysis. Quantitative characteristics are used more often, and this is information for the doctor, who, based on the obtained figures, can determine how serious deviations in the patient’s condition there are, if they are compared with what is indicated on the form as reference values. Decoding the data is usually the responsibility of a specialized specialist who knows what changes the numbers indicate. For many diseases, there are certain components of the diagnostic search, which are identified in each person using laboratory tests. If a doctor needs an exact answer in numbers, he receives quantitative characteristics on a standard form.
Don’t be shy, ask our consultants questions, right here on the website. We will definitely answer. Leave commentsGo
RW blood test: explanation, how to take it and what is it?
The results form includes pluses or minuses. The latter speak of a negative reaction and absence of illness. A positive reaction can be described with one to four plus signs. The transcript shows the stage of the disease:
- or – positive test;
- – weakly positive;
- – doubtful, requires double-checking.
If the RW analysis shows a negative result, this does not exclude that a person has syphilis at the first or third stage. Plus, a negative reaction may indicate the destruction of red blood cells. The secondary period of syphilis does not always show a positive result. In the first 17 days, the reaction can be negative, and only by the sixth week can it show, and even then only in 25% of patients with syphilis. After this, the reliability approaches 80%. Approximately 5% of healthy people show a false positive result.
If the test for RV is positive, this indicates the presence of antibodies to Treponema pallidum in the blood - that is, about 1.5 months have passed since the infection. Other reasons for results to appear on the form are:
- carrying out antisyphilitic therapeutic measures - reducing the acute process;
- pregnancy in the absence of the disease itself - the analysis will be weakly positive in approximately 1.5% of women;
- primary syphilis – 80% of cases at 6-8 weeks;
- secondary syphilis in 100% of cases;
- clinical relapse of the disease;
- tertiary period of the disease - in 75% of cases;
- early congenital syphilis.
RW negative
If you receive a negative test result, you can talk about the absence of infection and antibodies to syphilis in the body, but this is not always the case. In the early stages of the disease, the results will be negative because antibodies simply do not have time to develop. Plus, certain diseases and individual characteristics of patients influence the reliability failure.
Syphilis is the most famous and common infection that is transmitted through close contact of a patient with a healthy person. Very often, syphilis is transmitted through sexual contact, however, household infections also occur.
Transmission of syphilis
The likelihood of a pregnant woman infecting her child intrauterinely is very high. Most often, infection occurs during the secondary and primary periods of the disease. The tertiary period is not contagious.
The main symptoms of syphilis:
- erosion of oval forms (localized in areas where the pathogen is introduced, i.e. Treponema pallidum);
- syphilides;
- regional increase in the volume of lymph nodes.
The patient must undergo a test for RW to make an accurate diagnosis and prescribe a treatment regimen.
How is it determined
To determine the reference interval, the limits of reference values are taken - the largest and smallest indicators included in the relative state of health. If the data obtained for an individual patient falls within the interval between the largest or smallest value, his body is in a state of relative health. To make sure that there is a disease in the body, if the data obtained during the analysis are not included in the reference interval, a repeat test is often prescribed. Indicators in individual studies may change in one direction or another, under the influence of various factors.
The reference interval on the analysis data is determined by conducting research on the target audience (for example, healthy middle-aged men, or people of both sexes who do not have diseases). The upper and lower thresholds are those small numbers (usually 50 people out of a thousand) with the highest and lowest scores. The remaining values will be between these limits. The reference interval takes as the norm the data obtained in 95% of cases.
False positive reaction
In 5% of patients, a false positive reaction is observed - a condition when the analysis shows, but the patient is not sick. The reasons for a false positive manifestation are:
- tuberculosis, systemic lupus erythematosus, leukemia, leprosy, leptospirosis, cancer, typhus, scarlet fever, HIV and AIDS;
- beriberi and sleeping sickness, hepatitis;
- in pregnant women or those who have just given birth;
- during menstruation;
- after anesthesia, consumption of alcohol, drugs, fatty foods, coffee, cigarettes, medications, administration of certain serums or vaccination;
- acute infections in pregnant women.
Related and recommended questions
If the data obtained shows or, a secondary blood sample is also necessary. Sometimes ORS (disease selection response) is used. To do this, blood serum is applied to a glass slide and a cardiolipid antigen is added. If the repeated result is positive, a visit to a venereologist is required to make an accurate diagnosis.
To prevent congenital syphilis in children, pregnant women donate blood for RW during all nine months: this test is one of the mandatory procedures for expectant mothers. If a pregnant woman becomes infected, comprehensive treatment is necessary during the first months. If treatment is neglected, the consequences are dangerous for both the mother and the unborn child.
Analysis for syphilis is one of the most popular studies in venereology. There are several different methods that have one thing in common - the general material selected for diagnosis. This is blood. It is the presence of the pathogen in the human circulatory system that is a mandatory diagnostic marker for making a diagnosis of Syphilis, since the presence of a clinical picture is not always sufficient for this.
Decoding the diagnosis without laboratory testing is sometimes difficult, since the course of the disease is characterized by periods of complete absence of its obvious manifestations. Syphilis is caused by Treponema pallidum, a gram-negative spirochete, entering the human body. This is a spiral-like microorganism. Due to its complete immunity to any aniline dyes used for staining in bacteriology, the pathogen was called treponema pallidum.
The main mechanism of transmission is sexual, but due to the ability of the spirochete outside the host body to maintain viability and virulence for about four days, contact and household transmission is also possible. During pregnancy, the pathogen is freely transmitted from mother to child, therefore, the placental barrier is not a hindrance for it.
The average incubation period is about 3 weeks. After this, the first characteristic sign of a developing sexually transmitted infection appears - chancre. These are erosions that form on the surface of the skin or mucous membranes, that is, in the place where the pathogen was introduced.
The ulcer is usually small, painless, with slight serous discharge. It can last up to one and a half months on average, and then disappears. This is followed by a period of two months, which is characterized by a complete absence of symptoms. At this time, a diagnosis can only be made if tested for syphilis.
Later, symptoms appear that are called “Secondary syphilis.” This is a general intoxication with increased body temperature, weakness and characteristic rashes. They also disappear after some time, and the disease enters the so-called latent period, which is characterized by the periodic appearance of secondary symptoms of the disease, and then their complete absence.
In the absence of proper treatment, syphilitic damage to internal organs occurs, that is, the disease develops into a tertiary form of infection. Patients with this disease are dangerous to others at any stage of the infectious process, and due to the presence of stages of asymptomatic carriage of the pathogen, it can only be detected by testing for syphilis.
What is amylase?
Amylases (alpha-amylase) are a group of enzymes that serve to break down complex carbohydrates; Inside the pancreas, which is an exocrine gland, the enzyme is synthesized by acinar cells and then passes through the pancreatic ducts and reaches the digestive tract.
Amylases are also produced by the salivary glands, small intestinal mucosa, ovaries, placenta and liver. Pancreatic and salivary isoenzymes are detected in the blood at high concentrations by examination.
Under normal conditions, amylase is present in small amounts in the blood and urine, however, when the cells of the pancreas have some problem, such as pancreatitis or when the pancreas is blocked by a stone, or in rare cases by a tumor, the enzymes enter the blood circulation more easily, so their concentration increases as in blood and in urine (amylase leaves the body through urine).
Amylase testing is often used by doctors to diagnose pancreatitis. Pancreatic amylase (amylase P isoenzyme) testing is most useful for laboratory diagnosis of acute pancreatitis .
Total serum (blood) is still the most widely used method for diagnosing acute pancreatitis and is accurate to 95% (accuracy of a diagnostic test refers to its ability to provide true values).